Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we understand the worries about unusual skin changes, swelling, or leg pain. These signs might point to arteriovenous malformations (AVMs). AVMs are abnormal tangles of blood vessels that mess with normal blood flow.
AVMs let blood flow straight from arteries to veins, skipping capillaries. This can cause skin color changes, swelling, and pain in the affected limb.
We’re dedicated to giving top-notch, patient-focused care for those with AVMs. Our team is skilled in diagnosing and treating these rare vascular conditions. We make sure patients get all the support and treatment they need.
Key Takeaways
- Arteriovenous malformations (AVMs) are abnormal blood vessel tangles.
- AVMs can cause skin changes, swelling, and leg pain.
- Disrupted blood flow can lead to various complications.
- Liv Hospital provides expert diagnosis and treatment for AVMs.
- Patient-centered care is our top priority.
Understanding Arteriovenous Malformations (AVMs)
Arteriovenous malformations, or AVMs, are serious vascular problems. They can greatly affect a person’s health and life quality. We will dive into what AVMs are, starting with their basic features.
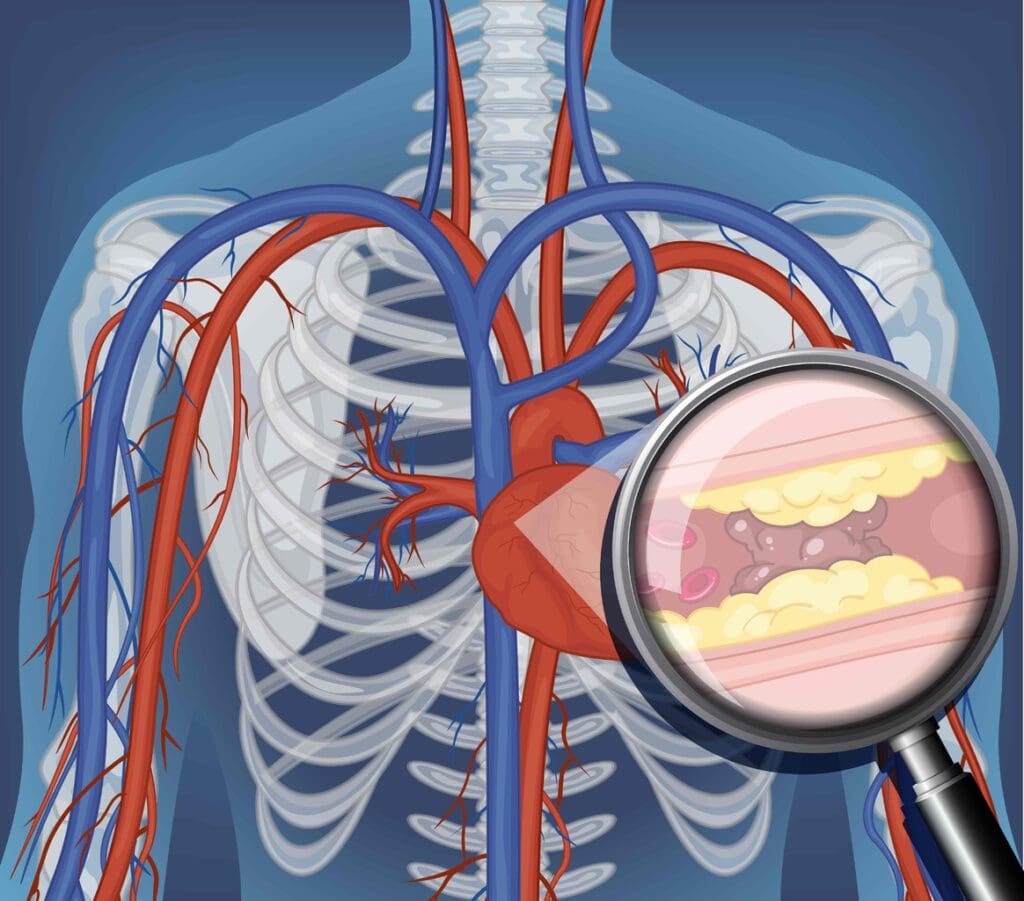
Definition and Basic Anatomy
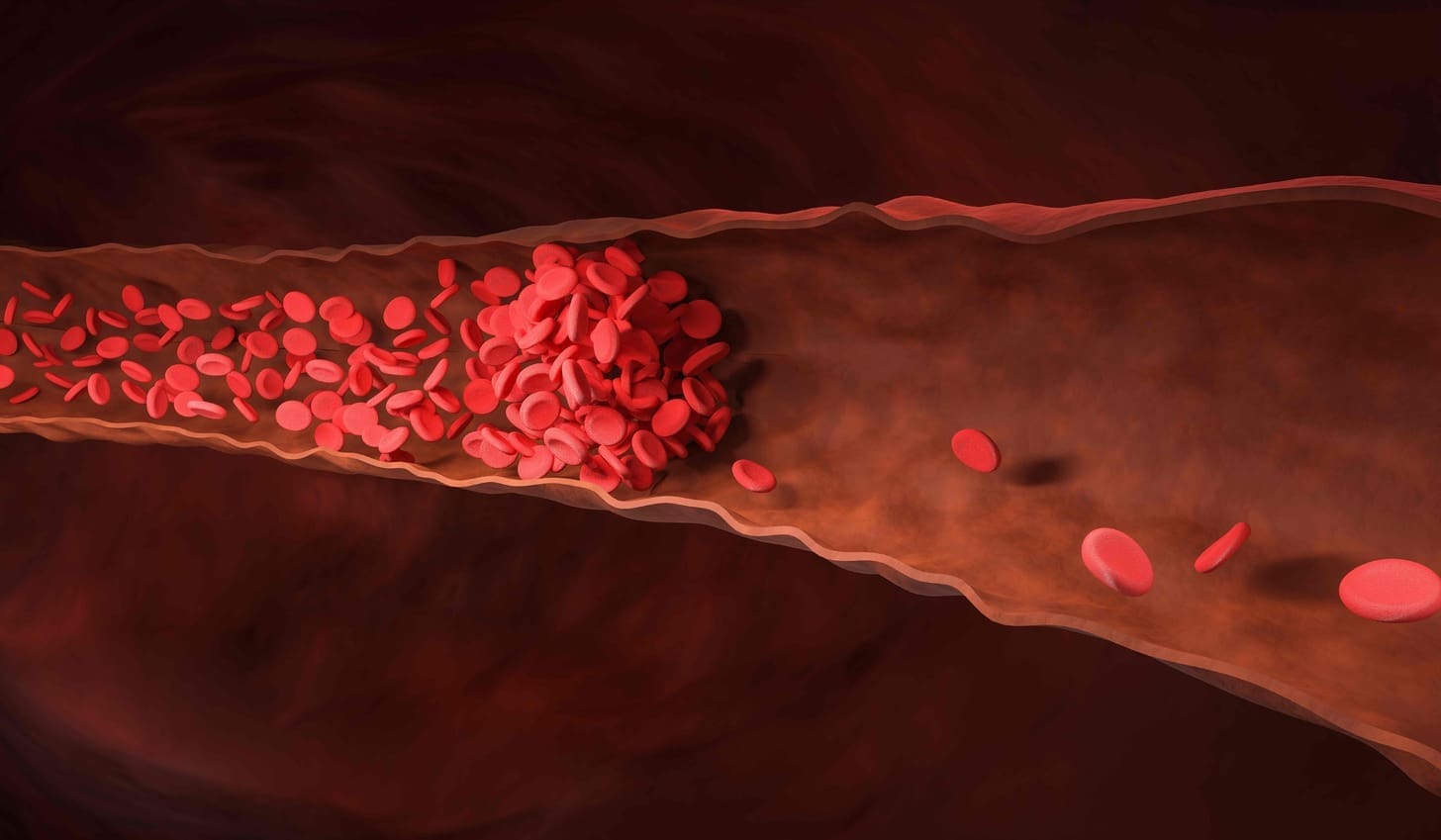
An AVM is a problem with blood vessels. Arteries connect directly to veins, skipping capillaries. This can cause health issues because it messes with blood and oxygen flow to tissues.
