Last Updated on October 21, 2025 by mcelik

Sickle cell disease is a group of inherited disorders that affect hemoglobin production. Sickle cell anemia is the most common form, impacting millions worldwide and causing significant health challenges.
We understand the serious effects of sickle cell anemia on individuals and families. It’s important to know the facts for proper care and awareness. Many people often ask, “which of the following is true about sickle cell anemia? The answer is that it occurs when a person inherits two abnormal hemoglobin genes, one from each parent. This genetic change leads to the production of abnormal hemoglobin, which causes red blood cells to take on a sickle shape.
Knowing the truth about sickle cell anemia helps patients and families manage the condition with more confidence and ensures they get the right medical care.
Key Takeaways
- Sickle cell disease is a group of inherited disorders affecting hemoglobin production.
- Sickle cell anemia is the most common and severe form of sickle cell disease.
- Understanding the facts about sickle cell anemia is crucial for providing comprehensive care.
- Sickle cell anemia results from inheriting two abnormal hemoglobin genes.
- It’s a condition that requires ongoing medical attention and support.
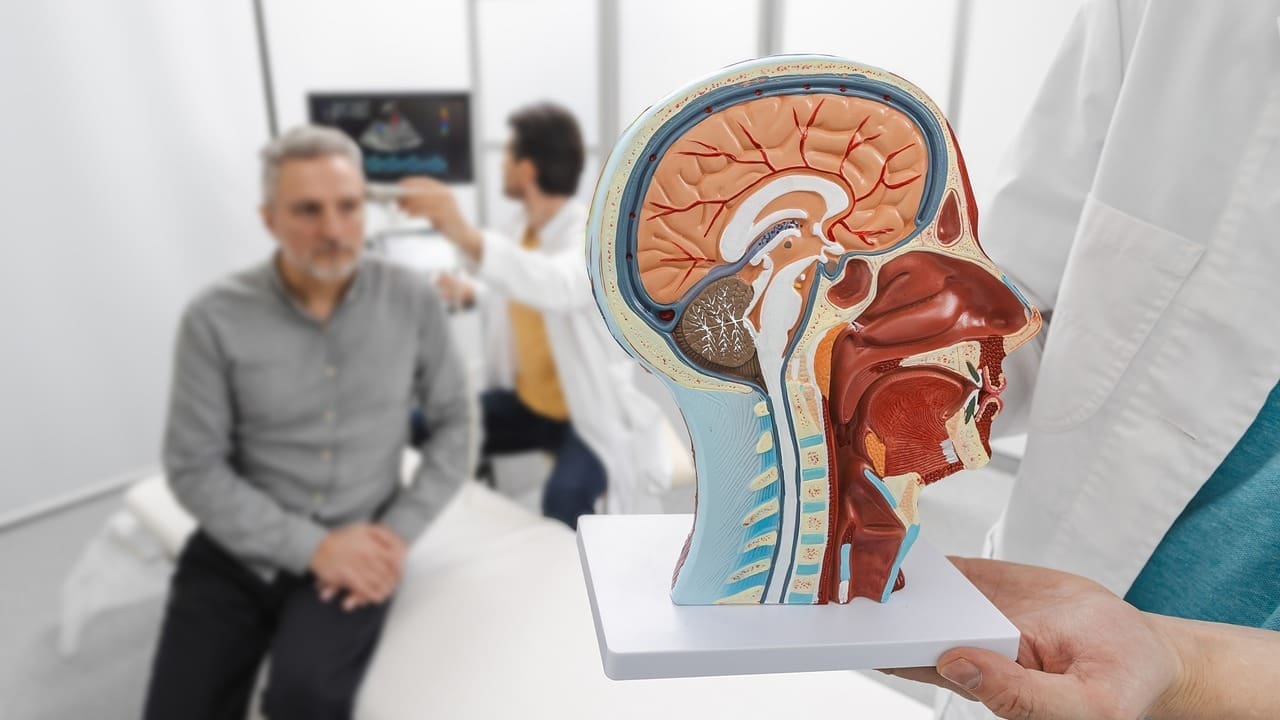
Understanding Sickle Cell Disease: A Hematological Perspective
Sickle cell disease is a complex condition that affects red blood cells. It happens when the body makes abnormal hemoglobin. This leads to red blood cells becoming misshapen, or “sickled.”
