Last Updated on November 4, 2025 by mcelik
At Liv Hospital, we know how scary arteriovenous malformations (AVMs) can be. An AVM is a rare problem with blood vessels. It messes up how blood flows and oxygen gets to our bodies.
This issue happens when arteries and veins get tangled up. They skip over tiny blood vessels called capillaries. This can lead to big health problems.
AVMs in the brain or spine are very dangerous. They can burst, causing serious harm. We aim to give top-notch care to patients from around the world. We help those dealing with AVMs and other serious health issues.
In medical terms, AVM stands for Arteriovenous Malformation. It’s a complex vascular condition. Knowing what AVM means is key for doctors and patients. It’s a serious condition that needs quick diagnosis and treatment.
AVM is a mix-up of blood vessels. Arteries connect directly to veins, skipping capillaries. This can cause health problems, like bleeding. AVM can happen in the brain, spine, and other organs.
AVMs are complex and have weird connections between arteries and veins. The cause is often unknown. But, genetic changes or mutations during development might play a role.
Knowing about AVM is very important. Accurate diagnosis and treatment depend on understanding it well. Doctors use special imaging to find and check AVMs.
| Key Aspects of AVM | Description |
|---|---|
| Definition | Abnormal connection between arteries and veins |
| Potential Locations | Brain, spine, and other organs |
| Causes | Genetic changes or somatic mutations |
| Diagnosis | Advanced imaging techniques |
Understanding AVM is vital for diagnosis and treatment. By knowing about AVM, doctors can give the right care and advice to patients.
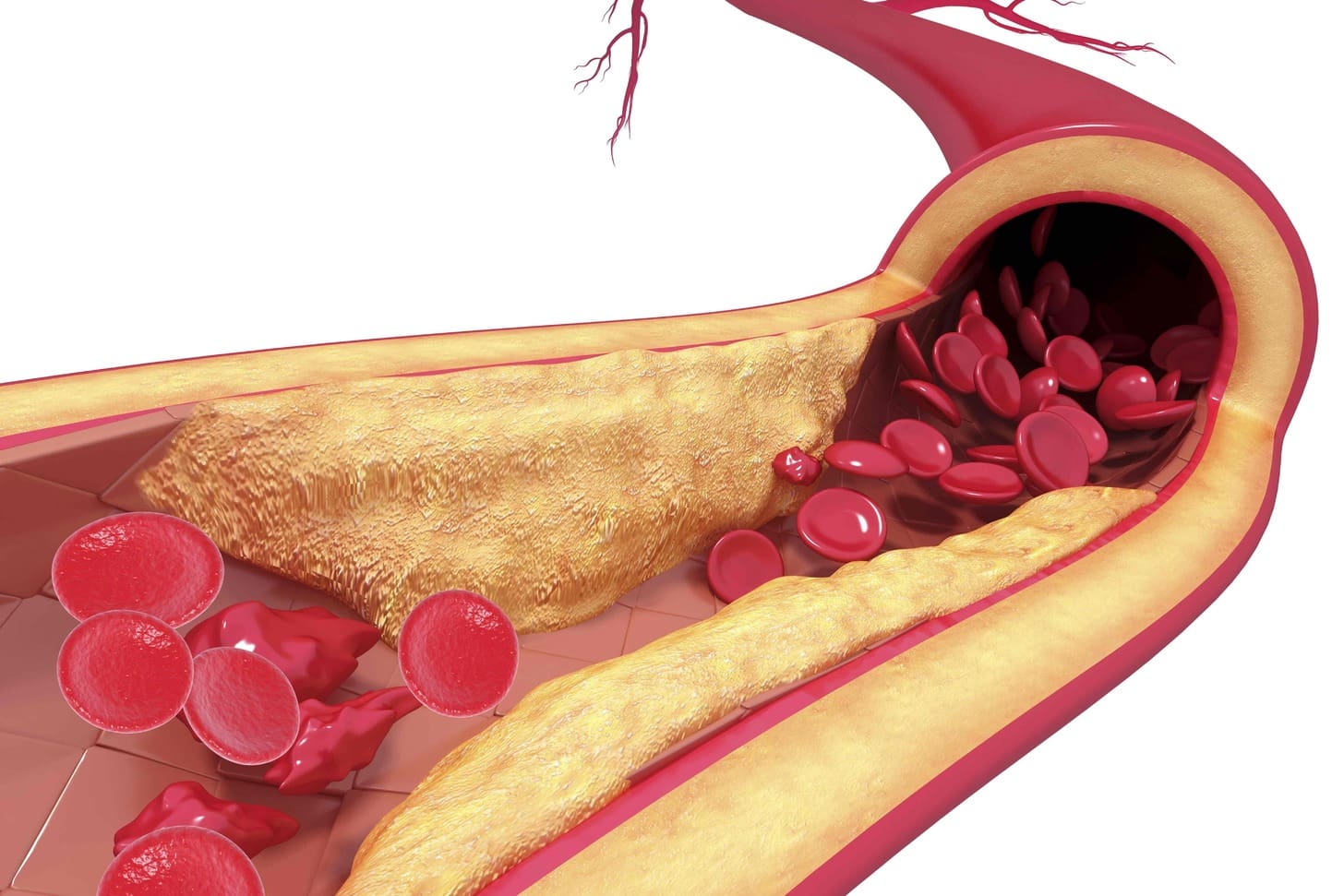
AVMs form when arteries and veins connect directly, skipping the usual capillary route. This unusual connection is key in medical terms.
Normal blood vessels ensure blood flows right and oxygen reaches tissues. Arteries carry oxygen-rich blood to capillaries for exchange. Then, veins take deoxygenated blood back to the heart. This setup is vital for tissue health.
AVMs are different because they don’t have capillaries. They have a straight path from arteries to veins. This leads to abnormal blood flow and health risks. The risk of rupture and bleeding is higher.
Without capillaries, AVMs disrupt oxygen and nutrient exchange. This can cause tissue ischemia and other issues. The risk of rupture is also higher.