Normally, arteries carry oxygen-rich blood to the body, and veins bring back oxygen-poor blood to the heart. But with an AVM, the direct connection can cause blood flow problems. This can lead to serious vascular issues.
Normal Blood Vessel Structure vs. AVMs
In a healthy body, blood goes from arteries to capillaries. In capillaries, oxygen and nutrients are exchanged for waste. Then, blood moves to veins. AVMs skip this step, which can cause tissue problems or other issues.
| Characteristics | Normal Blood Vessels | AVMs |
|---|---|---|
| Blood Flow Pathway | Arteries → Capillaries → Veins | Arteries directly to Veins |
| Oxygen Delivery | Efficient oxygen delivery to tissues | Potential for reduced oxygen delivery due to shunting |
| Complications | Rarely associated with vascular anomalies | Risk of bleeding, ischemia, and other vascular issues |
What Does AVM Stand For in Medical Terms
In medical terms, AVM means Arteriovenous Malformation. It’s a condition where arteries and veins connect abnormally. This can lead to health problems. Knowing what AVM means is key for patients and doctors to understand and treat it.
We’ve covered the basics of AVMs. We’ve looked at their definition, how they differ from normal blood vessels, and what AVM means in medical terms. This knowledge is important for talking about AVM causes, symptoms, and treatments.
What Is Arteriovenous Malformation: Causes and Risk Factors
Arteriovenous malformations (AVMs) come from a mix of genetic, environmental, and developmental factors. Knowing these causes helps us understand why AVMs happen and how to prevent them.
Developmental Origins of AVMs
AVMs start in the early stages of development. Abnormal vascular development leads to AVMs, where arteries connect directly to veins. This can happen in the brain, spine, and limbs.
Studies show AVMs often come from mistakes in angiogenesis, the making of new blood vessels. Genetic mutations or environmental factors might cause these mistakes.
Are AVMs Genetic?
Most AVMs happen by chance, but genetics might play a part in some cases. Certain genetic disorders, like Hereditary Hemorrhagic Telangiectasia (HHT), increase AVM risk. HHT causes AVMs in organs like the lungs, liver, and brain.
- Genetic mutations affecting vascular development
- Family history of AVMs or HHT
- Presence of multiple AVMs
This shows genetics might influence AVMs, but we don’t know all the details.
Environmental Factors and Triggers
Genetics isn’t the only factor. Trauma or injury to a blood vessel can also cause AVMs. Chemicals or radiation might play a role too, but we need more research.
“The exact causes of arteriovenous malformations remain unclear, but it is likely that both genetic and environmental factors play a role.”
Knowing what causes AVMs is key for early detection and treatment. By spotting high-risk individuals, doctors can take steps to prevent AVMs.
Types of AVMs Based on Location
It’s important to know where AVMs happen to treat them right. Arteriovenous malformations can show up in different parts of the body. Each place has its own set of problems and signs.
Brain and Spinal Cord AVMs
AVMs in the brain or spinal cord are very risky. They can hurt the nervous system. Symptoms include seizures, headaches, and muscle weakness.
Treatment might include embolization, surgery, and radiation therapy.
Skin AVMs (Cutaneous AVMs)
Skin AVMs, or cutaneous AVMs, are visible on the skin. They can look scary and cause pain or discomfort. Treatment depends on the size and where the AVM is.
