
Thrombosis is a serious condition where a blood clot blocks blood flow in a vessel. This can cause heart attacks, strokes, or pulmonary embolism. The US Department of Health and Human Services says it can lead to serious illness, disability, or even death.
We will look at the risk factors for thrombosis, blood clots. These include genetics, lifestyle, and medical conditions. Knowing these helps prevent and manage the condition. By understanding the main risks, we can lower the chance of getting thrombosis.
Key Takeaways
- Thrombosis occurs when a blood clot forms inside a blood vessel.
- Risk factors include genetic predisposition, lifestyle choices, and medical conditions.
- Understanding these factors is key for prevention and management.
- Serious complications can arise if left untreated, including heart attack and stroke.
- Identifying main risk factors can help mitigate the risk of developing thrombosis.
Understanding Thrombosis: The Formation of Blood Clots
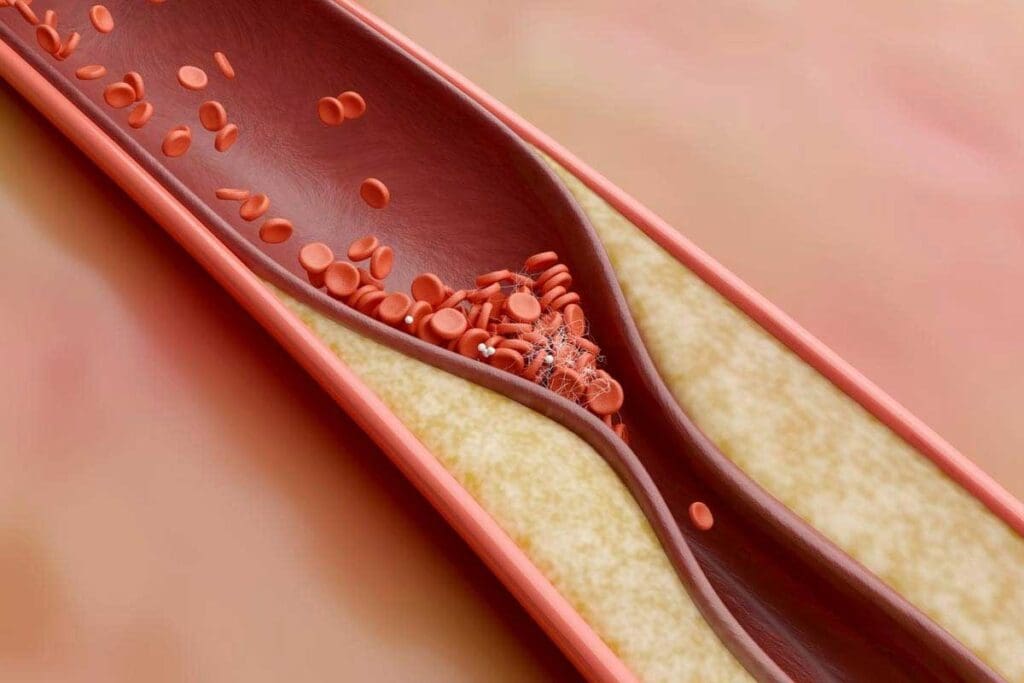
We will explore thrombosis, a condition where blood clots form inside blood vessels. This blocks normal blood flow. Thrombosis is a serious condition that can lead to venous thromboembolism (VTE). VTE includes deep vein thrombosis (DVT) and pulmonary embolism (PE).
Definition and Medical Terminology
Thrombosis is when a blood clot, or thrombus, forms in a blood vessel. This clot can block blood flow, leading to tissue damage or serious health issues. Terms like thrombiosis and thromosis describe this clotting process in vessels.
The medical field uses specific terms for thrombosis and related conditions. For example, thrombophlebitis is inflammation of a vein due to a blood clot. Knowing these terms is key for diagnosing and treating thrombosis.
Common Types of Thrombosis and Thrombiosis
There are several types of thrombosis, each with its own characteristics and implications. Deep Vein Thrombosis (DVT) happens when a blood clot forms in a deep vein, usually in the legs. If the clot breaks loose, it can travel to the lungs, causing a pulmonary embolism (PE), a serious condition.
- DVT is often linked to prolonged immobility, like during long flights or after surgery.
- PE can cause sudden symptoms like chest pain and shortness of breath.
