We dive into the complex world of hematopoiesis, the creation of blood cells. This process is key to our health. Hematopoietic stem cells (HSCs) are essential for making all blood cell types. Knowing what triggers HSCs is critical for finding new treatments for blood diseases.
Studies reveal that many things can activate HSCs. These include growth factors, cytokines, and interactions in the bone marrow. Together, they control hematopoietic stem cell differentiation. This ensures we get healthy blood cells.
Key Takeaways
- Hematopoietic stem cells are vital for blood cell creation.
- Growth factors and cytokines stimulate HSCs.
- The bone marrow microenvironment is key in regulating HSCs.
- Understanding HSC stimulation is vital for new therapies.
- Dysregulation of HSCs can cause various blood disorders.
The Biology of Hematopoietic Stem Cells
Understanding hematopoietic stem cells is key to knowing how our bodies make blood cells. These cells are vital for our health. Hematopoietic stem cells (HSCs) can make all blood cell types. They help keep the right balance of blood cells in our body.
Definition and Unique Properties
Hematopoietic stem cells are multipotent cells. They can grow into both myeloid and lymphoid lineages. They can also self-renew, making sure we always have blood cells. Plus, they can turn into different blood cell types, like red blood cells and immune cells.
These cells are important in hematopoiesis, the making of blood cells. This process is key for replacing old blood cells with new ones.
Historical Discovery and Research Milestones
The discovery of HSCs was a big step in hematology. Research on HSCs has helped us understand how blood cells are made. It has also led to new treatments for blood disorders.
Important research milestones include finding HSCs in the bone marrow. We learned they are key in making blood cells. They help repopulate blood cell lines after bone marrow transplants.
| Research Milestone | Description | Year |
| Identification of HSCs in Bone Marrow | Researchers found HSCs as the main cells for blood cell production in the bone marrow. | 1961 |
| Elucidation of HSC Role in Hematopoiesis | Studies showed how HSCs turn into different blood cell types. | 1970s |
| Bone Marrow Transplantation Advances | Improvements in bone marrow transplants showed HSCs’ role in repopulating blood cell lines. | 1980s |
Understanding Hematopoiesis: From Stem Cells to Blood Cells
Hematopoiesis is key to knowing how stem cells make blood cells all our lives. It’s a complex process that turns stem cells into different blood cells. This process is tightly controlled and vital for our health.
Stages of Blood Cell Development
Blood cells start from stem cells in several steps. First, stem cells turn into progenitor cells. Then, these cells decide which blood cell type to become. They can become red blood cells, platelets, or white blood cells.
The blood cell development stages are:
- Hematopoietic stem cells self-renew or differentiate into multipotent progenitor cells.
- Multipotent progenitor cells give rise to lineage-restricted progenitors.
- Lineage-restricted progenitors mature into specific blood cell types.
| Stage | Description | Cell Types Involved |
| 1 | Hematopoietic stem cell self-renewal or differentiation | Hematopoietic stem cells |
| 2 | Formation of multipotent progenitor cells | Multipotent progenitor cells |
| 3 | Lineage commitment and maturation | Lineage-restricted progenitors, mature blood cells |
Locations of Hematopoiesis Throughout Life
Hematopoiesis happens in different places at different times. In the womb, it starts in the yolk sac. It then moves to the liver and eventually to the bone marrow in adulthood.
The bone marrow is a special place for blood cell production. It supports stem cells and their growth. Knowing where hematopoiesis happens helps us understand how blood cells are made.
The Anatomical Niches Where Hematopoietic Stem Cells Reside
Hematopoietic stem cells live in special places called niches. These niches help them survive, grow, and change into different types of blood cells. The niches have a complex mix of cells and molecules that control how HSCs behave.
Bone Marrow Microenvironment
The bone marrow is where blood cells are made in adults. It’s a special place that helps HSCs stay healthy and work right. The bone marrow has many different cells, like osteoblasts and endothelial cells, that work together to control HSCs.
Extramedullary Hematopoiesis Sites
While the bone marrow is the main place for blood cell making, other organs can also make blood under certain conditions. The liver and spleen can help make blood during fetal development or when the body is sick.
| Organ | Role in Hematopoiesis | Conditions Supporting Extramedullary Hematopoiesis |
| Liver | Primary site during fetal development | Myelofibrosis, certain hematological malignancies |
| Spleen | Can support hematopoiesis in adults under pathological conditions | Myeloproliferative neoplasms, severe hemolytic anemia |
Knowing where hematopoietic stem cells live is key to finding new treatments. These treatments aim to help HSCs work better for patients.