This condition can greatly impact a person’s quality of life. It’s a serious health issue that needs attention.
Definition and Classification of Sickle Cell Disorders
Sickle cell disease is a group of genetic disorders. They affect how the body makes hemoglobin. A mutation in the HBB gene causes this problem.
The disease is marked by hemoglobin S (HbS). This abnormal hemoglobin can cause red blood cells to sickle under certain conditions.
There are different types of sickle cell disorders. The most common is Homozygous Sickle Cell Disease (HbSS). This happens when someone has two copies of the mutated HBB gene.
Other types include Hemoglobin SC Disease (HbSC) and Sickle Beta-Thalassemia. These result from different gene combinations.
Global Epidemiology and Distribution
Sickle cell disease is a global health concern. It’s most common in sub-Saharan Africa. The HbS allele is very common there.
It’s also found in the Mediterranean, the Middle East, and parts of India. Historical migration and malaria have played a role in its spread.
The disease is more common in areas with high malaria rates. The HbS allele helps protect against malaria.
Knowing where sickle cell disease is common is key. It helps us develop better public health plans. We must look at genetics, environment, and social factors.
The Molecular Basis of Sickle Cell Disease

To understand sickle cell disease, we must look at hemoglobin’s structure and function. Hemoglobin is a key protein in red blood cells. It carries oxygen from the lungs to our body’s tissues. Its role is essential for keeping red blood cells healthy.
Hemoglobin Structure and Function
Hemoglobin is made of four chains: two alpha and two beta. Each chain has a heme group with iron, which binds oxygen. This structure lets hemoglobin change shape when it binds oxygen. This change helps release oxygen to our tissues.
The HbS Mutation: Valine Substitution for Glutamic Acid
The HbS mutation changes a single nucleotide in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. The change swaps valine for glutamic acid at the sixth position of the beta-globin chain. This swap changes hemoglobin’s properties significantly.
Molecular Consequences of the HbS Mutation
The HbS mutation creates abnormal hemoglobin, known as sickle hemoglobin (HbS). When HbS is not oxygenated, it forms long, rigid fibers. These fibers distort red blood cells into a sickle shape. This is the main reason for sickle cell disease’s symptoms.
| Molecular Change | Effect on Hemoglobin | Clinical Consequence |
| Valine substitution for glutamic acid | Polymerization of HbS under deoxygenated conditions | Sickling of red blood cells |
| Abnormal hemoglobin structure | Reduced solubility and increased viscosity | Vaso-occlusion and ischemia |
| Red blood cell distortion | Increased hemolysis and reduced red blood cell lifespan | Anemia and related complications |
Genetics and Inheritance Patterns of Sickle Cell Disease
A detailed illustration of the genetic inheritance patterns of sickle cell disease. Set in a clinical laboratory environment, the image depicts a human chromosome diagram in the foreground, showcasing the characteristic sickle-shaped red blood cells. In the middle ground, a microscopic view of sickle cell erythrocytes is prominently displayed, while the background features medical equipment and a sterile, well-lit setting to convey the scientific and clinical nature of the subject matter. The lighting is soft and even, highlighting the key visual elements and creating a sense of depth and realism. The camera angle is slightly elevated to provide a comprehensive overview of the genetic and hematological aspects of sickle cell disease.
It’s important to know the genetics of sickle cell disease to understand how it’s passed down. This disease is caused by a change in the HBB gene. This gene is responsible for a part of hemoglobin.
Autosomal Recessive Inheritance
Sickle cell disease follows an autosomal recessive pattern. This means a person needs two bad genes to have the disease. We’ll look into what this means for families.
People who carry the disease but don’t show symptoms can still pass the bad gene to their kids. This is why genetic counseling is key for families with sickle cell disease.
Heterozygous vs. Homozygous States
Being heterozygous means having one normal and one sickle cell gene. People in this state are usually healthy but can pass the sickle cell gene to their kids. Being homozygous means having two sickle cell genes, leading to full sickle cell disease symptoms.
| Genotype | Phenotype | Health Implications |
| Heterozygous (HbAS) | Carrier | Generally healthy, may have some protection against malaria |
| Homozygous (HbSS) | Sickle Cell Disease | Experiences symptoms of sickle cell disease |
Pathophysiology of Sickle Cell Disease
Sickle cell disease’s complex pathophysiology includes hemoglobin polymerization, red blood cell sickling, and vaso-occlusion. These steps are linked, causing the disease’s symptoms.
