Last Updated on November 27, 2025 by Bilal Hasdemir
Abdominal aortic aneurysm (AAA) surgical repair is a key procedure. It stops a life-threatening rupture of an aortic aneurysm. We offer new and effective treatments for those with this condition.
There are two main ways to do triple A repair operation. Open surgery and endovascular aneurysm repair (EVAR). Open surgery uses a synthetic graft to replace the weak part of the aorta. EVAR is less invasive, using a stent graft to repair the aneurysm.
At Liv Hospital, we focus on our patients. Our expertise in aaa surgery repair is unmatched. We offer top-notch healthcare and support for international patients.
Key Takeaways
- AAA surgical repair is a major procedure to treat an aortic aneurysm.
- Two primary approaches: open surgery and endovascular aneurysm repair (EVAR).
- Open surgery replaces the weakened aorta segment with a synthetic graft.
- EVAR is a minimally invasive procedure using a stent graft.
- Liv Hospital provides patient-centered expertise and extensive care.
Understanding Abdominal Aortic Aneurysms

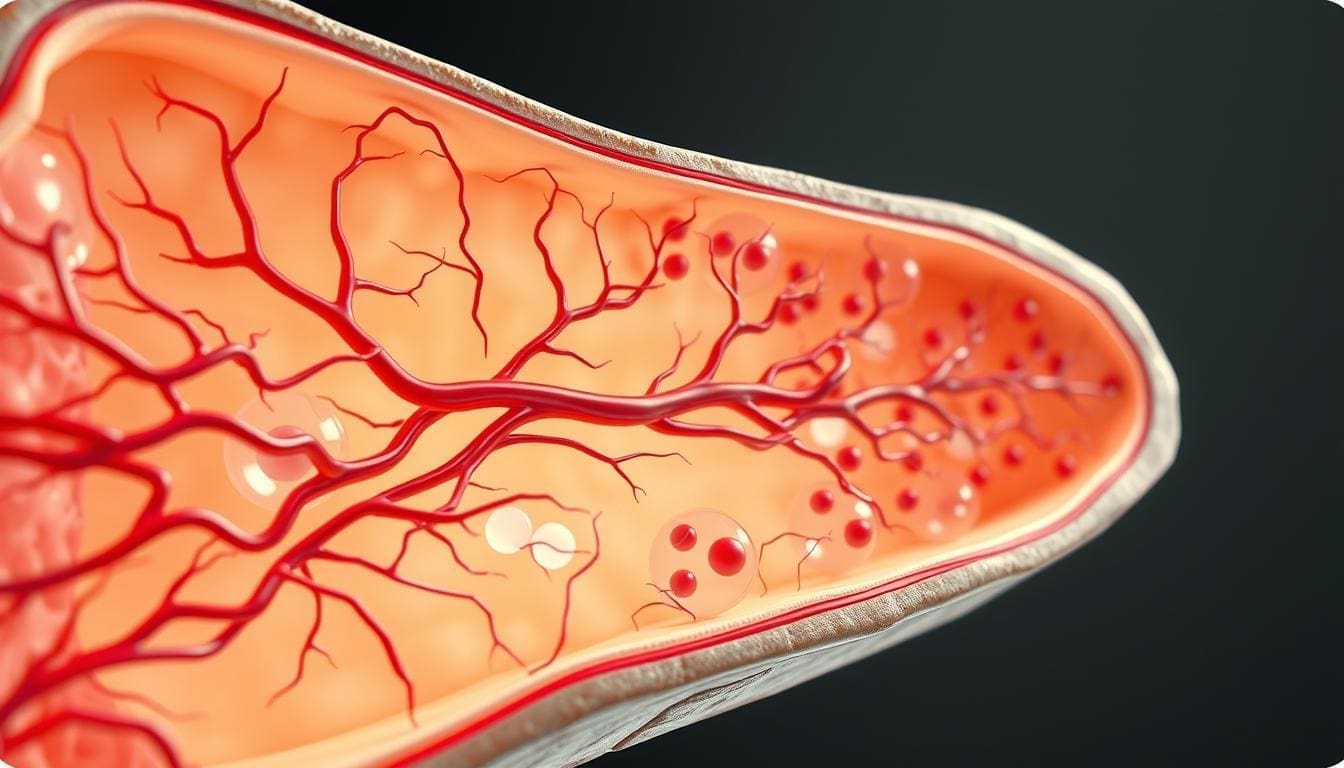
The abdominal aorta is a key part of our blood system. Aneurysms here can be deadly. An abdominal aortic aneurysm (AAA) happens when the aorta, the biggest artery, gets big in the belly.