Cellular Hierarchy and Differentiation Pathways
Understanding how hematopoietic stem cells develop into blood cells is key. These stem cells can turn into all blood cell types. This happens through a complex mix of cellular and molecular steps.
The journey of HSCs to mature blood cells is tightly controlled. They move through different stages of growth. This journey leads to two main paths: the myeloid and lymphoid lineages.
Myeloid Lineage Development
The myeloid lineage produces several blood cell types. These include monocytes, macrophages, and others. The growth of these cells is guided by various factors and cytokines.
- Myeloid Progenitor Cells: These cells are the precursors to the various myeloid-derived blood cells.
- Granulocyte-Macrophage Colony-Stimulating Factor (GM-CSF): This factor is key for granulocytes and macrophages.
- Erythropoietin (EPO): EPO is essential for erythrocyte production.
Lymphoid Lineage Development
The lymphoid lineage creates lymphocytes, like T cells and B cells. These cells are vital for our immune system.
- Lymphoid Progenitor Cells: These cells develop into lymphoid-derived cells.
- Interleukins (ILs): Interleukins play a role in lymphocyte development and function.
The difference between myeloid and lymphoid lineages is key to understanding blood cell development. The complex interactions of transcription factors, signaling pathways, and cell interactions guide HSCs into these distinct paths.
Growth Factors That Stimulate Hematopoietic Stem Cells
It’s important to know how growth factors help hematopoietic stem cells. These cells make all blood cell types. They keep our blood healthy. Growth factors help these cells grow and work right.
Stem Cell Factor (SCF)
Stem Cell Factor (SCF) is key for HSCs. It helps them live, grow, and stay healthy. SCF works with c-Kit to help HSCs thrive. Without it, blood problems can happen.
Thrombopoietin (TPO)
Thrombopoietin (TPO) is important for HSCs, too. It helps make platelets and keeps HSCs healthy. TPO works with c-Mpl to help HSCs grow and renew themselves.
Flt3 Ligand and Its Effects
Flt3 ligand helps HSCs and their early forms grow. It binds to Flt3, helping them live and grow. It’s used to help blood production, like in stem cell transplants.
These growth factors work together with HSCs in a complex way. Knowing how they work is key to helping blood production. They help keep our blood healthy by controlling HSCs.
Cytokines as Powerful Regulators of Hematopoietic Stem Cell Activity
Cytokines play a big role in how hematopoietic stem cells grow, change, and live. These molecules help stem cells talk to their environment. This is key for making blood cells.
Interleukins in Stem Cell Regulation
Interleukins are important for controlling hematopoietic stem cells. They help these cells grow and turn into different blood cells. Interleukin-3 (IL-3) helps many blood cell types, while Interleukin-6 (IL-6) helps with inflammation.
Interleukins shape the HSC niche, affecting both stem cells and their environment. If they’re not working right, it can cause blood problems. This shows how critical they are for stem cell control.
Colony-Stimulating Factors (CSFs)
Colony-Stimulating Factors are key for blood cell development. Granulocyte-CSF (G-CSF) and Granulocyte-Macrophage CSF (GM-CSF) help make certain blood cells. Doctors use them to help blood counts after chemo.
We use CSFs to help blood cells recover and to get stem cells ready for transplants. They’re important for making specific blood cells.
Erythropoietin (EPO) and Thrombopoietin (TPO)
Erythropoietin (EPO) and Thrombopoietin (TPO) control making red blood cells and platelets, respectively. EPO helps make red blood cells, and TPO helps make platelets. They keep these cell types in balance.
We use EPO and TPO to treat low red blood cells and platelets. Their specific jobs show how complex cytokine control is in making blood cells.
Hormonal Influences on Hematopoietic Stem Cell Function
Hormones are key in controlling hematopoietic stem cells (HSCs). They affect how these cells work and the overall process of making blood cells. These effects are important in both healthy and sick states.
Sex Hormones: Estrogen and Testosterone
Sex hormones like estrogen and testosterone impact HSCs. Estrogen helps these cells grow and change, possibly by acting on estrogen receptors. Testosterone, in turn, plays a role in making red blood cells.