Hemoglobin Polymerization and Red Blood Cell Sickling
Hemoglobin polymerization is key in sickle cell disease. When oxygen levels drop, abnormal hemoglobin (HbS) forms rigid, sickle-shaped red blood cells. This change is initially reversible but becomes permanent with repeated episodes.
Key factors influencing hemoglobin polymerization include:
- Low oxygen tension
- High intracellular hemoglobin concentration
- Presence of other abnormal hemoglobins
A leading researcher noted,
“The polymerization of HbS is a crucial event in the pathogenesis of sickle cell disease, leading to the characteristic sickling of red blood cells.”
Vaso-occlusion Mechanisms
Vaso-occlusion is a major feature of sickle cell disease. It occurs when sickled red blood cells block small blood vessels. This causes tissue ischemia and pain crises, common symptoms of the disease.
The causes of vaso-occlusion are complex, involving:
- Adhesion of sickled red blood cells to endothelial cells
- Activation of various cellular and molecular pathways
- Increased blood viscosity due to the presence of sickled cells
Hemolysis and Anemia Development
Hemolysis, or the destruction of red blood cells, is a major part of sickle cell disease’s pathophysiology. Sickled red blood cells are more likely to be destroyed, leading to anemia.
Anemia in sickle cell disease is made worse by:
- Chronic hemolysis
- Splenic sequestration
- Aplastic crises
Understanding these processes is key to managing the disease and improving patient outcomes.
Which of the Following is True About Sickle Cell Anemia: Key Facts

It’s important to know the basics about sickle cell anemia. This condition affects how red blood cells carry oxygen. It’s a genetic disorder that impacts hemoglobin production.
Genetic Basis and Inheritance
Sickle cell anemia comes from a gene mutation in the HBB gene. This mutation creates abnormal hemoglobin, known as sickle hemoglobin or HbS. People need two copies of this mutated gene to have the disease.
Carriers have one normal and one mutated gene. They don’t show all symptoms but can pass the gene to their kids.
Hematological Manifestations
The main issue in sickle cell anemia is red blood cells sickling. This makes them break down faster, leading to anemia.
People with sickle cell anemia often have pain crises. These happen when sickled cells block blood vessels.
Clinical Complications
Sickle cell anemia can lead to many problems. These include infections, stroke, and more. Getting regular medical care helps manage these issues.
“Sickle cell disease is associated with a high risk of infections, particularly those caused by encapsulated organisms such as Streptococcus pneumoniae.”
Protective Effect Against Malaria
Having sickle cell trait (HbAS) can protect against malaria. This is especially true for severe malaria caused by Plasmodium falciparum. This is why sickle cell trait is common in malaria areas.
Knowing these facts is key to caring for people with sickle cell anemia.
Clinical Manifestations of Sickle Cell Disease
Sickle cell disease has many symptoms, both sudden and long-term. These symptoms come from the disease’s effects on blood cells and blood flow.
Acute Complications
Acute complications of sickle cell disease happen quickly and can be dangerous. Some common ones include:
- Pain Crises: Severe pain happens when blood vessels get blocked by sickled red blood cells.
- Acute Chest Syndrome: This is a serious condition with a new lung problem, fever, and breathing issues.
- Splenic Sequestration: Blood suddenly pools in the spleen, causing severe anemia and serious problems.
- Aplastic Crisis: Caused by parvovirus B19, it stops the body from making new red blood cells, leading to severe anemia.
Chronic Complications
Chronic complications of sickle cell disease happen over time. They come from repeated damage to organs. Some include:
- Chronic Anemia: Long-term anemia from broken-down red blood cells, causing tiredness and weakness.
- Organ Damage: Damage to organs like the kidneys, liver, and heart from repeated blockages.
- Osteonecrosis: Bones in the hips and shoulders can die due to lack of blood flow.
- Retinopathy: Eye damage can lead to vision loss and blindness if not treated.
Knowing about these symptoms is key to managing sickle cell disease. Early treatment can greatly improve a patient’s life.
Hematological Findings in Sickle Cell Disease
Hematological findings are key in diagnosing and managing sickle cell disease. They give insights into the disease’s pathophysiology. This helps clinicians assess its severity and potential complications.
