Last Updated on November 13, 2025 by
Childhood leukemia is a complex condition that needs a detailed approach. Advances in medical therapies have greatly improved survival rates. This change has given hope to patients all over the world. We use a mix of therapies to tailor treatment to each child’s specific needs.
Our treatment plan includes multi-agent chemotherapy, immunotherapy, targeted therapy, and sometimes bone marrow transplantation. These treatments are designed to effectively manage the disease while keeping side

effects low. By combining different therapies, we aim to give the best results for children with leukemia.
Key Takeaways
- Childhood leukemia treatment involves a combination of therapies.
- Multi-agent chemotherapy is a primary treatment modality.
- Immunotherapy and targeted therapy are also utilized.
- Bone marrow transplantation is considered in specific cases.
- Comprehensive care is key to improving survival rates.
Understanding Childhood Leukemia
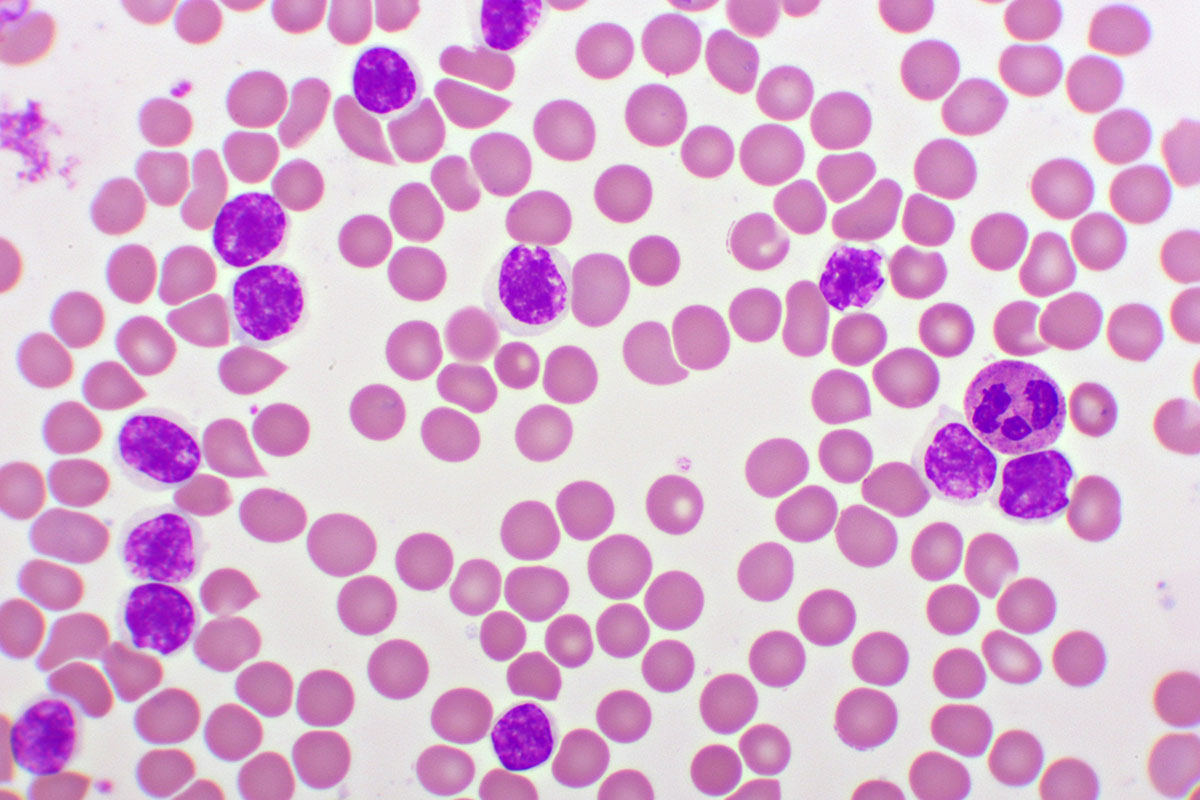
It’s important to know about childhood leukemia to catch it early and treat it well. This cancer affects the blood and bone marrow. It happens when abnormal white blood cells grow too much.
Types of Childhood Leukemia
There are two main types of childhood leukemia: acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). ALL is the most common, making up about 80% of cases. AML is less common. There are also rare types like chronic myeloid leukemia (CML) and juvenile myelomonocytic leukemia (JMML).

Each leukemia type has its own signs and treatment plans. For example, ALL has lymphoblasts in the bone marrow. AML has myeloid cells. Knowing these differences helps doctors choose the right treatment.
Prevalence and Incidence Trends
Childhood ALL has increased by 59% over 30 years. But thanks to better treatments, death rates have dropped a lot. The numbers change based on where people live and their genes.