A recent study mentioned in a news article shows hormonal effects on blood cell production. This supports the idea that hormones greatly influence how blood cells are made.
| Hormone | Effect on HSCs | Mechanism |
| Estrogen | Influences proliferation and differentiation | Estrogen receptor-mediated |
| Testosterone | Affects erythropoiesis | Enhances red blood cell production |
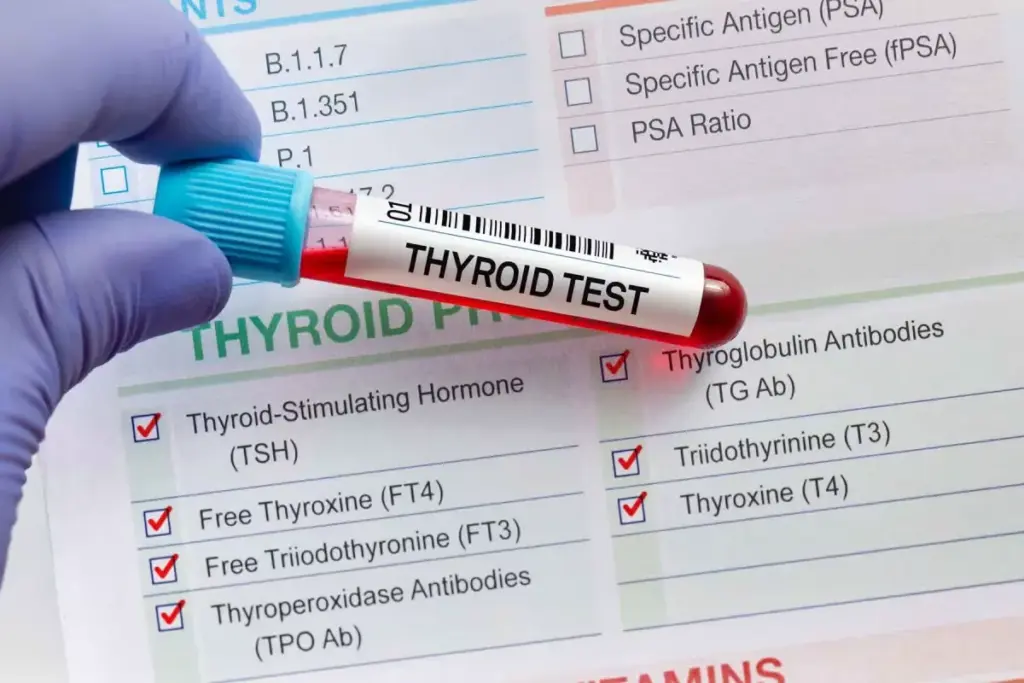
Thyroid Hormones and Their Impact
Thyroid hormones also affect HSCs. They control how fast cells work and help in the growth and function of cells, including HSCs.
“Thyroid hormones play a critical role in blood cell production. Changes in their levels can affect how many blood cells are made.”
Thyroid hormone receptors are found in HSCs and their descendants. This shows they directly control these cells.
Glucocorticoids and Stress Response
Glucocorticoids, like cortisol, are hormones released when we’re stressed. They help reduce inflammation and can affect HSCs, mainly in stress situations.
Long-term exposure to glucocorticoids can change how blood cells are made. This might affect the balance between different types of blood cells.
It’s important to understand how hormones influence HSCs to fully grasp blood cell production. More research into these hormonal effects could lead to new treatments for blood-related diseases.
The Microenvironment: Niche Factors That Stimulate Hematopoietic Stem Cells
Understanding what makes hematopoietic stem cells (HSCs) work is key to new treatments. The bone marrow’s environment, with its cells, matrix, and conditions, is vital. It helps control how HSCs behave.
Cell-to-Cell Interactions
In the bone marrow, HSCs talk to different cells. This includes osteoblasts, endothelial cells, and mesenchymal stem cells. They get important signals that help them stay the same or change into other cells.
These talks happen through special molecules and pathways. For example, HSCs and osteoblasts need each other to stay in a resting state. Endothelial cells also help by sending out signals that guide HSCs.
Extracellular Matrix Components
The bone marrow’s matrix gives HSCs a place to stand and sends them messages. It’s made of things like collagen, laminin, and fibronectin. These interact with HSCs, affecting how they stick, move, and change.
The matrix also holds onto growth factors and cytokines. When needed, it releases them to help control HSCs. The matrix’s makeup and structure are important for HSC health.