Complete Blood Count Abnormalities
A complete blood count (CBC) is a fundamental diagnostic tool in hematology. In patients with sickle cell disease, CBC typically reveals anemia. This is characterized by low hemoglobin levels and hematocrit. The red blood cell count is often decreased, while the white blood cell count may be elevated due to inflammation or infection.
The CBC also helps in identifying other abnormalities such as thrombocytopenia or thrombocytosis. These can occur due to various factors including splenic sequestration or bone marrow response to anemia.
Peripheral Blood Smear Characteristics
Examination of the peripheral blood smear is crucial for diagnosing sickle cell disease. Characteristic findings include sickle-shaped red blood cells, which are a hallmark of the disease. Other features may include target cells, Howell-Jolly bodies, and nucleated red blood cells. These are indicative of hyposplenism or functional asplenia.
Reticulocyte Count and Implications
The reticulocyte count is a measure of the bone marrow’s response to anemia. In sickle cell disease, an elevated reticulocyte count indicates the marrow’s attempt to compensate for the hemolysis. A high reticulocyte count is often seen in patients with sickle cell disease. It reflects the ongoing hemolytic process.
Hemoglobin Electrophoresis Patterns
Hemoglobin electrophoresis is a critical diagnostic test for identifying the different types of hemoglobinopathies, including sickle cell disease. In sickle cell anemia (HbSS), the predominant hemoglobin is HbS, with variable amounts of HbF (fetal hemoglobin). The pattern of hemoglobin on electrophoresis helps in diagnosing the specific hemoglobinopathy and assessing its severity.
The key hematological findings in sickle cell disease can be summarized as follows:
- Anemia and low hemoglobin levels
- Presence of sickle-shaped red blood cells on peripheral smear
- Elevated reticulocyte count
- Characteristic hemoglobin electrophoresis pattern showing predominantly HbS
Understanding these hematological findings is essential for the diagnosis, management, and follow-up of patients with sickle cell disease.
Diagnostic Approaches for Sickle Cell Disease
Early detection of sickle cell disease is key. Several methods are used to find it early. These include lab tests and screening programs.
Newborn Screening Programs
Newborn screening is crucial for early detection. A simple blood test is done when the baby is 24 to 48 hours old. This test checks for abnormal hemoglobin, helping start early treatment.
Universal newborn screening is used in many places. It helps find sickle cell disease early. This way, families can get the help they need sooner.
Hemoglobin Electrophoresis
Hemoglobin electrophoresis is a key test for diagnosing sickle cell disease. It separates hemoglobin types by charge. This helps find abnormal hemoglobin.
Hemoglobin electrophoresis is a top choice for diagnosing sickle cell disease. It tells the difference between sickle cell trait and disease. This is vital for treatment.
High-Performance Liquid Chromatography
High-performance liquid chromatography (HPLC) is used to detect hemoglobin types. It’s very accurate and can find HbS, HbA, and HbF levels.
HPLC is great for sickle cell disease diagnosis and monitoring. It gives detailed hemoglobin info. This is key for managing the disease and preventing complications.
Genetic Testing Methods
Genetic testing looks at DNA for sickle cell disease mutations. It confirms the diagnosis and gives genotype info. This is useful for family planning and counseling.
Genetic testing can also find sickle cell gene carriers. This helps with reproductive choices. We suggest genetic counseling for families with sickle cell history.
Management of Sickle Cell Disease: Current Standards of Care
Managing sickle cell disease today focuses on prevention, pain control, and smart use of blood transfusions. Each patient needs a care plan that fits their unique situation.
Preventive Measures
Prevention is key in sickle cell disease care. It includes:
- Immunizations: Keeping up with vaccines like pneumococcal and meningococcal to fight off infections.
- Infection Prevention: Giving antibiotics to kids to lower the chance of serious infections.
- Hydration: Drinking enough water to avoid dehydration, which can cause crises.
- Avoiding Triggers: Steer clear of things that can trigger crises, like very hot or cold temperatures and high places.
Pain Management Strategies
Pain control is a big part of sickle cell disease care. It involves:
- Assessment and Monitoring: Checking pain regularly with special scales to decide on treatment.
- Pharmacological Interventions: Using pain medicines, from non-opioids to opioids, based on how bad the pain is.