Extremity AVMs (Leg and Arm)
AVMs in the legs or arms can cause pain, swelling, and trouble moving. AVM leg cases can make walking hard. Arm avm can make it hard to use your hands.
| Location | Common Symptoms | Treatment Options |
|---|---|---|
| Brain and Spinal Cord | Seizures, Headaches, Muscle Weakness | Embolization, Surgery, Radiation Therapy |
| Skin (Cutaneous) | Visible Lesions, Discomfort, Pain | Sclerotherapy, Surgical Removal |
| Extremities (Leg and Arm) | Pain, Swelling, Limited Mobility | Embolization, Compression Therapy, Surgery |
| Internal Organs (Heart, Lungs, Liver) | Varies by Organ (e.g., Heart: Heart Failure; Lungs: Hemoptysis) | Embolization, Surgical Intervention, Monitoring |
Internal Organ AVMs (Heart, Lungs, Liver)
AVMs in the heart, lungs, and liver are tricky because they’re in important places. For example, an avm heart can lead to heart failure. Treatment needs a team of experts in cardiology, pulmonology, and hepatology.
We know AVMs need careful treatment, no matter where they are. Our team offers personalized care and advanced treatments to manage AVMs well.
Arteriovenous Malformation in the Skin: Characteristics and Symptoms
Arteriovenous malformations (AVMs) in the skin can be challenging due to their visibility and complications. We will look at the characteristics, symptoms, and complications of skin AVMs. This will give a full understanding of this condition.
Visual Appearance of Skin AVMs
Skin AVMs appear as discolored, swollen lesions that feel warm. They come in different sizes and may pulse due to abnormal blood flow. The look of these lesions can affect a person’s self-esteem and quality of life.
Common Symptoms of Cutaneous AVMs
People with cutaneous AVMs may feel pain, swelling, and bleeding from the lesion. Symptoms can vary from mild to severe. Some may just feel a little discomfort, while others may find it hard to do daily activities.
Progression and Complications of Skin AVMs
Skin AVMs can get worse over time, leading to more pain, bleeding, or ulcers. The risk of these complications increases if the AVM is damaged or not managed well. Knowing about these risks is key to managing and treating the condition effectively.
| Complication | Description | Management |
|---|---|---|
| Bleeding | AVMs can bleed due to their fragile structure. | Apply pressure; seek medical attention if severe. |
| Pain | Pain can occur due to the AVM or its complications. | Manage with pain relief medications; consider interventions. |
| Ulceration | Skin breakdown can occur over the AVM. | Wound care; protect the area from further trauma. |
Bleeding AVMs in the Skin
Bleeding is a big worry for those with skin AVMs. The blood vessels in the AVM are fragile and can easily break, causing bleeding. It’s important to manage bleeding well to avoid more problems and keep the person safe.
We’ve talked about the characteristics, symptoms, and complications of arteriovenous malformations in the skin. Knowing these details is vital for managing the condition and improving the lives of those affected by skin AVMs.
AV Malformation in Leg: Presentation and Complications
It’s important to know about leg AVMs to manage and treat them well. Leg AVMs can show up in different ways. They can affect your health and how you live your life.
Symptoms Specific to Leg AVMs
Leg AVMs can cause a variety of symptoms. These include:
- Pain or discomfort, often when you’re active
- Swelling or getting bigger in the affected limb
- Visible varicose veins or a mass you can feel
- Skin discoloration or ulcers in severe cases
These symptoms can get worse if the AVM isn’t treated.
Impact on Mobility and Daily Activities
An AVM in the leg can really affect how you move and do daily tasks. Pain and swelling can make it hard to move. We aim to help improve your life by addressing these symptoms.
Complications of Untreated Leg AVMs
Untreated leg AVMs can lead to serious problems. These include:
- Chronic pain from the constant strain
- Infection or skin ulcers over the AVM
- Heart failure in severe cases due to extra heart work
These issues show why treatment is so important.
Risk of AVM Rupture in the Leg
One big risk with leg AVMs is rupture. This can cause a lot of bleeding. Rupture risk is a big worry that needs careful watching and sometimes action to prevent it.
We know how complex and risky leg AVMs are. We’re dedicated to giving full care and support to those with this condition.
Diagnosis of Arteriovenous Malformations
To find AVMs, doctors use many methods. They start with a physical check and then use advanced imaging.
Physical Examination Findings
First, doctors do a physical check. They look for signs like swelling, color changes, or a lump. If the AVM is close to the skin, it might look red or purple.
They also check for pain, tenderness, or a sound called a bruit. This sound means blood is flowing strangely.
