When you notice skin changes, swelling, or bleeding without a clear reason, it’s important to find out why. At Liv Hospital, we focus on treating complex vascular conditions with care. We use the latest medical methods to help our patients.
An arteriovenous malformation (AVM) is when arteries and veins connect in a way they shouldn’t. This messes up blood flow and stops tissues from getting oxygen. It can cause many health problems.
We know how important it is to give the right care to those with AVMs. We study each case deeply. We learn about the condition, its causes, symptoms, and treatments. This helps us give our patients the best chance for a good outcome.
Key Takeaways
- Arteriovenous malformation (AVM) is an abnormal connection between arteries and veins.
- AVMs disrupt normal blood flow and oxygen delivery to tissues.
- Understanding AVM causes, symptoms, and treatment options is key for good care.
- Liv Hospital offers patient-centered, multidisciplinary treatment for complex vascular conditions.
- The latest medical protocols are used to guide treatment at Liv Hospital.
Decoding the AVM Medical Acronym and Its Significance

It’s important to know what AVM means for health. An arteriovenous malformation (AVM) is a mix-up of blood vessels. It messes up how blood moves from arteries to veins.
Definition of Arteriovenous Malformation
An AVM is when arteries and veins connect in a bad way. Usually, arteries bring oxygen-rich blood to capillaries. Then, oxygen is swapped for carbon dioxide. But in an AVM, blood goes straight from arteries to veins, missing capillaries.
This can cause health problems. The area affected doesn’t get enough oxygen.
Normal Blood Vessel Structure vs. AVM Abnormalities
Normally, arteries split into smaller arterioles and then capillaries. This is where oxygen and nutrients are exchanged. After that, blood goes into venules and then veins.
But, an AVM makes a direct path from arteries to veins. This can happen in places like the brain, spinal cord, skin, or limbs. It leads to different symptoms and problems, depending on where it is.
AVMs can be there from birth or show up later. Some people might not have any symptoms. But others might feel pain, swelling, or have problems with their brain or nerves. Knowing about AVMs helps doctors diagnose and treat them right.
Types and Locations of Arteriovenous Malformations

Arteriovenous malformations (AVMs) can happen in different parts of the body. Each location has its own set of symptoms and treatment options. Where an AVM is located greatly affects how it’s diagnosed and treated.
Brain and Spinal AVMs
AVMs in the brain or spinal cord are very serious. They can cause seizures, headaches, or even life-threatening bleeding. It’s important to find and treat them quickly to avoid serious problems.
Brain AVMs are close to important brain areas. Treating them requires a team of experts, including neurosurgeons and neuroradiologists.
Peripheral AVMs
Peripheral AVMs are found in the limbs and other tissues. They can cause swelling, pain, and skin changes. In severe cases, they can lead to ulcers or bleeding. These AVMs can make patients very uncomfortable and limit their ability to function.
AVMs in the legs or arms can make it hard to use the limb and can affect how it looks. Doctors often use a mix of treatments, including endovascular procedures and surgery.