Oxygen Tension and Hypoxic Regulation
Oxygen levels are important for HSCs in the bone marrow. They live in low-oxygen areas, which helps them stay stem cells and not turn into other cells.
Hypoxia-inducible factors (HIFs) help HSCs adjust to low oxygen. They control genes for making blood vessels, using glucose, and surviving. This keeps HSCs healthy in low-oxygen conditions.
| Microenvironmental Factor | Role in HSC Regulation | Key Mechanisms |
| Cell-to-Cell Interactions | Regulates HSC self-renewal and differentiation | Adhesion molecules, signaling pathways |
| Extracellular Matrix Components | Provides structural support and biochemical signals | ECM-HSC interactions, growth factor reservoir |
| Oxygen Tension | Maintains HSC stemness and prevents differentiation | Hypoxia-inducible factors, metabolic adaptation |
Molecular Signaling Pathways in Hematopoietic Stem Cell Regulation
Molecular signaling pathways are key in controlling hematopoietic stem cells (HSCs). They help keep HSCs in balance, ensuring they can renew, grow, and differentiate. This balance is vital for making blood cells throughout our lives.
Notch Signaling Pathway
The Notch signaling pathway is found in many living things. It’s important for deciding what HSCs will do next. Notch signaling helps HSCs stay the same and not turn into other cells. Studies show it’s active in the bone marrow, where HSCs live.
Wnt/β-catenin Pathway
The Wnt/β-catenin pathway is also vital for HSCs. It helps with self-renewal, growth, and survival. Wnt proteins bind to HSCs, leading to β-catenin moving into the cell’s nucleus. This pathway can help grow or keep HSCs, depending on how active it is.
Hedgehog and BMP Signaling
Hedgehog and BMP signaling are also important for HSCs. Hedgehog signaling helps HSCs stay the same and keeps them in their right place. BMP signaling, on the other hand, can make HSCs grow and change, working with other pathways.
| Signaling Pathway | Role in HSC Regulation | Key Effects |
| Notch Signaling | Promotes self-renewal, maintains undifferentiated state | Influences cell fate decisions |
| Wnt/β-catenin | Affects self-renewal, proliferation, survival | Context-dependent expansion or maintenance of HSCs |
| Hedgehog Signaling | Supports self-renewal, niche maintenance | Promotes HSC maintenance |
| BMP Signaling | Influences proliferation, differentiation | Coordination with other pathways for HSC regulation |
In conclusion, controlling HSCs is complex and involves many pathways. Understanding Notch, Wnt/β-catenin, Hedgehog, and BMP signaling is key. This knowledge is essential for creating new treatments to help HSCs for medical use.
Inflammatory Signals and Their Effect on Hematopoietic Stem Cells
The link between inflammation and hematopoietic stem cells is complex. It has big implications for blood diseases. Inflammation is key in fighting off infections and injuries. It deeply affects how HSCs work and behave.
Acute Inflammation Response
When the body faces injury or infection, it quickly responds with inflammation. This response sends out signals that change how HSCs grow and develop. Cytokines and growth factors are released, helping to quickly produce more blood cells. This is vital for fighting infections and starting the healing process.
Interleukins like IL-1 and IL-6 are important in this fight. They help control the inflammation and directly affect HSCs. This response is usually short-lived, stopping once the cause is gone.
Chronic Inflammation Consequences
But chronic inflammation is harmful to HSCs and the blood-making system. Long-term exposure to these signals can wear out the HSCs. This can lower blood cell production and may lead to blood disorders.
Chronic inflammation is linked to issues like anemia and blood cancers. It’s important to understand how it harms HSCs. This knowledge is key to finding ways to protect them.
Metabolic Regulators of Hematopoietic Stem Cell Function
Hematopoietic stem cells (HSCs) rely on their metabolism to work properly. They need a balance of metabolic processes to keep their stemness. This balance is key for their role in making blood cells.
Glucose Metabolism and Glycolysis
Glucose metabolism is vital for HSCs. Glycolysis turns glucose into pyruvate, helping HSCs stay stem-like. HSCs use glycolysis more than oxidative phosphorylation for energy. This keeps their ROS levels low and helps them self-renew.
Signaling pathways control glucose metabolism in HSCs. The PI3K/AKT pathway boosts glycolysis. HIF-1α also increases glycolytic gene expression, supporting HSCs’ glycolytic nature.