- Arterial thrombosis occurs when a clot forms in an artery, potentially leading to a heart attack or stroke.
Knowing the different types of thrombosis is key for proper management and treatment. We will look at causes and risk factors in the next sections.
What Causes Thrombosis: Exploring Virchow’s Triad
Blood clots form due to three main reasons, as stated by Virchow’s triad. This idea, by Rudolf Virchow, is key to understanding blood clotting. The triad includes damage to blood vessel walls, abnormal blood flow, and blood that clots too easily.
Damage to Blood Vessel Walls
Damage to the inner lining of blood vessels is a big factor in blood clots. This damage can come from physical trauma, infection, or inflammation. When the inner lining is hurt, it starts a chain reaction that leads to clotting.
Medical procedures or diseases like vasculitis can cause this damage. It not only starts clotting but also weakens the blood vessel’s ability to prevent clots.
Abnormal Blood Flow Patterns
Unusual blood flow, whether it’s turbulent or static, raises the risk of blood clots. Turbulent flow can harm the blood vessel lining, while slow flow lets clotting factors build up.
Things like heart problems, aneurysms, or narrowed blood vessels can cause abnormal flow. For example, irregular heartbeats in atrial fibrillation can lead to blood clotting in the heart.
Hypercoagulability of Blood
Hypercoagulability means the blood clots too easily. This can be due to genetic factors, like Factor V Leiden, or acquired conditions, such as cancer. It’s also caused by certain medications, like hormonal therapies.
This condition makes blood clotting more likely. It’s important to find people with this condition to prevent and manage blood clots.
Venous vs. Arterial Thrombosis: Key Differences
It’s key to know the differences between venous and arterial thrombosis for proper diagnosis and treatment. Thrombosis can happen in veins and arteries, each with its own set of issues and outcomes.
Deep Vein Thrombosis (DVT) and Thrombosis
Deep Vein Thrombosis (DVT) is a venous thrombosis that forms in deep veins, usually in the lower leg, thigh, or pelvis. It’s serious because if the clot breaks loose, it can go to the lungs and cause a pulmonary embolism.
Risk factors for DVT include:
- Prolonged immobility
- Surgery or trauma
- Cancer and its treatment
- Genetic predisposition to clotting
Arterial Blood Clots and Thrombosis Blood Clots
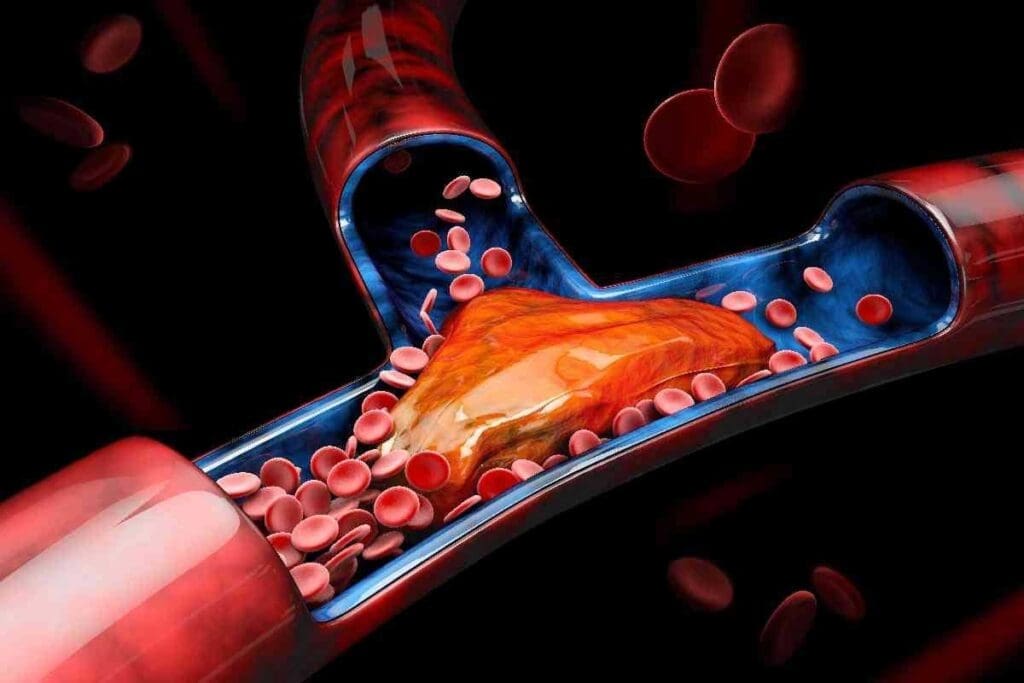
Arterial thrombosis happens when a blood clot forms in an artery. This can lead to heart attacks or strokes. Arterial blood clots usually start when an atherosclerotic plaque ruptures, blocking an artery suddenly.