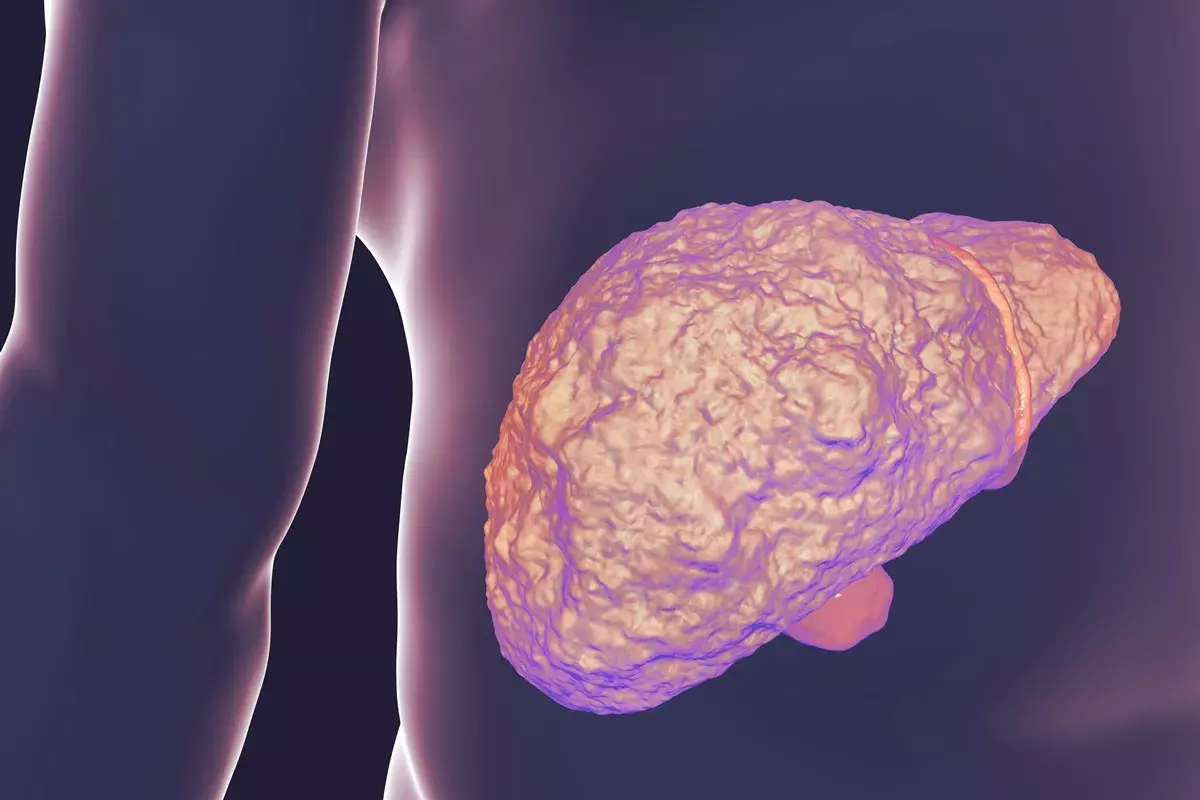
Cardiac and Visceral AVMs
AVMs can also appear in the heart and organs like the liver or kidneys. These cases are rare but can be very challenging to manage. Cardiac AVMs can change blood flow in the heart.
Visceral AVMs can cause different symptoms based on where they are and how big they are. It’s key to find and treat them early to avoid serious issues like bleeding or organ failure.
In summary, the type and location of an AVM are key in understanding its symptoms and treatment. Knowing this helps doctors give the best care to patients with AVMs.
Causes and Risk Factors of Arteriovenous Malformations
The exact causes of arteriovenous malformations (AVMs) are not fully understood. Research has shed light on several risk factors. AVMs are considered to be congenital anomalies that occur during fetal development.
Developmental Origins During Fetal Growth
AVMs are believed to form during fetal development, when the vascular system is forming. Abnormal development of blood vessels can lead to the creation of AVMs. Research suggests that both genetic and environmental factors may contribute to this abnormal development.
Are AVMs Genetic? Hereditary Factors Explained
While most AVMs are not inherited, there is evidence to suggest that genetic factors may play a role in their development. Certain genetic syndromes have been associated with an increased risk of AVMs.
“Genetic factors can contribute to the development of AVMs, though most cases are sporadic.”
Associated Genetic Syndromes and Conditions
Several genetic syndromes have been linked to an increased risk of developing AVMs. These include:
- Hereditary Hemorrhagic Telangiectasia (HHT)
- Sturge-Weber Syndrome
- Klippel-Trenaunay Syndrome
| Genetic Syndrome | Description | AVM Risk |
|---|---|---|
| Hereditary Hemorrhagic Telangiectasia (HHT) | A disorder characterized by abnormal blood vessel formation | High |
| Sturge-Weber Syndrome | A condition involving a port-wine stain and neurological abnormalities | Moderate |
| Klippel-Trenaunay Syndrome | A rare disorder involving abnormal growth of blood vessels, soft tissue, and bone | Moderate |
Understanding the causes and risk factors of AVMs is key for early detection and management. While the exact mechanisms are under research, it’s clear that both genetic and developmental factors play significant roles.