Watching these trends helps us understand the disease better. It also helps us plan for research and treatment.
Signs and Symptoms
Spotting the signs of childhood leukemia early is key. Look for fatigue, pale skin, frequent infections, and easy bruising. Kids might also have bone pain, fever, and lose weight. These signs can be hard to spot.
Seeing a doctor right away is important. Early treatment can make a big difference in how well a child does.
Diagnosis of Childhood Leukemia
Diagnosing childhood leukemia is a detailed process. It involves several important steps. “Accurate diagnosis is the cornerstone of effective treatment for childhood leukemia,” as it allows healthcare providers to identify the specific type of leukemia and its characteristics.
Blood Tests and Initial Screening
The first step in diagnosing leukemia is a complete blood count (CBC) test. This test checks the levels of different blood cells. It looks at white blood cells, red blood cells, and platelets. If the results are abnormal, it might mean leukemia is present.
A leading medical expert says, “A CBC is a key initial test. It gives valuable insights into leukemia.”
“Early detection through blood tests can significantly improve treatment outcomes.”
Bone Marrow Aspiration and Biopsy
After the initial screening, a bone marrow aspiration and biopsy are done. This involves taking a sample of bone marrow for examination. It’s a key step in diagnosing leukemia. It lets doctors directly look at bone marrow cells.
- Helps in confirming the presence of leukemia cells
- Provides information on the type of leukemia
- Aids in understanding the extent of the disease
Genetic and Molecular Testing
Genetic and molecular testing are key in identifying the specific subtype of leukemia. They help understand its genetic characteristics. These tests help tailor the treatment plan to the child’s needs.
Genetic testing has changed leukemia diagnosis. It lets doctors offer targeted therapies. “Genetic testing has become an indispensable tool in the diagnosis and treatment planning of childhood leukemia.”
Staging and Risk Classification
Knowing the stage and risk of leukemia is key to the best treatment. Leukemia staging looks at how far and severe the disease is. This helps predict how well a patient will do and what treatment to use.
Classification Basis
Leukemia types are based on the cells affected, their maturity, and genetic changes. The system helps doctors understand how aggressive the disease is and how it might react to treatment. In kids, the main types are Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML). Each needs a different treatment plan.
Risk Stratification Process
The risk stratification process sorts patients into groups based on several factors. This is key for tailoring treatment intensity. Patients are usually put into standard, high, or intermediate risk groups. This guides the treatment plan.
Impact on Treatment Planning
The stage and risk of leukemia greatly affect treatment planning. Knowing the risk category helps doctors choose the right treatment intensity. This balances treatment effectiveness with side effect risks. This personalized approach has improved outcomes for kids with leukemia.
Accurate staging and risk classification are essential for managing childhood leukemia. By using these classifications, healthcare providers can create targeted treatment plans. These plans meet the unique needs of each patient.
Comprehensive Treatment for Leukemia in Children
We treat leukemia in children with a holistic approach. We use different therapies to get the best results. Treating leukemia in kids is complex and needs a plan that fits each child’s needs.
Treatment Protocol Development
Creating a treatment plan for childhood leukemia is detailed. We look at the leukemia type, risk level, and how the patient responds to treatment. Our team of experts works closely together to make a plan that works well and is safe.
- Assessment of leukemia type and stage
- Risk stratification to determine the intensity of treatment needed
- Selection of appropriate therapeutic agents and their dosages
Multidisciplinary Approach
A multidisciplinary team is key in treating childhood leukemia. Our team includes pediatric oncologists, hematologists, nurses, nutritionists, and more. They all work together to give complete care. This teamwork makes sure every part of a child’s health is looked after during treatment.
Treatment Phases
The treatment of leukemia in children goes through several phases. Each phase has its own goals and challenges. Knowing about these phases helps us manage expectations and give the right care.
- Induction phase: The first phase aims to get the leukemia into remission.
- Consolidation phase: This phase is to kill any leukemia cells left.
- Maintenance phase: This is ongoing treatment to stop the leukemia from coming back.
Understanding the treatment for leukemia in children helps us support our young patients and their families. This includes knowing about treatment plans, the team involved, and the different treatment phases.
Chemotherapy Protocols and Administration
Chemotherapy is key in treating childhood leukemia. It has evolved to better help kids. The success of chemotherapy depends on the leukemia type, the child’s health, and the treatment plan.
Multi-Agent Chemotherapy Approaches
Using a mix of drugs is the main way to treat childhood leukemia. This method attacks leukemia cells better than one drug alone. The drugs and doses are chosen based on the child and their leukemia type.
For example, chemotherapy protocols for Acute Lymphoblastic Leukemia (ALL) might include vincristine, prednisone, and asparaginase. This approach has greatly improved survival rates.
Administration Methods
Chemotherapy can be given in different ways, like orally, through an IV, or into the spinal fluid. The method chosen depends on the drugs and the child’s health.