Definition and Anatomy of the Aorta
The aorta is a vital artery that starts at the heart and goes down to the belly. An abdominal aortic aneurysm is when the belly aorta gets bigger than 3 cm or more than half its normal size at the diaphragm. This happens when the aorta’s wall gets weak and bulges out.
Causes and Risk Factors
Many things can lead to AAA. Smoking is a big risk because it harms the aorta’s wall. Other risks include being older, male, having a family history, and certain genetic conditions. High blood pressure and atherosclerosis also play a part.
Prevalence and Demographics
AAA is more common in some groups in the US. Men over 65 are at higher risk. Screening programs aim to find AAA in these groups early to save lives.
Detecting and Diagnosing AAA

Finding an abdominal aortic aneurysm (AAA) early is key to managing it well. We’ll talk about the signs and symptoms of AAA. We’ll also cover how to screen and diagnose it.
Common Symptoms and Warning Signs
Mostly, AAA doesn’t show symptoms. But when it does, the symptoms can be serious. You might feel pain in your belly or back, or notice a pulsating mass in your abdomen. If you notice these signs, get medical help right away.
Warning signs of a ruptured AAA include:
- Severe abdominal or back pain
- Low blood pressure
- Rapid heart rate
- Loss of consciousness
Screening and Diagnostic Methods
There are several ways to find AAA. The most common are:
- Ultrasound: A non-invasive test that uses sound waves to create images of the aorta.
- Computed Tomography (CT) scans: Provides detailed cross-sectional images of the aorta.
- Magnetic Resonance Imaging (MRI): Uses magnetic fields to create detailed images of the aorta.
Measuring Aneurysm Size and Growth Rate
The size of an AAA is very important. It helps doctors know if it might burst. Doctors use ultrasound or CT scans to measure it. They also watch how fast it grows to see if it’s getting bigger.
| Aneurysm Size | Risk of Rupture | Recommended Follow-Up |
|---|---|---|
| Less than 3 cm | Low | Regular ultrasound every 2-3 years |
| 3-4 cm | Moderate | Ultrasound every 6-12 months |
| 4-5.5 cm | High | Ultrasound or CT scan every 6 months |
| Greater than 5.5 cm | Very High | Surgical intervention considered |
When Is AAA Surgical Repair Necessary?
Deciding if AAA surgical repair is needed involves looking at several important factors. We check different signs to figure out the best treatment for patients with abdominal aortic aneurysms.
Size Thresholds for Intervention
The size of the aneurysm is a key factor in deciding on AAA surgical repair. If the aneurysm is 5.5 cm or bigger, surgery is usually recommended. But, if a patient is at high risk of rupture or has other health issues, surgery might be needed even if the aneurysm is smaller.
An aneurysm between 5.0 to 5.4 cm might need more checks and a look at rupture risk. The choice to have surgery at these sizes depends on the patient’s health, life expectancy, and symptoms.
Symptom-Based Indicators
Symptoms are also important in deciding on AAA intervention. If a patient has abdominal pain, back pain, or tenderness, they need urgent care. These symptoms mean the aneurysm might be about to rupture, making surgery a must.
- Abdominal pain or tenderness
- Back pain
- Pain radiating to the groin, buttocks, or legs
Even if the aneurysm is smaller than usual, symptoms can mean a higher risk of rupture. This makes quick surgery very important.
Risk Assessment for Rupture
Figuring out the AAA rupture risk is complex. We look at the patient’s vascular health, other medical conditions, and the aneurysm’s shape and growth rate.
Fast growth or an unusual shape in the aneurysm means a higher risk of rupture. We use advanced imaging and regular checks to see these factors. This helps us decide when AAA surgical repair is best.
By carefully looking at these signs, we can make smart choices about when AAA surgical repair is needed. This ensures patients get the right treatment on time to prevent rupture and improve their health.
Overview of AAA Surgical Repair Options
AAA surgical repair offers two main choices: open surgery and endovascular repair. We’ll look at each, covering their differences, who they’re best for, and what to do before surgery.
Open Surgical Repair vs. Endovascular Approach
Open surgery requires an incision in the belly to reach the aorta. Surgeons then replace the weak part with a synthetic tube. This method has been around for a long time and works well for many.
EVAR, on the other hand, is less invasive. A stent graft is inserted through the groin arteries, bypassing the weak spot. This method is quicker to recover from and better for those at high risk for open surgery.
Patient Selection Criteria for Each Method
Choosing the right surgery depends on several things. These include the patient’s health, the aneurysm’s shape, and any other health issues. For example, younger patients or those with complex aneurysms might do better with open surgery. But, those with serious health problems or a difficult abdomen might be better off with EVAR.