| Characteristics | Venous Thrombosis | Arterial Thrombosis |
| Location | Veins, typically deep veins | Arteries, often with atherosclerosis |
| Common Complications | Pulmonary embolism | Heart attack, stroke |
| Typical Symptoms | Swelling, pain, and warmth in the affected limb | Chest pain, sudden weakness, or paralysis |
“The distinction between venous and arterial thrombosis is not just semantic; it has significant implications for treatment and management.”
—Thrombosis Expert
Understanding these differences is vital for proper care and prevention of complications. By knowing the unique traits of each type of thrombosis, healthcare providers can offer the right treatment for each patient.
Age and Genetic Factors in Blood Clot Formation
Advanced age and inherited genetic predispositions are major factors in blood clot formation. It’s important to understand their impact on managing blood clot risk.
How Aging Affects Clotting Risk
As we age, our blood vessels lose flexibility. This makes blood clotting more likely. Older adults also face more health issues that raise thrombosis risk.
Inherited Thrombophilia and Genetic Predisposition
Inherited thrombophilia is a genetic condition that makes blood clotting more likely. It affects how blood clots and how it prevents clotting. Knowing your genetic risk can help prevent blood clots.
Let’s look at some data. The risk of deep vein thrombosis (DVT) grows with age. Genetic mutations like Factor V Leiden can raise thrombosis risk by 3- to 8-fold.
| Risk Factor | Description | Impact on Thrombosis Risk |
| Advanced Age | Physiological changes with aging | Increased risk |
| Genetic Predisposition | Inherited conditions affecting clotting factors | Increased risk |
| Factor V Leiden | Specific genetic mutation | 3- to 8-fold increase |
In conclusion, age and genetics are key in determining thrombosis risk. Understanding these factors helps in the early identification and management of thrombosis risk.
Lifestyle Risk Factors for Thrombosis
Many lifestyle choices can increase our risk of getting blood clots. By changing these habits, we can lower our chances of developing blood clots.
Obesity and Its Impact on Clotting
Being overweight is a big risk for blood clots. Extra weight, mainly around the belly, can cause more inflammation and clotting factors in our blood. This makes it easier for clots to form.
Also, obesity often goes hand in hand with other health issues like diabetes and high blood pressure. These conditions can make the risk of blood clots even higher. Keeping a healthy weight through good eating and exercise is key to reducing this risk.
Smoking and Nicotine Effects on Thrombosis Risk
Smoking is another big risk for blood clots. The chemicals in tobacco smoke harm the blood vessel lining, making them more likely to clot. Nicotine also makes blood vessels narrow, raising the risk even more.
Stopping smoking is a big step in lowering the risk of blood clots. There are many resources to help people quit, like counseling and medicine.
Sedentary Behavior and Prolonged Immobility
Being inactive and staying in one place for too long can also raise the risk of blood clots. When we’re not moving, blood flow slows down, which can lead to clotting.
Regular exercise and taking breaks to move, even during long trips, can help lower this risk. Simple moves like ankle rotations and stretching can also improve blood flow.
Knowing how our lifestyle choices affect our risk of blood clots gives us power. By tackling these changeable risks, we can take steps to lower our chance of getting blood clots.
| Lifestyle Factor | Impact on Thrombosis Risk | Mitigation Strategies |
| Obesity | Increases inflammation and clotting factors | Maintain a healthy weight through diet and exercise |
| Smoking | Damages the blood vessel lining and constricts vessels | Quit smoking with counseling and medication |
| Sedentary Behavior | Slows down blood flow | Engage in regular physical activity and take breaks to move |
Medical Conditions That Increase Risk of Thrombosis
Medical conditions greatly affect the risk of getting blood clots. Some health issues can make it more likely to develop blood clots. It’s important to know these conditions to prevent and manage thrombosis.