Imaging Techniques
Imaging is key in finding AVMs. The main tools are:
- Magnetic Resonance Imaging (MRI): MRI gives clear pictures of soft tissues. It shows how big the AVM is and where it is.
- Angiography: This method uses a contrast agent to see blood vessels. It helps find the AVM’s feeding and draining points.
- Computed Tomography (CT) Scan: CT scans show the AVM’s size and location. They also check for bleeding.
- Ultrasound: Doppler ultrasound looks at blood flow in the AVM. It spots any problems.
Differential Diagnosis
It’s important to rule out other conditions that look like AVMs. These include hemangiomas and vascular malformations. A detailed check-up is needed for the right diagnosis and treatment.
Doctors look at the patient’s history, symptoms, and imaging results. This helps them tell AVMs apart from other issues. It also helps plan the best treatment.
Treatment Options for AVMs
Managing AVMs requires different treatments, from simple monitoring to more complex procedures. The right treatment depends on the AVM’s location, size, and depth. It also depends on the patient’s health.
Conservative Management Approaches
For some, watching the AVM closely is the best first step. This means regular imaging to check its size and activity. It also includes managing symptoms like pain.
Conservative management strategies may include:
- Regular check-ups with a healthcare provider
- Imaging studies (e.g., MRI, CT scans) to monitor the AVM
- Managing pain with medication or other methods
Embolization of AVM
Embolization is a less invasive way to stop blood flow to the AVM. It involves injecting materials to block the blood vessels. This reduces the risk of rupture or complications.
Benefits of embolization include:
- Lower risk of bleeding
- Less invasive, leading to quicker recovery
- Can be used with other treatments
Surgical Interventions
Surgery is considered for AVMs that are easily reached and pose a high risk. Removing the AVM surgically can cure it but comes with risks. These include damage to nearby tissues.
| Surgical Approach | Benefits | Risks |
|---|---|---|
| Open surgery | Can be curative | Risk of damage to surrounding tissues |
| Microsurgery | High precision | Technically challenging |
Radiation Therapy for AVMs
Radiation therapy, or radiosurgery, uses high doses of radiation to damage AVM blood vessels. This leads to their closure. It’s often used for AVMs that are hard to treat with surgery or embolization.
Advantages of radiation therapy include:
- Non-invasive
- Effective for AVMs in sensitive or hard-to-reach locations
- Can be used when other treatments are not feasible
Living with AVMs: Management and Quality of Life
Living with an arteriovenous malformation (AVM) can be tough. But, with the right strategies, you can improve your life quality. Managing an AVM well means tackling it from all angles.
Pain Management Strategies
Pain is a big issue for AVM patients, often due to the size or location of the malformation. It’s key to manage pain well to keep your life quality up. We suggest a mix of methods for pain control, including:
- Medications: Over-the-counter or prescription drugs can help with pain.
- Lifestyle adjustments: Avoiding pain triggers and gentle exercises can help.
- Alternative therapies: Acupuncture or physical therapy might offer relief.
Preventing Complications
Stopping complications is vital in AVM management. This means watching for signs of rupture or other serious issues and taking steps to avoid them. We recommend:
- Regular check-ups with your doctor to keep an eye on the AVM.
- Staying away from contact sports or activities that could cause injury.
- Knowing the signs of serious complications, like a bad headache or changes in your brain function.
Here’s a table showing some complications and how to manage them:
| Complication | Signs and Symptoms | Management |
|---|---|---|
| Rupture | Severe headache, nausea, vomiting, neurological deficits | Immediate medical attention, possible surgery or embolization |
| Heart Failure | Shortness of breath, fatigue, swelling in legs | Medical management with diuretics, lifestyle changes |
Psychological Impact and Support
AVMs can affect your mind, causing anxiety, depression, and stress. It’s important to tackle these to stay well. We suggest:
- Getting help from mental health experts.
- Joining support groups to meet others with AVMs.
- Trying stress-reduction methods like meditation or yoga.