We look at many factors, like age, kidney function, and blood vessel health, to decide. A vascular specialist’s detailed evaluation is key in making this choice.
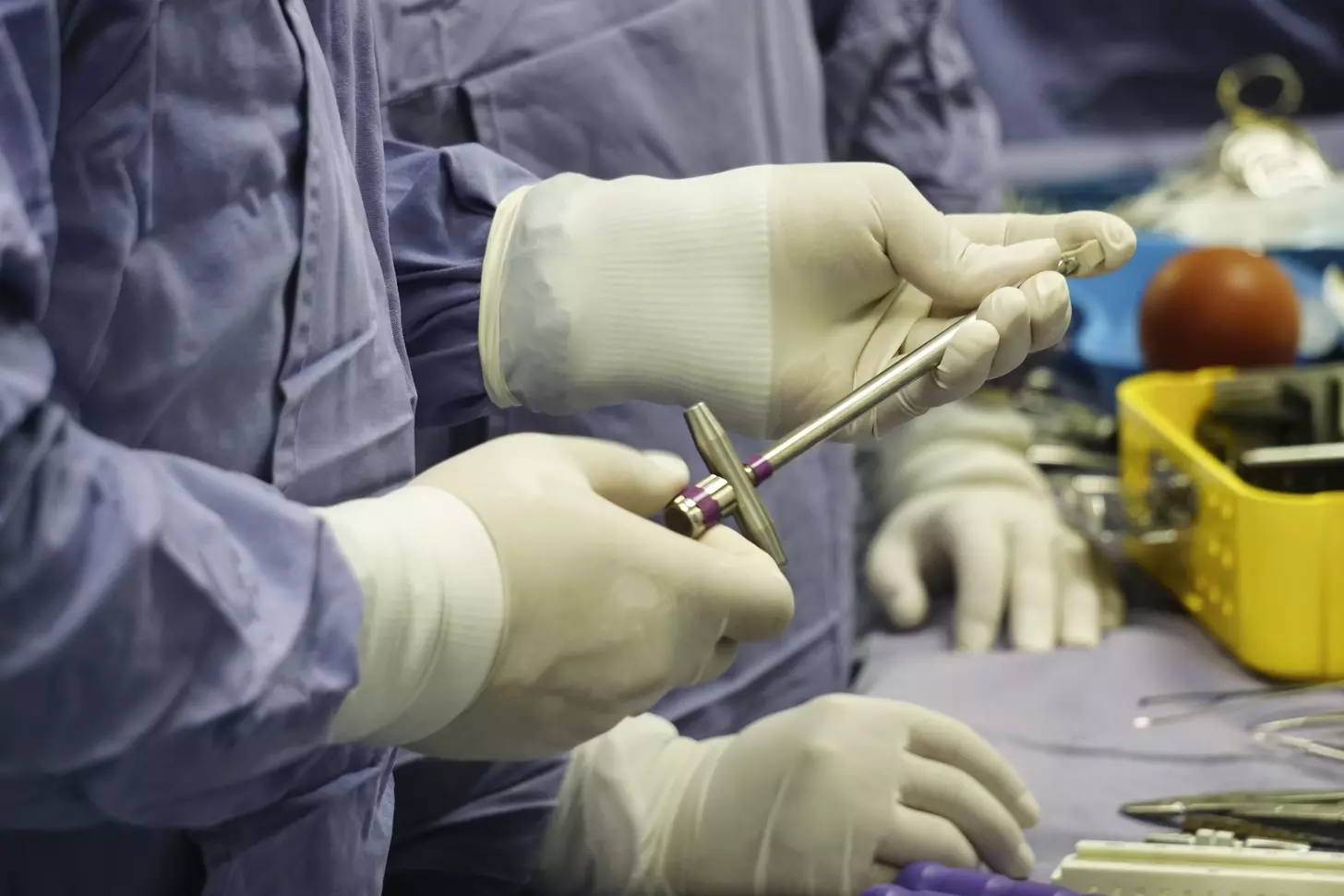
Preoperative Planning and Preparation
Planning before surgery is essential for both open and endovascular repairs. We use CT scans to check the aneurysm’s size and shape, and the patient’s blood vessels. This helps us understand the situation fully.
We also review the patient’s medical history, including past surgeries, heart risks, and current medicines. This helps us prepare the patient and plan for any possible issues during surgery.
The Open Triple A Repair Operation Process
Patients with abdominal aortic aneurysms get a lasting fix with open surgery. It removes the aneurysm and puts in a synthetic graft. This method needs a big cut to reach the aorta.