Knowing how AVMs form is key to treating them. We’ll look at more about AVMs next.
Knowing where AVMs are found is key to treating them well. AVMs can pop up anywhere in the body. But, their effects change a lot based on where they are.
Brain AVMs are very serious because they can mess with important brain functions. They can lead to seizures, headaches, and even bleeding in the brain, which is very dangerous. These malformations are rare, but it’s hard to know how common they are because they often don’t show symptoms.
Spinal AVMs are less common than brain ones but are just as risky. They can cause pain, muscle weakness, and even paralysis, depending on where and how big they are. Finding spinal AVMs can be tough because they’re rare and symptoms are not always clear.
AVMs can also show up in other parts of the body, not just the brain and spine. For example:
Each place has its own set of problems and symptoms. This means doctors need to use different treatments for each one.
In short, where an AVM is located greatly affects how it’s treated. Doctors need to understand these differences to give the right care.
Scientists are studying why AVMs happen. They think genetics, developmental problems, and cell mutations might play a part. Even though we don’t know all the details, learning about these factors helps us understand AVMs better.
Genetics seem to be a big deal in AVMs. Some genetic disorders, like Hereditary Hemorrhagic Telangiectasia (HHT), raise the risk of getting AVMs. It’s thought that genes that control blood vessel growth might be involved in AVMs.
AVMs might start in the womb, when blood vessels are forming. Problems with blood vessel growth can cause arteries and veins to connect directly. This can lead to an AVM.
Somatic mutations in non-reproductive cells might also cause AVMs. These mutations can mess with genes that help blood vessels grow. Researchers are looking into how these mutations affect blood vessels.
Figuring out why AVMs happen is key to finding better treatments. By studying genetics, development, and cell changes, we can better manage AVMs.
It’s important to know the signs of an arteriovenous malformation (AVM) for early treatment. We’ll look at the symptoms that might show an AVM is present. This helps both patients and doctors spot the condition.
AVMs can affect the brain or spinal cord, leading to various symptoms. These include seizures, headaches, and muscle weakness. The symptoms depend on where the AVM is located.