Signs and Symptoms of AVM by Location
Knowing the signs of AVMs is key for early treatment. AVMs can show up in different ways, based on where they are, how big they are, and if they’ve ruptured.
General Manifestations
AVMs can cause headaches, seizures, and muscle weakness. These happen because of the abnormal blood flow and pressure on nearby tissues.
AVMs might not show symptoms until they rupture. Then, they can cause serious issues like bleeding or stroke. It’s important to watch for these signs to get medical help.
Location-Specific Symptoms
The symptoms of AVMs depend on where they are. For example, brain AVMs can lead to dizziness, vision problems, or trouble speaking. Spinal AVMs might cause back pain, weakness, or numbness in the limbs.
Peripheral AVMs, found in limbs or other body parts, can cause skin changes or swelling. They might also lead to chronic pain or limited mobility.
When to Seek Immediate Medical Attention
If you have symptoms of an AVM rupture, like a sudden severe headache, confusion, or loss of consciousness, get help right away. Bleeding from an AVM can be very dangerous.
If you know you have an AVM, watch your symptoms closely. Tell your doctor about any changes. Regular check-ups and proper care can help avoid serious problems.
Potential Complications of Untreated AVMs
AVMs that are not treated can cause serious problems. These problems can even be life-threatening. Getting medical help quickly is very important.
Bleeding and Rupture: Acute Emergencies
One big risk of untreated AVMs is bleeding or rupture. If an AVM bleeds, it can cause sudden and severe symptoms. These symptoms include:
- Severe headache, often described as “the worst headache of my life”
- Confusion or altered mental status
- Weakness or numbness in parts of the body
- Seizures
Such bleeding events are medical emergencies that need immediate care. The risk of rupture is higher in certain AVMs. These are AVMs that are large or deep.
Chronic Complications and Progressive Damage
Untreated AVMs can also cause chronic complications. These complications can damage tissues over time. They may include:
- Progressive neurological decline due to compression or steal phenomenon
- Chronic pain resulting from the AVM’s presence
- Skin changes or ulcers in cases of superficial AVMs
- High-output cardiac failure in large AVMs
There are treatments available, like AVM embolization. Embolization blocks the abnormal blood flow in the AVM. This reduces the risk of complications. Knowing about these complications shows why it’s important to get medical help for AVMs.
Diagnostic Approaches for Arteriovenous Malformations
Diagnosing arteriovenous malformations (AVMs) needs a detailed approach. This includes clinical checks, advanced imaging, and looking at other possible conditions. We’ll dive into these methods to see how they help in finding AVMs accurately.
Clinical Evaluation and Physical Examination
The first step is a thorough check-up and physical exam. We look for signs like abnormal pulsations, murmurs, or uneven limbs. A detailed medical history helps spot risk factors and related conditions.
During the exam, we search for visible signs of AVMs. These include:
- Visible pulsations or thrills over the affected area
- Bruits or murmurs heard on auscultation
- Limb length discrepancy or asymmetry
- Skin discoloration or ulceration
Advanced Imaging Techniques
Advanced imaging is key in confirming AVMs and understanding their details. We use different imaging methods to see the AVM’s size, location, and blood flow.
The main imaging methods for AVM diagnosis are:
- MRI (Magnetic Resonance Imaging): Shows detailed images of soft tissues and the AVM’s extent.
- Angiography: Visualizes blood vessels and flow in the AVM, important for treatment planning.
- Ultrasound: Useful for checking blood flow and finding AVMs, mainly in peripheral areas.
- CT (Computed Tomography) Scan: Helps evaluate the AVM’s structure and any related issues.