Anesthesia and Surgical Access
The surgery starts with general anesthesia to keep the patient comfortable. A midline incision in the abdomen gives the best view of the aorta. This lets surgeons see and work on the aneurysm directly.
Careful dissection is done to show the aorta and nearby areas. This is to avoid harming other vessels or nerves. The incision and how the surgery is done can change based on the patient and the surgeon.
Aortic Clamping and Aneurysm Management
Next, the aorta is clamped to stop blood flow in the aneurysm. This step is very important and needs to be done right to keep the patient safe.
The aneurysm is then opened, and any clots or debris are taken out. Aortic clamping keeps blood from flowing back and makes the area clear for surgery.
Synthetic Graft Placement Techniques
After dealing with the aneurysm, a synthetic graft is sewn in to replace the bad part of the aorta. The graft is picked and placed carefully to make sure the repair lasts.
Suturing techniques are used to make a tight seal. This ensures blood flows right and the aneurysm is cut off. When the clamp is removed, blood starts flowing through the graft again.
Endovascular Aneurysm Repair (EVAR) Procedure
The EVAR procedure is a new way to treat abdominal aortic aneurysms without open surgery. It’s less invasive, which means less pain and quicker recovery. This method also lowers the chance of serious side effects.
Minimally Invasive Approach Through Groin Incisions
We do EVAR by making small cuts in the groin to reach the femoral arteries. This method is less invasive than traditional surgery. It causes less damage to tissues and helps wounds heal faster.
Small incisions also lower the risk of wound problems. This makes the whole process safer for patients.
Stent Graft Deployment and Positioning
After we get to the arteries, we put in a stent graft. This graft seals off the aneurysm and keeps blood flowing. Getting the stent graft in the right spot is very important.
We pick the right size and type of stent graft for each patient. This ensures it fits well and works right. The stent graft is made to last a long time, so you might not need more surgeries.
Intraoperative Imaging and Verification
We use imaging like fluoroscopy and angiography during EVAR. These tools help us place the stent graft correctly. This lets us make changes right away if needed.
After the procedure, we watch the patient closely. We deal with any problems quickly. The advanced imaging and careful stent graft placement are key to EVAR’s success.
AAA Surgical Repair Recovery and Rehabilitation
Recovering well after AAA repair is key. The surgery type, open or EVAR, affects how you get better.
Hospital Stay Duration Differences
Hospital stays differ for open surgery and EVAR. EVAR patients usually stay less than those with open surgery. Healthcare guidelines say EVAR patients stay 1-3 days. Open surgery patients might stay 5-7 days or more.
Key factors influencing hospital stay duration include:
- Presence of comorbidities
- Age of the patient
- Intraoperative and postoperative complications
Pain Management Protocols
Managing pain well is important for recovery. We use many ways to control pain, like:
- Epidural anesthesia
- Patient-controlled analgesia (PCA)
- Oral pain medications
One study found, “Adequate pain control is essential for reducing stress and promoting healing”
Adequate pain control is essential for reducing stress and promoting healing.
Physical Therapy and Activity Progression
Moving early and doing physical therapy helps. We tailor therapy to each patient and increase it slowly.
Return to Normal Activities Timeline
When you can go back to normal activities depends on your surgery and health. Here’s what you can expect:
- Light activities in 2-4 weeks
- Moderate activities in 6-8 weeks
- Strenuous activities in 3-6 months
It’s important to follow your doctor’s advice and go to all follow-up appointments for a smooth recovery.
Potential Complications of Stomach Aneurysm Surgery
AAA surgical repair can save lives, but it comes with risks. We need to talk about the possible problems that can happen. These include immediate risks right after surgery and long-term issues.
Immediate Post-Operative Risks
Right after surgery, patients face several dangers. “Bleeding and hematoma formation are significant concerns in the early post-operative period,” as noted in medical literature. We closely watch patients to reduce these risks.
Some immediate risks are:
- Cardiac complications due to the stress of surgery
- Respiratory issues, such as pneumonia or respiratory failure
- Renal complications, including acute kidney injury
- Graft-related complications, such as endoleak or graft migration
For more detailed information on complications related to endovascular abdominal aortic repair, we refer to resources like UpToDate. It offers detailed insights into managing these risks.
Long-Term Complications
Patients may also face long-term issues after AAA repair. These include graft failure, risk of rupture, and complications from the surgery, like incisional hernias in open repair.
As one study shows, “Long-term surveillance is key for spotting and handling late complications after EVAR.” This underlines the need for ongoing care after AAA repair.