For example, brain AVMs might cause trouble with speech, vision, or balance. Some people might feel tingling sensations or numbness in their body. This happens because the abnormal blood vessels can harm nearby nerves.
AVMs can also cause physical symptoms. You might see swelling or discoloration on the skin’s surface if the AVM is near it.
Some people feel pain or discomfort due to the AVM. This can happen when the malformation presses on nearby tissues or nerves. The symptoms can vary a lot from person to person.
Not all AVMs show symptoms. Asymptomatic AVMs can hide for years, posing a risk until they rupture or cause harm. Even without symptoms, an AVM can rupture and lead to serious problems.
Regular doctor visits and advanced imaging are key to finding these hidden AVMs. Finding them early lets doctors keep an eye on them or treat them before they become a big issue.
Arteriovenous malformations (AVMs) are risky because they can cause severe bleeding and harm to the brain. We will look at the dangers of AVMs. This includes the risk of bleeding, brain damage from bad blood flow, and long-term health issues.
AVMs can rupture, leading to bleeding and stroke. This can be very dangerous and even life-threatening. The rupture can cause bleeding in the brain, leading to a stroke.
The chance of bleeding from an AVM is a big worry. Studies show the annual risk is about 2-4%. Even though it’s not very high, the damage from a rupture can be severe.
AVMs can also harm the brain by changing blood flow. The abnormal connection in an AVM can divert blood from normal brain areas. This can cause seizures, weakness, and problems with thinking.
AVMs can also lead to long-term health problems. Repeated bleeding or bad blood flow can make the brain worse over time. Some people may have ongoing symptoms like headaches or seizures.
We have summarized the dangers of AVMs in the following table:
| Danger | Description | Potential Consequences |
|---|---|---|
| Hemorrhage and Bleeding | Rupture of AVM leading to bleeding into surrounding tissue | Hemorrhagic stroke, severe neurological damage, death |
| Neurological Damage | Disruption of normal blood flow causing ischemia or infarction | Seizures, weakness, cognitive impairment, neurological decline |
| Long-term Health Complications | Repeated episodes of bleeding or ischemia | Chronic symptoms (headaches, seizures), progressive neurological decline |
In conclusion, AVMs are dangerous because they can cause severe bleeding, brain damage, and long-term health problems. Knowing these risks is important for those with AVMs to make good choices about their care.
It’s important to know what causes an arteriovenous malformation (AVM) to rupture. This is because an AVM rupture can be very serious. Knowing the causes helps doctors give the right care.
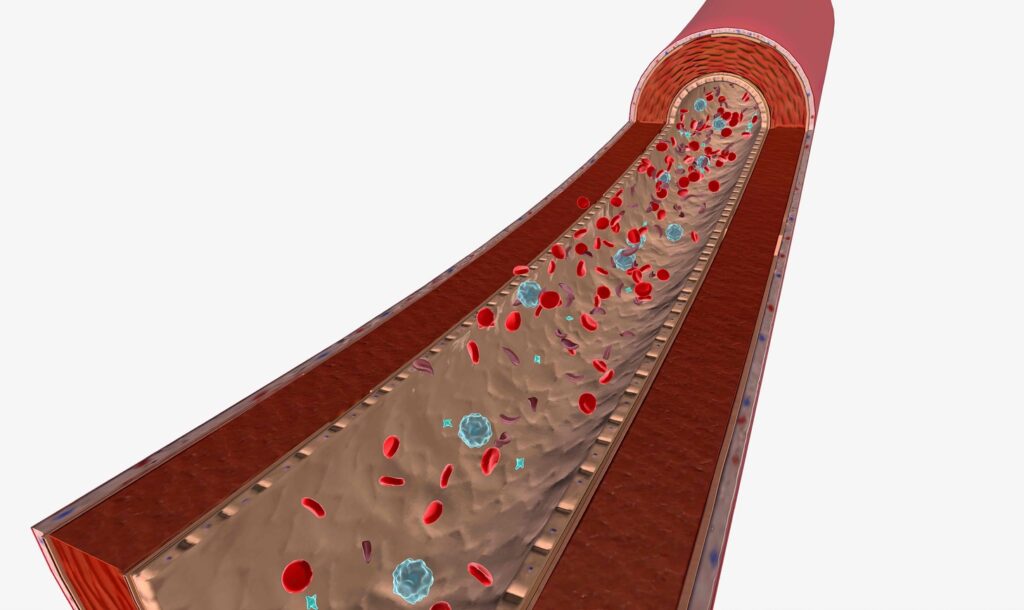
An AVM has abnormal connections between arteries and veins. This means high-pressure blood flow goes straight into veins. These veins are not built for such pressure.