Cancer and Blood Clots
Cancer is a big risk factor for blood clots. The link between cancer and blood clots is complex. It involves tumor cells, inflammation, and changes in blood clotting factors.
People with cancer are more likely to get venous thromboembolism (VTE). VTE includes deep vein thrombosis (DVT) and pulmonary embolism (PE). The risk depends on the cancer type, stage, and treatment.
Cardiovascular Disease and Thrombosis
Cardiovascular disease affects the heart and blood vessels. Conditions like atherosclerosis, hypertension, and heart failure raise thrombosis risk. They damage blood vessel walls and change blood flow.
It’s key to manage cardiovascular disease to lower thrombotic events risk.
Inflammatory and Autoimmune Disorders
Inflammatory and autoimmune disorders, like rheumatoid arthritis and lupus, also raise thrombosis risk. Chronic inflammation changes blood clotting and increases clot formation. Effective management of these conditions is essential to reduce thrombotic risks.
Healthcare providers can develop specific prevention and management plans by understanding these conditions. They can closely monitor high-risk patients and use preventive measures when needed.
Medications and Treatments Associated with Thrombosis Risk
We look at how different medicines, like hormonal treatments, can raise the risk of blood clots. Some drugs can make blood clots more likely. It’s key to know these risks to handle them well.
Hormonal Therapies and Contraceptives
Hormonal treatments, like birth control pills and hormone replacement therapy (HRT), are used for many health issues and family planning. But they can also increase the risk of blood clots, mainly in women who smoke or have other risk factors. The risk is higher with estrogen-containing contraceptives, mostly in the first year of use.
People using hormonal treatments or contraceptives should know the risks. They should talk about their health and family history with their doctor. This helps in choosing the best treatment.
Other Medications That May Cause Thrombosis
Other than hormonal treatments, some medicines can also raise the risk of blood clots. This includes certain cancer treatments, like tamoxifen and thalidomide, which can increase blood clot risk. Also, some antipsychotic medications and anti-inflammatory drugs may add to this risk.
It’s important for patients to tell their doctors about all the medicines they take. This helps doctors figure out the overall risk of blood clots. Then, they can create a plan to lower these risks.
Knowing which medicines can lead to blood clots is a big step in managing this risk. By staying informed and working with doctors, people can make smart choices about their treatment.
Complications of Untreated Thrombosis
Untreated thrombosis can cause severe and life-threatening problems. A blood clot that isn’t treated can lead to serious health issues. These issues can affect a person’s life for a long time. We will look at the complications that can happen from untreated thrombosis.
Pulmonary Embolism
A pulmonary embolism happens when a blood clot travels to the lungs. It blocks blood flow there. This is a medical emergency that needs quick attention.
Stroke and Heart Attack
Thrombosis can also cause a stroke or heart attack. This happens when a clot blocks blood flow to the brain or heart. These are serious and can be life-threatening, needing immediate medical help.
Post-Thrombotic Syndrome and Long-Term Effects
Post-thrombotic syndrome (PTS) is a condition after deep vein thrombosis (DVT). It causes chronic pain, swelling, and skin discoloration. PTS can greatly affect a person’s quality of life.
| Complication | Description | Potential Consequences |
| Pulmonary Embolism | Blockage of blood flow in the lungs | Respiratory failure, death |
| Stroke | Blockage of blood flow to the brain | Brain damage, disability, death |
| Heart Attack | Blockage of blood flow to the heart | Heart damage, death |
| Post-Thrombotic Syndrome | Chronic pain, swelling, skin discoloration | Reduced quality of life, disability |
Prevention Strategies and Management of Thrombosis
Preventing thrombosis means understanding and reducing risk factors. This can be done through lifestyle changes and using anticoagulant medications. By taking a proactive approach, people can lower their risk of thrombosis and its serious complications.
Lifestyle Modifications to Reduce Thrombosis Risk
Healthy lifestyle choices are key to preventing thrombosis. Regular exercise, a healthy weight, and avoiding long periods of sitting are important. Try to include activities that improve blood flow, like walking or swimming, in your daily life.
Eating a balanced diet with fruits, vegetables, and whole grains is also beneficial. Drinking enough water is essential. Dehydration can make blood thicker and increase clotting risk.