Fatty Acid Oxidation Pathways
Fatty acid oxidation (FAO) is key for HSC function. FAO helps keep HSCs in balance by providing energy and managing fatty acids. Studies show that better FAO in HSCs leads to better self-renewal and repopulating.
- Regulating FAO in HSCs involves activating CPT1a, a key FAO enzyme.
- The AMPK pathway also boosts FAO by activating downstream targets.
Amino Acid Metabolism and Protein Synthesis
Amino acid metabolism is vital for protein synthesis in HSCs. It involves complex pathways. For example, the mTOR pathway controls protein synthesis based on amino acid availability and energy status.
Glutamine and arginine are key for HSCs’ metabolic needs. Glutamine helps with nucleotide synthesis and redox balance. Arginine is important for cell growth and survival.
Physical and Mechanical Stimuli Affecting Hematopoietic Stem Cells
Hematopoietic stem cells (HSCs) are influenced by many factors. Physical and mechanical stimuli are key in this. They help control how HSCs work in the bone marrow.
Shear Stress from Blood Flow
Shear stress from blood flow is a big mechanical force on HSCs. It affects their growth, division, and change into different cell types. Studies have found that HSCs adjust their genes and actions based on shear stress. This adjustment is vital for keeping the right balance between HSC growth and change.
Biomechanical Forces in the Bone Marrow
Biomechanical forces in the bone marrow, like cell movement and matrix stiffness, also affect HSCs. These forces can change the HSC niche’s mechanical properties, influencing HSC behavior. For example, changes in matrix stiffness can impact HSC growth and self-renewal.
It’s important to understand how physical and mechanical stimuli affect HSCs. This knowledge can help us find ways to improve HSC function. By adjusting these stimuli, we might enhance HSC performance. This could lead to better results in stem cell transplantation and regenerative medicine.
Therapeutic Approaches to Stimulate Hematopoietic Stem Cells
New ways to help hematopoietic stem cells (HSCs) are being developed. These methods are key for better blood cell production and treating blood diseases.
Recombinant Growth Factors in Clinical Use
Recombinant growth factors have changed how we treat HSCs. They help HSCs grow and turn into different blood cells. For example, Stem Cell Factor (SCF) and Flt3 Ligand help HSCs grow and live longer.
Here’s a list of important growth factors used in treatments:
| Growth Factor | Function | Clinical Application |
| SCF | Supports HSC proliferation and survival | Bone marrow transplantation |
| Flt3 Ligand | Promotes HSC expansion | Treatment of hematological disorders |
| Thrombopoietin (TPO) | Regulates platelet production | Treatment of thrombocytopenia |
Small Molecule Stimulators
Small molecules are also being studied to boost HSCs. They work by changing important signals in HSCs. For example, SR1 helps HSCs grow by blocking a certain receptor.
Gene Therapy and CRISPR Approaches
Gene therapy and CRISPR/Cas9 are new ways to fix genetic blood diseases. They let us edit HSCs to fix genetic problems. CRISPR/Cas9 has been used to treat sickle cell anemia and beta-thalassemia.
These methods are very promising for treating blood disorders. As research grows, we expect even better ways to help HSCs.
Clinical Applications of Hematopoietic Stem Cell Stimulation
Hematopoietic stem cell stimulation is key in medical treatments. These cells are vital for making blood cells. Their stimulation helps in treating many diseases.
Bone Marrow Transplantation Procedures
Bone marrow transplants help treat blood cancers and disorders. Hematopoietic stem cell stimulation is essential. It helps the bone marrow recover faster.
Stimulating HSCs improves the success of transplants. This reduces complications and boosts patient recovery. A leading researcher says, “Stimulating hematopoietic stem cells is vital for bone marrow transplant success. It leads to quicker recovery and better graft function.”
Treatment of Hematological Disorders
Hematological disorders like anemia and leukemia need treatments that boost HSCs. This increases healthy blood cell production. It helps patients feel better and live better lives.
- Enhancing erythropoiesis to treat anemia
- Supporting the recovery of leukocytes after chemotherapy
- Promoting thrombopoiesis to prevent bleeding complications
Emerging Research in Hematopoietic Stem Cell Stimulation
New research is changing how we see HSC stimulation. We’re finding new ways to make HSCs work better. Several promising methods are now being studied.
Novel Growth Factors and Cytokines
Studies have found novel growth factors and cytokines that help control HSCs. These can be used to help HSCs grow and work better. For example, Flt3 ligand has been shown to help HSCs grow and stay healthy.