Over time, the veins can get weaker. This makes it more likely for them to burst. Studies show that AVM patients face a high risk of bleeding as discussed in recent medical literature.
Several things can make an AVM rupture more likely. These include:
Age is a big factor in the risk of an AVM rupture. Younger people are at higher risk because they have more years to live. This means they have more time for an AVM to possibly rupture.
Also, as people get older, their blood vessels can change in ways that increase the risk of rupture.
Understanding these factors helps doctors figure out the best way to manage an AVM. By knowing what causes an AVM rupture, doctors can take steps to lower the risk of serious bleeding.
Getting an accurate diagnosis of arteriovenous malformations (AVMs) is key for good treatment plans. It involves advanced imaging and clinical checks. Finding out what’s wrong with AVMs is a detailed job.
Advanced imaging is essential for spotting AVMs. We use different methods to see the malformation’s structure and blood flow. The main imaging tools are:
The clinical check is also vital for AVM diagnosis. We look at symptoms, medical history, and physical checks to grasp the AVM’s impact. The clinical check includes:
After finding an AVM, we use grading systems to judge its severity. The Spetzler-Martin system is common. It looks at:
By mixing advanced imaging, clinical checks, and grading systems, we can accurately find AVMs. Then, we make treatment plans that fit each patient’s needs.
Managing arteriovenous malformations (AVMs) has improved a lot. Now, we have many ways to treat AVMs. Each method has its own benefits and risks. The right treatment depends on the AVM’s size, location, and how severe it is, as well as the patient’s health.
Surgical removal is a common and effective way to treat AVMs. It works best for AVMs that are superficial and easily accessible. The goal is to remove the AVM completely to prevent rupture and complications. We look at several things before deciding on surgery, like the AVM’s location, size, and the patient’s health.
The surgery process includes:
Endovascular embolization is a minimally invasive method. It involves delivering embolic materials directly into the AVM through its feeding arteries. This method can be used alone or with other treatments like surgery or radiosurgery. It can make the AVM smaller, making it easier to treat.
Some benefits of endovascular embolization include:
Stereotactic radiosurgery (SRS) is a precise radiation therapy. It delivers a concentrated dose of radiation to the AVM, with minimal exposure to surrounding tissues. SRS is great for AVMs that are deep-seated or located in eloquent areas of the brain, where surgery might be risky.
The process of SRS involves:
Every patient’s situation is different. Often, the best treatment is a mix of these methods, tailored to the patient’s needs. By working with a team of healthcare professionals, we can create a treatment plan that addresses the complexities of AVMs and improves patient outcomes.
Unruptured AVMs are a challenge for doctors. They need a careful approach to manage them. The choice to treat or watch depends on the AVM’s details and the patient’s health.
Many patients with unruptured AVMs are watched closely. This means regular scans like MRI or angiography. These studies check if the AVM is changing, which could mean a higher risk of rupture.
Key components of observation and monitoring protocols include:
A leading neurosurgeon says, “Watching closely is not just about monitoring the AVM. It’s also about being ready to act fast if there’s a sign of instability or rupture risk.”
“Careful observation is key in managing unruptured AVMs. It helps us weigh the risks and benefits of treatment.”
Changing your lifestyle can lower the risk of AVM rupture. Doctors often tell patients to avoid activities that raise blood pressure or strain blood vessels.
Recommended lifestyle changes include:
Deciding to treat an unruptured AVM is complex. It involves looking at the AVM’s risks, the patient’s health, and the benefits of treatment.