Key Lifestyle Modifications:
- Regular exercise
- Healthy weight management
- Avoiding prolonged immobility
- Balanced diet
- Adequate hydration
Anticoagulant Medications and Treatments
For those at high risk, anticoagulant medications are vital. These drugs stop blood from clotting, reducing the chance of clots. Common ones include warfarin, apixaban, rivaroxaban, and dabigatran.
| Anticoagulant Medication | Mechanism of Action | Common Use |
| Warfarin | Inhibits vitamin K-dependent clotting factors | Long-term anticoagulation |
| Apixaban | Direct Factor Xa inhibitor | Stroke prevention in atrial fibrillation |
| Rivaroxaban | Direct Factor Xa inhibitor | Treatment and prevention of DVT and PE |
When to Consider Thrombosis Prophylaxis
Thrombosis prophylaxis is needed for those at high risk. This includes people having major surgery, those in the hospital, or those with a history of blood clots. The decision to start should be based on a thorough risk assessment and medical judgment.
It’s important to talk to a healthcare professional about the best prevention plan for you.
Conclusion: Understanding and Managing Your Risk Factors of Thrombosis
It’s key to know the risk factors and causes of thrombosis to prevent and manage it well. By spotting the factors that lead to thrombosis, we can take steps to lower our risk. This helps us manage the condition more effectively.
Preventing thrombosis starts with managing risk factors. This means making healthy lifestyle choices like keeping a healthy weight and exercising often. It also means avoiding sitting for too long. Knowing the medical conditions and medicines that raise thrombosis risk is also important.
Preventing thrombosis needs a full approach that includes being aware, making lifestyle changes, and using medical treatments. Working with healthcare experts helps us find ways to lower thrombosis risk and handle its problems.
Understanding and managing our risk factors helps cut down on thrombosis cases. This improves our health outcomes. Good prevention and management of thrombosis reduces the chance of serious issues like pulmonary embolism and stroke.
FAQ
What is thrombosis, and how does it occur?
Thrombosis happens when a blood clot blocks a blood vessel. This can cause serious problems like heart attacks, strokes, or pulmonary embolisms.
What are the main risk factors for developing thrombosis?
Risk factors include genetics, lifestyle, and medical conditions. Being older, overweight, smoking, and not moving much also increases the risk.
What is Virchow’s triad, and how does it relate to thrombosis?
Virchow’s triad explains three key factors for thrombosis: damaged blood vessels, abnormal blood flow, and blood that clots too easily. Knowing these helps find and prevent risks.
What is the difference between venous and arterial thrombosis?
Venous thrombosis, like DVT, happens in deep veins. Arterial thrombosis, which can cause heart attacks or strokes, occurs in arteries.
How do hormonal therapies and contraceptives affect the risk of thrombosis?
Hormonal treatments, like birth control and hormone therapy, can increase blood clot risk. It’s important to monitor and manage this risk.
What are the complications of untreated thrombosis?
Untreated thrombosis can lead to serious issues like pulmonary embolism, stroke, and heart attack. It can also cause long-term problems like post-thrombotic syndrome.
How can the risk of thrombosis be reduced?
To lower thrombosis risk, stay active, keep a healthy weight, and avoid sitting for too long. Anticoagulant drugs are also key for high-risk people.
What is thrombosis prophylaxis, and when should it be considered?
Thrombosis prophylaxis means taking steps to prevent blood clots. It’s important for those at high risk, like those with a clotting history or certain conditions.
How does age affect the risk of thrombosis?
Age increases the risk of thrombosis. Older people should be aware of the risks and take steps to prevent them.
What is the role of genetic factors in thrombosis?
Some genetic conditions, like inherited thrombophilia, raise the risk of blood clots. Knowing these risks helps in preventing them.
Can thrombosis be prevented?
While some risks can’t be changed, many cases of thrombosis can be prevented. This includes changing lifestyle, managing health conditions, and using anticoagulants when needed.
References:
- Kumar, D. R., Khan, S., & Pillarisetti, L. S. (2024). Virchow Triad. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK539697/
- Prandoni, P. (2009). Venous and arterial thrombosis: Two aspects of the same disease? Clinical Epidemiology, 1, 1–6. https://pmc.ncbi.nlm.nih.gov/articles/PMC2943163/




