- Non-Pharmacological Interventions: Adding things like therapy, relaxation, and physical therapy to help with pain.
Blood Transfusion Therapy
Blood transfusions help prevent some problems and manage severe anemia. They include:
- Simple Transfusions: Boosting normal red blood cells to lower sickle-prone cells.
- Exchange Transfusions: Swapping out sickle-prone cells for normal ones, especially in severe cases.
By using these methods, doctors can give patients with sickle cell disease better care. This improves their life quality and lowers the risk of serious issues.
Pharmacological Interventions for Sickle Cell Disease
New treatments have changed how we manage sickle cell disease. These treatments aim to lessen pain crises, cut down on blood transfusions, and boost patients’ quality of life.
Hydroxyurea: Mechanism and Benefits
Hydroxyurea is a key treatment for sickle cell disease. It boosts fetal hemoglobin, which lowers pain crises and may reduce blood transfusions. Clinical trials have shown it can cut down on acute chest syndrome and other sickle cell disease complications.
L-glutamine (Endari)
L-glutamine, known as Endari, is another approved treatment. It reduces pain crises by fighting oxidative stress. Clinical evidence shows it can lower hospital stays for sickle cell crises.
Crizanlizumab and Voxelotor
Crizanlizumab and voxelotor are newer treatments with promise. Crizanlizumab targets P-selectin to lessen vaso-occlusive crises. Voxelotor increases oxygen affinity of hemoglobin, reducing hemolysis. Both have shown to improve patient results.
Emerging Drug Therapies
The sickle cell disease treatment pipeline is strong, with many new drugs in the works. These include gene therapies, anti-adhesion molecules, and more. Ongoing research aims to offer more treatment options to patients.
| Drug | Mechanism of Action | Benefits |
| Hydroxyurea | Increases fetal hemoglobin production | Reduces pain crises, need for blood transfusions |
| L-glutamine (Endari) | Mitigates oxidative stress | Decreases frequency of pain crises |
| Crizanlizumab | Targets P-selectin | Reduces vaso-occlusive crises |
| Voxelotor | Increases hemoglobin’s affinity for oxygen | Reduces hemolysis |
In conclusion, new treatments have greatly improved sickle cell disease management. With options from hydroxyurea to emerging therapies, doctors can create personalized treatment plans. This significantly improves patient outcomes.
Special Considerations Across the Lifespan
People with sickle cell disease face different healthcare needs at each stage of life. It’s important to understand these needs to give the best care. This ensures they get the support they need.
Pediatric Sickle Cell Management
Managing sickle cell disease in kids starts with early diagnosis and intervention. Newborn screening helps find affected babies early. This allows for quick start of treatments and prevention.
Pediatric care aims to prevent problems, manage pain, and help kids grow normally. Regular visits to a pediatric hematologist are key. They help track the disease and adjust treatments as needed. Teaching families about recognizing complications and sticking to treatment plans is also crucial.
Adult Transition of Care
When kids with sickle cell disease grow up, their care changes. Coordinated care between pediatric and adult healthcare providers is needed. This ensures treatment continues smoothly.
Adults with sickle cell disease need ongoing care. This includes managing pain, watching for complications, and getting mental health support. It’s also important to address the psychosocial aspects of the disease, like work, insurance, and personal life.
Pregnancy and Reproductive Health
Pregnancy is high-risk for women with sickle cell disease. They need specialized prenatal care. This involves watching for problems in both mom and baby.
Preconception counseling is key to discuss risks. Reproductive health also includes planning for pregnancy and managing pregnancy-related issues. A team of healthcare professionals is needed for the best outcomes.
Aging with Sickle Cell Disease
As people with sickle cell disease get older, they face more health problems. Comprehensive geriatric care is vital to manage these issues. It helps improve their quality of life.
Older adults need careful monitoring for organ damage and other health issues. Palliative care can help manage pain and other symptoms. This is part of their care plan.
Curative Approaches: Stem Cell Transplantation and Gene Therapy
Medical science has made big strides in treating sickle cell disease. Now, stem cell transplantation and gene therapy are seen as possible cures. These new treatments aim to fix the disease’s root cause, giving hope to those suffering.
Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation (HSCT) is the only cure for sickle cell disease today. It replaces the patient’s bone marrow with healthy stem cells from a donor, often a sibling or someone else.