When to Seek Emergency Care
It’s vital for AVM patients to know when to get emergency help. Look out for these signs:
- Sudden severe headache.
- Weakness or numbness in parts of your body.
- Confusion or trouble speaking.
By knowing how to manage your AVM and when to seek help, you can live a better life despite the challenges.
Research and Future Directions in AVM Treatment
Research is leading the way in treating arteriovenous malformations (AVMs). The field is growing fast, thanks to new medical tech, genetic studies, and clinical trials.
Emerging Therapies and Clinical Trials
New treatments are being created to help AVM patients. Embolization techniques are getting better, making treatments more precise. Clinical trials are testing new materials and methods.
Researchers are working on targeted therapies for AVMs. These aim to lower risks and improve results for patients.
Genetic Research in AVM Development
Genetic studies are key to understanding AVMs. They’re finding genetic markers linked to AVM risk. This could mean earlier detection and treatment.
Scientists are looking into genetic therapies for AVMs. They hope to find treatments that target the condition’s root cause.
Specialized Treatment Centers and Expert Care
Specialized treatment centers are vital. They have teams of experts for AVM care. Patients get full support from diagnosis to aftercare.
As research moves forward, AVM treatment will get better. Healthcare will offer the latest and best treatments to patients.
Conclusion: Understanding and Managing Arteriovenous Malformations
Arteriovenous malformations (AVMs) are complex conditions that need a deep understanding and a careful management plan. We’ve looked at what AVMs are, their symptoms, how they’re diagnosed, and treatment options. Knowing about AVMs is key to managing them well. It helps doctors create treatment plans that fit each patient’s needs.
Handling AVMs well means working together. Specialists from fields like radiology, surgery, and rehabilitation are all involved. This team effort helps patients deal with AVM challenges and live better lives. Understanding AVMs and managing them requires a detailed and thoughtful approach.
As we learn more about AVMs, we can find better ways to treat them. This means better care and support for patients. With the right care, patients can manage their AVMs and enjoy a better life.
FAQ
What does AVM stand for in medical terms?
AVM stands for Arteriovenous Malformation. It’s a condition where blood vessels are tangled. This lets blood flow from arteries to veins, skipping capillaries.
Are AVMs genetic?
Some AVMs might be linked to genetics. But most cases happen without a known cause. Researchers are studying the risk factors.
What are the symptoms of a skin AVM?
Skin AVMs can show up as a visible lesion or mass. They might cause pain, swelling, and bleeding. They often look red or purple.
How are AVMs diagnosed?
Doctors use a physical exam, MRI, or angiography to diagnose AVMs. They also compare symptoms to rule out other conditions.
What are the treatment options for AVMs?
Treatment depends on the AVM’s location and size. Options include watching it, embolization, surgery, or radiation therapy.
What is embolization of an AVM?
Embolization is a procedure where materials block blood flow in the AVM. It aims to reduce symptoms and shrink the malformation.
Can AVMs rupture, and what are the risks?
Yes, AVMs can rupture, causing bleeding. The risk depends on the AVM’s location and size. Rupture can lead to severe bleeding.
How do AVMs in the leg affect mobility?
Leg AVMs can cause pain, swelling, and mobility issues. The impact on daily life depends on the AVM’s size and location.
What is the role of MRI in diagnosing AVMs?
MRI is key for diagnosing AVMs. It shows detailed images of the malformation. This helps doctors assess its size and location.
Are there any emerging therapies for AVM treatment?
Yes, new treatments for AVMs are being researched. Advances in genetics might also help manage AVMs better.
How can individuals with AVMs manage their condition?
Managing AVMs involves pain control, preventing complications, and addressing mental health. Knowing when to seek emergency care is also important.
- REFERENCES
- MedlinePlus. Arteriovenous Malformations (AVMs). Retrieved from https://www.medlineplus.gov/arteriovenousmalformations.html MedlinePlus
- NORD (National Organization for Rare Disorders). Arteriovenous Malformation. Retrieved from https://rarediseases.org/rare‑diseases/arteriovenous‑malformation rarediseases.org