A comparison of these imaging techniques is provided in the table below:
| Imaging Modality | Key Features | Clinical Utility |
|---|---|---|
| MRI | High soft tissue resolution, no radiation | Assesses AVM extent, involvement of surrounding tissues |
| Angiography | Detailed vascular anatomy, flow dynamics | Crucial for treatment planning, embolization procedures |
| Ultrasound | Non-invasive, real-time blood flow assessment | Initial screening, peripheral AVM assessment |
| CT Scan | Quick, high-resolution images, bony structure assessment | Evaluating AVM structure, detecting complications |
Differential Diagnosis Considerations
When diagnosing AVMs, it’s important to think about other possible conditions. We need to rule out other vascular malformations, tumors, or conditions that might look similar. This helps us find the right diagnosis.
Some conditions to consider in the differential diagnosis include:
- Other types of vascular malformations (e.g., venous, lymphatic)
- Arterial aneurysms
- Vascular tumors
- Soft tissue tumors
By combining clinical checks, advanced imaging, and considering other conditions, we can accurately diagnose AVMs. Then, we can plan the best treatment.
Comprehensive Treatment Options for AVMs
Treating arteriovenous malformations (AVMs) needs a detailed plan. This plan is made for each patient, based on their needs and the AVM’s specifics. Every patient is different, so their treatment must be too.
Conservative Management Strategies
For some, watching and waiting might be the best first step. This means regular checks with imaging to see how the AVM changes. We also help manage symptoms and prevent problems with medicine and lifestyle changes.
This approach is often for patients with AVMs that don’t cause symptoms or have a high risk of surgery problems. Our team helps patients understand the pros and cons of this method and keeps a close eye on their condition.
Endovascular Procedures
Endovascular embolization is a key part of AVM treatment. It’s a small procedure that blocks the AVM’s blood vessels. We use advanced imaging to make sure it’s done safely and accurately.
This method can be used alone or with surgery or radiosurgery. Our team decides the best plan for each patient, looking at the AVM’s location and the patient’s health.
Surgical Interventions and Resection
Surgery is a big part of AVM treatment for many patients. It’s often for those with high-risk features or big symptoms. Our neurosurgeons talk with patients and their families about surgery’s risks and benefits.
The goal of surgery is to remove the AVM completely. This stops future bleeding risks. We use the latest techniques and monitoring during surgery to help it succeed.
| Treatment Option | Indications | Benefits | Risks |
|---|---|---|---|
| Conservative Management | Asymptomatic AVMs, high surgical risk | Avoids immediate risks of intervention | Risk of future bleeding or growth |
| Endovascular Embolization | AVMs with suitable vascular anatomy | Minimally invasive, can reduce AVM size | Risk of incomplete occlusion, procedural complications |
| Surgical Resection | High-risk AVMs, significant symptoms | Can eliminate AVM, reduce bleeding risk | Surgical risks, possible neurological problems |
A leading neurosurgeon says, “Choosing AVM treatment is very personal. It needs a team effort for the best results.” This shows how important a detailed plan is for each patient.
Embolization of AVM: Procedure, Benefits, and Risks
Embolization is a key treatment for arteriovenous malformations (AVMs). It’s a less invasive way to lessen symptoms and avoid complications. This method involves using materials to block abnormal blood flow in the AVM.
Technique Overview
AVM embolization is a detailed process that needs precise navigation and clear vision. We use advanced imaging technologies to guide the catheter to the AVM. This ensures the embolic materials are placed correctly.
The goal is to cut down blood flow through the malformation. This helps reduce symptoms and lowers the risk of rupture.
The materials used can be glue-like substances, coils, or particles. The choice depends on the AVM’s size, location, and feeding arteries.
The Procedure Process and Recovery Timeline
The procedure is done under general anesthesia or sedation. We carefully monitor the patient’s vital signs to keep them safe.
- Access is gained through a small incision in the groin to introduce the catheter.
- The catheter is guided to the AVM using real-time imaging.
- Embolic materials are injected to block blood flow through the AVM.
- The catheter is removed, and the incision is closed.
Recovery times vary, but most patients stay in the hospital for at least 24 hours. We provide detailed post-procedure care to manage any discomfort and watch for complications.
Success Rates and Long-term Outcomes
The success of AVM embolization depends on several factors. These include the AVM’s size and location, and the patient’s health. Our team reviews each case individually to find the best treatment plan.