IV administration is common. It sends the drugs straight into the blood. This helps the drugs reach all parts of the body to fight leukemia.
Managing Side Effects
It’s important to manage chemotherapy side effects to keep the child’s quality of life good. Side effects can include nausea, hair loss, tiredness, and a higher risk of infections.
To help, we use anti-nausea meds, nutrition support, and ways to prevent infections. We work with families to watch for and handle side effects. We adjust the treatment as needed to reduce discomfort and problems.
Understanding chemotherapy and how to manage side effects helps improve outcomes for kids with leukemia. Our team provides care that fits each child’s needs.
Targeted Therapy Approaches
Targeted therapy is key in treating childhood leukemia. It’s a precise way to fight the disease. This method targets specific molecular issues that make leukemia cells grow and live.
Molecular Targets in Pediatric Leukemia
In kids with leukemia, doctors have found certain genetic changes and proteins to target. For example, the BCR-ABL protein is a big target in some leukemia cases. Targeted therapy works to block these issues, stopping the disease from getting worse.
Types of Targeted Medications
There are many targeted medicines for childhood leukemia. Tyrosine kinase inhibitors (TKIs) like imatinib are a big deal. They stop the BCR-ABL tyrosine kinase, helping in CML and some ALL cases. Other treatments include monoclonal antibodies and immunotherapies that target leukemia cells.
As noted by a leading expert, “Targeted therapies have greatly improved treatment for some leukemia types. They offer new ways to fight the disease.”
Benefits and Limitations
Targeted therapy is good because it’s more precise. This can mean fewer side effects and less harm to healthy cells. But, there are downsides. These include the chance of the therapy not working and needing to keep taking it to keep the disease under control. We need to think carefully about using targeted therapy for kids with leukemia.
As
“Targeted therapies are a big step forward in treating leukemia. But, we need to really understand the disease to use them best.”
Immunotherapy Advancements
The field of childhood leukemia treatment is changing with immunotherapy. This method uses the body’s immune system to fight disease. It brings new hope to patients and their families.
CAR T-Cell Therapy
CAR T-cell therapy is a new way to treat leukemia. It changes a patient’s T-cells to attack leukemia cells. This innovative approach works well on some types of leukemia that other treatments can’t.
First, T-cells are taken from the patient. Then, they are changed to find and kill leukemia cells. This targeted approach helps avoid harming healthy cells.
Monoclonal Antibodies like Blinatumomab
Monoclonal antibodies, like blinatumomab, are another immunotherapy option. Blinatumomab helps T-cells find and kill leukemia cells. It’s shown great promise in treating acute lymphoblastic leukemia (ALL).
Using monoclonal antibodies like blinatumomab offers a targeted treatment option. It works differently than traditional chemotherapy. This could lead to fewer side effects and better results for patients.
Emerging Immunotherapeutic Approaches
Researchers are also looking into other immunotherapies. These include checkpoint inhibitors and vaccines. They aim to boost the immune system’s fight against cancer.
These new methods are in clinical trials. While they show promise, more research is needed. We must understand the benefits and risks of treating childhood leukemia.
Immunotherapy is transforming childhood leukemia care. It uses the immune system to improve treatment results. This brings hope to families dealing with this disease.
Stem Cell and Bone Marrow Transplantation
Bone marrow transplantation is an option for some kids with leukemia. It’s for those with high-risk or relapsed disease. This treatment replaces the patient’s bone marrow with healthy stem cells from a donor. It’s a chance for a cure when other treatments fail.
When Transplantation is Recommended
We suggest stem cell transplantation for kids with high-risk leukemia or those who have relapsed. The choice depends on the child’s health, the type, and how well they’ve done with previous treatments.
Key factors influencing the decision for transplantation include:
- The presence of certain genetic markers indicating high-risk disease
- Relapse after initial chemotherapy
- Inadequate response to initial treatment
Donor Selection Process
After deciding on transplantation, finding a good donor is key. We look for both related and unrelated donors. The goal is to find the best match to reduce the risk of graft-versus-host disease (GVHD).
The donor selection process involves:
- Tissue typing to identify compatible donors
- Cross-matching to ensure compatibility between the donor and recipient
- Evaluation of the donor’s overall health and suitability for donation
Transplantation Procedure and Recovery
The transplant starts with a conditioning regimen. This includes high-dose chemotherapy and sometimes radiation. It kills the patient’s existing bone marrow and leukemia cells.
Then, the patient gets the donor’s stem cells through an intravenous infusion. This is like a blood transfusion.
After a transplant, care is vital for recovery. It includes:
- Monitoring for signs of GVHD
- Managing side effects like infection and organ damage
- Supportive care, like nutrition and counselling
Recovery from stem cell transplantation takes time. It requires ongoing care to manage issues and help the child get better.