Factors influencing treatment decisions include:
| Factor | Description |
|---|---|
| AVM Size and Location | Larger AVMs or those in critical areas may need more aggressive treatment |
| Patient Age and Health | Younger patients or those with fewer health issues might get more invasive treatments |
| AVM Characteristics | Things like how the AVM drains blood and if there are aneurysms can affect rupture risk |
Healthcare providers use these factors to create a plan that suits each patient with an unruptured AVM. This plan aims to balance risks and benefits.
An AVM rupture is a serious event that needs quick action. It can lead to a hemorrhagic stroke, causing severe and lasting brain damage. Knowing how to handle an AVM rupture is key for doctors and patients.
Spotting an AVM rupture is the first step. Symptoms include sudden, severe headaches, nausea, vomiting, and weakness or numbness. “The sudden onset of a severe headache, often described as ‘the worst headache of my life,’ is a classic symptom of AVM rupture,” say doctors.
Other signs include seizures, vision changes, or trouble speaking. It’s vital to notice these symptoms quickly and get medical help right away.
Dealing with an AVM rupture focuses on keeping the patient stable, stopping bleeding, and managing brain pressure. First, doctors check the patient’s airway, breathing, and circulation (ABCs). They might give oxygen, control blood pressure, and make sure the patient is breathing well.
Sometimes, surgery is needed to relieve pressure or fix the AVM. Doctors might also use endovascular embolization or other small procedures to block the AVM.
Recovering from an AVM rupture is a big step. It involves many healthcare teams, like neurologists and rehabilitation experts. The aim is to help the patient get back to normal and improve their life quality.
Rehab might include physical, occupational, and speech therapy. It depends on what parts of the body were affected. Keeping an eye on the patient and following up is also important to manage any lasting effects and prevent future problems.
In summary, managing an AVM rupture needs a team effort. By knowing the signs, providing immediate care, and supporting recovery, we can help patients recover better from this serious condition.
Arteriovenous malformations (AVMs) are complex vascular anomalies that pose significant health risks. Knowing what AVM stands for and its implications is key for both patients and healthcare providers. An AVM is a tangle of blood vessels that can disrupt normal blood flow, leading to various complications.
The danger of AVMs lies in their ability to rupture, causing hemorrhage and neurological damage. The risk of rupture and associated complications makes it essential to carefully manage AVMs. We must consider the severity of the malformation, its location, and the patient’s overall health when determining the best course of treatment.
AVM medical management involves a range of options, from observation and monitoring to surgical intervention. The decision to treat an unruptured AVM depends on several factors, including the risk of rupture and the benefits of treatment. By understanding the serious nature of AVMs and the available treatment options, patients can make informed decisions about their care.
In conclusion, AVMs are serious vascular anomalies that require careful management to prevent rupture and other complications. We emphasize the importance of understanding the risks associated with AVMs and the need for timely medical intervention to mitigate these risks.
AVM stands for arteriovenous malformation. It’s a condition with an abnormal tangle of blood vessels.
Arteriovenous malformation is when arteries and veins connect abnormally. This skips the capillary network.
The exact cause of AVMs is often unknown. But genetic changes or mutations during development are thought to play a role.
Symptoms include seizures and weakness. Physical symptoms vary based on the AVM’s location.
AVMs are dangerous because they can rupture. This leads to bleeding and can cause neurological damage.
Rupture can be caused by pressure in weakened blood vessels. Age and certain triggers also increase risk.
Advanced imaging techniques are used to diagnose AVMs. Clinical assessment and grading systems also help evaluate severity.
Treatment options include surgery, endovascular embolization, and radiosurgery. The choice depends on size, location, and severity.
Management involves weighing treatment risks and benefits. Options include observation, monitoring, and lifestyle changes to reduce rupture risk.
Emergency management includes recognizing acute hemorrhage signs. It also involves critical care and recovery after rupture.
While AVMs aren’t directly hereditary, genetics can influence their development.
Yes, AVMs can be asymptomatic. They may remain undetected until they rupture or cause significant damage.
AVMs are relatively rare. Their exact prevalence is hard to determine due to asymptomatic cases
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us