- The ultimate goal is to completely obliterate the AVM. But this might not always be possible in one procedure.
- Partial embolization can also provide significant symptom relief and lower the risk of future complications.
- Follow-up care is key to monitor the AVM’s response to treatment and address any remaining or recurring issues.
Understanding the embolization procedure, its benefits, and risks helps patients make informed decisions. We are committed to providing personalized care to ensure the best outcomes for each patient.
Recent Advances in AVM Treatment and Research
The field of arteriovenous malformation (AVM) treatment is changing fast. New research and treatments are helping patients. We now know more about AVMs, leading to better care.
Innovative Therapeutic Approaches
New ways to treat AVMs are being developed. Endovascular therapies are getting better. Now, we can treat AVMs more precisely.
Techniques like embolic liquid agents and stent-assisted coiling are making a big difference. They help patients with complex AVMs.
A study found that liquid embolic agents are changing AVM treatment. They offer a lasting and effective solution for many patients. This shows how AVM care is always getting better.
Targeted Medications and Emerging Therapies
Researchers are also working on targeted medications and new treatments for AVMs. These aim to better manage symptoms and lower risks.
- Anti-angiogenic therapies to slow AVM growth
- Medicines to help with symptoms and improve life quality
- Gene therapies to address AVM causes
These new treatments are very promising. They offer hope for the future of AVM management.
Future Directions in AVM Management
Looking ahead, AVM treatment will keep getting better. Personalized medicine will be more important. Treatments will be made just for each patient’s AVM.
“The future of AVM treatment lies in a multidisciplinary approach, combining the expertise of neurosurgeons, interventional radiologists, and other specialists to provide complete care for patients.”
By keeping up with AVM research and treatments, we can help patients more. We aim to improve their lives and outcomes.
Conclusion
It’s key for patients to understand the avm medical acronym and its meaning. Arteriovenous malformation, or AVM, is a complex condition. It needs careful management to avoid problems and improve health.
We’ve looked at AVM’s causes, symptoms, and treatment choices. Knowing about AVM helps patients make better decisions. They can work with their doctors to get the best care.
Medical research and technology are making AVM treatment better. If symptoms don’t go away or get worse, see a doctor. With the right care, people with AVMs can live healthier, happier lives.
FAQ
What does AVM stand for in medical terms?
AVM stands for Arteriovenous Malformation. It’s a condition where arteries and veins connect directly, skipping capillaries.
Are AVMs genetic or hereditary?
Most AVMs aren’t passed down through genes. But, some genetic syndromes can raise the risk. We look into the genetic side of AVMs.
What are the symptoms of an AVM?
Symptoms vary by location. They can include pain, swelling, and abnormal bleeding. For example, brain AVMs might cause neurological problems.
How are AVMs diagnosed?
Doctors use a mix of clinical checks, MRI, angiography, and genetic tests. These help pinpoint the AVM and any linked syndromes.
What are the treatment options for AVMs?
Treatments range from watching and waiting to endovascular and surgical methods. The best option depends on the AVM’s size, location, and the patient’s health.
What is embolization of an AVM?
Embolization is a non-surgical method. It blocks the AVM’s blood flow with coils or glue. This aims to prevent bleeding and complications.
Can AVMs rupture or bleed?
Yes, AVMs can rupture or bleed, posing a serious risk. Understanding and managing the condition can help reduce this risk.
Are there any new or emerging treatments for AVMs?
Research on AVMs is active, with new treatments and medications being tested. Keeping up with these advancements is key for effective management.
Can AVMs be found in different parts of the body?
Yes, AVMs can occur in many places, like the brain, spinal cord, and even the heart. The location affects symptoms and treatment.
How do AVMs affect the heart?
Heart AVMs can cause serious issues, like irregular heartbeats or heart failure. This depends on the AVM’s size and heart location.
Is it possible for AVMs to be asymptomatic?
Yes, some AVMs may not show symptoms until they grow or complications happen. Regular check-ups can catch them early.