Treatment Outcomes and Survival Rates
Childhood leukemia treatment has greatly improved over time. Thanks to medical research and new treatments, more kids are surviving leukemia.
Current Survival Statistics
The 5-year survival rate for Acute Lymphoblastic Leukemia (ALL) is now over 90%. This is due to better chemotherapy, targeted therapy, and care. Many kids with leukemia are now living long, healthy lives.
Recent data shows that kids with ALL have a high survival rate. This success is thanks to modern medicine and the hard work of doctors and nurses.
Factors Affecting Prognosis
Several things can change a child’s leukemia prognosis. These include:
- Age at Diagnosis: Kids between 1 and 9 usually do better.
- Genetic Factors: Some genetic issues can affect the outcome.
- Response to Initial Treatment: A good response to the first treatment is hopeful.
- Type of Leukemia: ALL is more treatable than Acute Myeloid Leukemia (AML).
Long-term Follow-up Care
After leukemia treatment, kids need ongoing care. This includes watching for late effects like second cancers and heart issues. Regular doctor visits help catch and manage these problems early.
It’s key to have a detailed follow-up plan. This might include:
- Regular visits with doctors and specialists.
- Screenings and tests for late effects.
- Support to help with physical, emotional, and mental health.
By focusing on long-term care, we help kids who beat leukemia live happy, healthy lives.
Complementary Approaches and Supportive Care
Supportive care is key in managing leukemia treatment side effects and improving life quality for kids. It’s important to look at the whole child, including their physical, emotional, and nutritional needs.
Nutritional Support During Treatment
Nutritional support is vital for kids with leukemia. Good nutrition helps them get through treatment better, recover faster, and stay healthy. A well-balanced diet with fruits, veggies, whole grains, and lean proteins is best. But treatment can make it hard for kids to eat well.
“Good nutrition is key for kids with leukemia,” says a pediatric oncologist. “It helps them deal with treatment side effects and recover better.” Getting help with nutrition can really help a child’s treatment journey.
Managing Treatment Side Effects
It’s important to manage leukemia treatment side effects to keep a child’s quality of life up. Side effects can be anything from nausea and tiredness to serious issues like infections or bleeding. Managing side effects includes medicine, lifestyle changes, and other therapies. For example, nutrition can help with some side effects, and pain management can reduce pain.
- Nutritional counselling to manage eating difficulties
- Pain management through medication and alternative therapies
- Infection prevention measures, including hygiene practices and prophylactic antibiotics
Integrative Therapies and Quality of Life
Integrative therapies like acupuncture, massage, and mind-body therapies can greatly improve a child’s quality of life with leukemia. They help manage side effects, reduce stress, and improve overall well-being. It’s important to add these therapies to the treatment plan with healthcare professional guidance.
By adding complementary approaches and supportive care to treatment plans, we can offer kids with leukemia better care. As we keep improving medical treatments, focusing on supportive care is just as important. It makes a big difference in a child’s journey through leukemia treatment.
Conclusion: The Future of Childhood Leukemia Treatment
Looking at childhood leukemia treatment today, we see big steps forward. New therapies like blinatumomab have opened up more options. This has led to better survival rates for kids.
Research and clinical trials keep pushing the boundaries of leukemia treatment. We’re committed to top-notch healthcare and support for our patients. This ensures they get the best care and quality of life.
We’re excited about the future of treating leukemia in kids. With ongoing research, we’re hopeful for even better care and outcomes. Our goal is to provide the best care, tailored to each child’s needs.
FAQ’s:
What is the treatment for leukemia in children?
What are the different types of childhood leukemia?
How is childhood leukemia diagnosed?
What is the role of chemotherapy in treating childhood leukemia?
What is targeted therapy, and how is it used in childhood leukemia treatment?
How does immunotherapy work in treating childhood leukemia?
When is stem cell or bone marrow transplantation recommended for childhood leukemia?
What are the current survival statistics for childhood leukemia?
How can I support my child during leukemia treatment?
Are there any alternative or complementary therapies for childhood leukemia?
How do you treat leukemia naturally?
Is there a cure for leukemia?
What are the signs and symptoms of childhood leukemia?
How is leukemia staged and classified?
What is the role of a multidisciplinary team in childhood leukemia treatment?
References
- Surveillance, Epidemiology, and End Results (SEER) Program. (2025). Cancer Stat Facts: Leukemia. https://seer.cancer.gov/statfacts/html/leuks.html
- Shimony, S., et al. (2025). Acute Myeloid Leukemia: 2025 Update on Diagnosis, Risk Classification, and Management. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC11966364/
- Siegel, R. L., et al. (2025). Cancer statistics, 2025. CA: A Cancer Journal for Clinicians. https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21871