Long-term complications may include:
- Graft durability issues, needing ongoing checks
- Risk of new aneurysm formation in other areas
- Potential for reintervention to address complications
Knowing these complications helps us manage patient expectations and outcomes better. Our care goes beyond surgery, with thorough follow-up and support to lessen these risks.
Outcomes and Success Rates of AAA Procedures
The success of AAA surgery depends on many things. These include the repair method and the patient’s health. We will look at how different repairs compare, focusing on death rates, quality of life, and survival chances.
Comparative Mortality Statistics
Research shows EVAR has a lower death rate right after surgery compared to open repair. EVAR is linked to less death risk in the first few days, making it a good choice for high-risk patients. But, survival chances over time are about the same for both methods.
A big study found EVAR’s 30-day death rate was between 0.5% and 1.5%. Open repair’s rate was between 2% and 4%. This means EVAR might be better in the short term, but long-term results are similar.
Quality of Life After Different Repair Methods
How well patients do after AAA surgery is key. Studies say EVAR patients recover faster and feel better sooner than open repair patients. This is because EVAR is less invasive.
But, over time, both groups tend to have similar quality of life. Age, health problems, and how well patients were before surgery affect how they do after surgery.
Long-Term Survival Rates and Durability
Survival chances after AAA surgery depend on many things. These include the repair type, patient health, and aneurysm details. EVAR might offer a survival edge early on, but long-term survival is about the same as open repair.
Follow-Up Requirements and Monitoring
It’s important to keep up with follow-ups after AAA surgery. This helps catch any problems early and makes sure the repair lasts. For EVAR, this means regular scans to watch for leaks or graft movement.
- Patients who had EVAR need to be checked for life.
- Open repair patients also need regular check-ups to watch for complications.
Conclusion: Advances in AAA Surgical Repair
Advances in AAA surgical repair have greatly improved treatment options for patients with abdominal aortic aneurysms. We’ve looked at how to detect and diagnose AAA. We’ve also discussed the different surgical repair methods, like open surgery and endovascular aneurysm repair (EVAR).
It’s very important to act quickly when dealing with AAA. Surgical repair is key to preventing a life-threatening rupture. Knowing the pros and cons of each treatment helps patients and doctors make the best choice.
As we keep improving AAA treatments, early detection and action are more important than ever. New technologies and methods mean better results and a higher quality of life for patients after surgery.
FAQ
What is AAA surgical repair?
AAA surgical repair is a critical procedure. It prevents life-threatening rupture of a stomach aneurysm. It involves either open surgery or endovascular aneurysm repair (EVAR) to replace or repair the weakened aorta segment.
What are the main approaches to AAA repair?
There are two main approaches to AAA repair. Open surgery involves replacing the weakened aorta segment with a synthetic graft. EVAR is a minimally invasive procedure that uses a stent graft to repair the aneurysm.
What are the causes and risk factors associated with AAA development?
Smoking, age, and genetics are the main causes and risk factors for AAA. They can weaken the aortic wall and lead to an aneurysm.
How is AAA detected and diagnosed?
AAA is detected and diagnosed through screening and diagnostic methods. Ultrasound and CT scans measure aneurysm size and growth rate.
When is AAA surgical repair necessary?
AAA surgical repair is necessary when the aneurysm size exceeds certain thresholds. It’s also needed when symptoms occur or the risk of rupture is high.
What is the difference between open surgery and EVAR for AAA repair?
Open surgery is more invasive with a larger incision. EVAR is minimally invasive with smaller incisions in the groin. This results in different recovery times and risks.
How is the recovery process after AAA surgical repair?
The recovery process varies between open surgery and EVAR. Differences include hospital stay duration, pain management, physical therapy, and activity progression.
What are the possible complications after stomach aneurysm surgery?
Possible complications include immediate post-operative risks and long-term complications. These can be mitigated with proper preoperative planning, surgical techniques, and postoperative care.
What are the outcomes and success rates of AAA procedures?
Outcomes and success rates vary depending on the repair method. Important factors include mortality statistics, quality of life, and long-term survival rates.
How often is follow-up required after AAA surgical repair?
Follow-up is required regularly after AAA surgical repair. The frequency depends on the type of repair and individual patient factors.
What are the advances in AAA surgical repair?
Advances include improvements in surgical techniques, stent graft technology, and imaging modalities. These lead to better outcomes and reduced risks for patients.
References
- Avishay, D. M., & Reimon, J. D. (2024, January 25). Abdominal aortic repair. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554573/ NCBI+1
- MedlinePlus. (n.d.). Abdominal aortic aneurysm: Open repair. Retrieved from https://medlineplus.gov/ency/article/007392.htm MedlinePlus