Discovering new cytokines and growth factors helps us understand the HSC niche better. This knowledge is helping us create targeted treatments. These treatments aim to improve HSC function and support blood cell production.
Artificial Niche Engineering
Artificial niche engineering is another exciting field. It’s about making fake environments that mimic the real HSC niche. This could lead to better results in HSC transplants.
Researchers are working on creating artificial niches. They use biomaterials and microfabrication to make structures that look like the real niche. This helps HSCs grow and function better.
Exosomes and Microvesicles
Exosomes and microvesicles are being studied for their role in HSC regulation. These tiny particles can send signals between cells, affecting HSC behavior and blood cell production. Scientists are trying to figure out how to use them to stimulate HSCs.
Using exosomes and microvesicles could be a new way to help HSCs. It offers a chance to send signals directly to HSCs and their environment.
Challenges and Limitations in Hematopoietic Stem Cell Stimulation
Exploring hematopoietic stem cell stimulation brings up challenges and limits. This complex therapy is promising but comes with risks and complications.
Potential for Malignant Transformation
One big worry is malignant transformation. Stimulating these cells can sometimes cause uncontrolled growth. This could lead to leukemia or other blood cancers. Experts say this risk is a key thing to think about when using these cells for treatment.
Exhaustion of the Stem Cell Pool
Another issue is the risk of using up the stem cell pool. Keeping these cells stimulated can deplete them. This makes it hard for the bone marrow to make blood cells over time. It can lead to aplastic anemia or other blood problems, affecting patient health.
Immune Complications and Graft-versus-Host Disease
Immune problems, like graft-versus-host disease (GVHD), are also big concerns. GVHD happens when the immune cells from the stem cells see the host body as foreign. This leads to an immune attack on the host’s tissues. This is a big issue in allogeneic hematopoietic stem cell transplants.
Dealing with these challenges needs a detailed plan. This includes choosing patients carefully, watching for early signs of problems, and finding new ways to reduce risks. By tackling these issues, we can make hematopoietic stem cell stimulation safer and more effective.
Conclusion: Future Directions in Hematopoietic Stem Cell Research and Therapy
Hematopoietic stem cell (HSC) research is growing fast. We’re learning more about HSCs and finding new ways to help them work better. This could lead to new treatments for blood diseases.
New studies are looking into things like special growth factors and creating artificial environments for HSCs. They’re also exploring the use of tiny particles called exosomes. These ideas could make bone marrow transplants safer and more effective.
But, there are challenges ahead. We have to be careful not to harm the stem cells. Despite these risks, researchers keep pushing forward. They want to make healthcare better for everyone.
FAQ
What are the challenges associated with hematopoietic stem cell stimulation?
There are risks like turning into cancer cells, running out of stem cells, and immune problems. These need careful thought when treating with HSCs.
What are the clinical applications of hematopoietic stem cell stimulation?
Stimulation of HSCs is used in bone marrow transplants and treating blood diseases. It also helps after chemotherapy and radiation. It’s very important for treatment.
What are the therapeutic approaches to stimulate hematopoietic stem cells?
To help HSCs, doctors use growth factors, small molecules, and gene therapy. These methods aim to improve blood cell making and treat blood issues.
How do inflammatory signals affect hematopoietic stem cells?
Inflammation can change how HSCs work. It affects blood cell production and can lead to blood disorders.
What is the role of the microenvironment in hematopoietic stem cell regulation?
The microenvironment, with its cell-to-cell interactions and oxygen levels, supports HSCs. It helps them stay healthy and function well.
How do cytokines regulate hematopoietic stem cell activity?
Cytokines, like interleukins and Colony-Stimulating Factors (CSFs), help HSCs talk to their surroundings. This controls how HSCs behave.
What growth factors stimulate hematopoietic stem cells?
Growth factors like Stem Cell Factor (SCF), Thrombopoietin (TPO), and Flt3 ligand help HSCs. They are important for HSCs to work right.
What is hematopoiesis?
Hematopoiesis is how HSCs turn into different blood cells. It happens in specific places in our body all our lives
Where do hematopoietic stem cells reside?
HSCs live mainly in the bone marrow. But, they can also be found in other places where blood is made.
What are hematopoietic stem cells?
Hematopoietic stem cells (HSCs) are special cells. They create all types of blood cells. This is key to keeping our blood healthy.