The HSCT process is detailed and includes several steps:
- Pre-transplant conditioning to weaken the immune system
- Infusion of donor stem cells
- Post-transplant care to manage side effects and prevent disease
Though HSCT can cure, it comes with risks. Issues like graft failure, disease from the donor, and infections can happen. Yet, better transplant methods and care have made it a safer option for some patients.
| Aspect | Description |
| Donor Selection | Typically a sibling or unrelated donor with HLA compatibility |
| Pre-transplant Conditioning | Chemotherapy and/or radiation to suppress the immune system |
| Complications | Graft failure, graft-versus-host disease, infections |
Gene Therapy Approaches
Gene therapy is a new hope for sickle cell disease. It changes or fixes the faulty gene causing the disease. Viral vectors carry a healthy gene to the patient’s stem cells.
“Gene therapy has the potential to cure sickle cell disease by correcting the underlying genetic defect, offering a treatment that could be more accessible than HSCT for many patients.”
Several gene therapy methods are being tested, including:
- Lentiviral vector-mediated gene transfer
- CRISPR-Cas9 gene editing
These methods aim to fix hemoglobin production, easing sickle cell disease symptoms. Though still in trial stages, early results are promising.
As research grows, HSCT and gene therapy will likely become key in treating sickle cell disease. They offer new hope for patients around the world.
Conclusion: Advances and Future Directions in Sickle Cell Disease Management
Looking back, we see big steps forward in managing sickle cell disease. These steps have made a real difference in how patients live. We’re excited about what’s coming next.
New medicines like hydroxyurea and voxelotor are giving doctors more ways to help. We’re also looking into ways to cure the disease, like gene therapy.
The future looks bright for sickle cell disease care. We expect to see even better treatments and more support for patients. This will help people with the disease live fuller lives.
Our team is dedicated to finding new ways to help patients. We’re committed to providing top-notch care and support to people from around the world.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder that affects how red blood cells are made. It makes them misshapen and prone to breaking down. The most common type is sickle cell anemia.
What causes sickle cell anemia?
Sickle cell anemia comes from a gene mutation in the HBB gene. This mutation leads to abnormal hemoglobin, known as HbS.
How is sickle cell disease inherited?
Sickle cell disease is inherited in an autosomal recessive pattern. This means a person needs two defective HBB genes, one from each parent, to have the disease.
What are the symptoms of sickle cell disease?
Symptoms include anemia, pain episodes, infections, and damage to organs like the spleen, kidneys, and liver.
How is sickle cell disease diagnosed?
Diagnosis often starts with newborn screening. It can also involve hemoglobin electrophoresis, high-performance liquid chromatography, or genetic testing.
What are the treatment options for sickle cell disease?
Treatments include managing pain, blood transfusions, and medications like hydroxyurea. Other options are L-glutamine, crizanlizumab, voxelotor, and hematopoietic stem cell transplantation.
Can sickle cell disease be cured?
The only cure now is hematopoietic stem cell transplantation. Gene therapy is also being researched as a potential cure.
How does sickle cell trait differ from sickle cell disease?
Sickle cell trait means having one normal and one defective HBB gene. It usually causes mild or no symptoms. Sickle cell disease, on the other hand, is when a person has two defective genes.
What is the protective effect of sickle cell trait against malaria?
People with sickle cell trait are less likely to get malaria, especially severe forms. This is because their red blood cells are less hospitable to malaria parasites.
What are the complications of sickle cell disease?
Complications include acute chest syndrome, stroke, splenic sequestration, and damage to organs.
How is pain managed in sickle cell disease?
Pain management uses non-pharmacological methods and medications. This includes opioids, NSAIDs, and other pain relievers.
What is the role of hydroxyurea in treating sickle cell disease?
Hydroxyurea helps by reducing painful crises and possibly lowering the need for blood transfusions. It does this by increasing fetal hemoglobin production.
References
- Piel, F. B., Steinberg, M. H., & Rees, D. C. (2017). Sickle cell disease. New England Journal of Medicine, 376(16), 1561“1573. https://www.nejm.org/doi/full/10.1056/NEJMra1510865
- Rees, D. C., Williams, T. N., & Gladwin, M. T. (2010). Sickle-cell disease. The Lancet, 376(9757), 2018“2031. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2852629/