Last Updated on December 3, 2025 by Bilal Hasdemir
Colorectal cancer hits thousands in the U.S. each year. Surgery is often a necessary treatment. One such surgery is bowel resection, also known as colon resection or intestinal resection.Identifying the main medical reasons why bowel resection needed, such as cancer, strictures, or severe inflammation.
This surgery removes a part of the intestine. It’s done to treat various medical conditions, like colorectal cancer and inflammatory bowel disease. A healthcare professional will decide if you need this surgery after a thorough check-up and diagnosis.
Key Takeaways
- Bowel resection surgery is often necessary for treating colorectal cancer and other intestinal conditions.
- The procedure involves removing a portion of the intestine.
- A thorough evaluation and diagnosis by a healthcare professional are required before undergoing bowel resection.
- Various medical conditions can be treated with bowel resection surgery.
- Bowel resection is also known as colon resection or intestinal resection.
The Basics of Bowel Resection Surgery
It’s important for patients to know about bowel resection surgery. This surgery removes a part of the intestine that’s sick or damaged. It can be either the small intestine or the colon.
Definition and Purpose of the Procedure
Bowel resection, or intestinal resection, aims to take out the sick part of the bowel. The main goal is to get rid of the diseased segment. This helps to ease symptoms and improve the patient’s life quality.
Anatomical Considerations: Small Intestine vs. Colon
The way bowel resection surgery is done changes based on the part of the intestine involved. The small intestine is key for absorbing nutrients. On the other hand, the colon is important for absorbing water and handling waste.
| Aspect | Small Intestine | Colon |
| Primary Function | Nutrient Absorption | Water Absorption and Waste Processing |
| Surgical Considerations | Preservation of absorptive capacity | Management of fecal stream |
Common Terminology in Bowel Surgery
Knowing common terms is key to understanding bowel resection surgery. Words like resection, anastomosis, and ostomy are often used in bowel surgery.
- Resection: Removal of the diseased segment
- Anastomosis: Reconnection of the remaining bowel segments
- Ostomy: Creation of an opening in the abdomen for waste diversion
Why Bowel Resection Is Needed: Primary Indications

Doctors decide on bowel resection when other treatments don’t work or aren’t right. This surgery helps with serious gut problems that really hurt a person’s life quality.
Medical vs. Surgical Management Decision-Making
Choosing between medicine and surgery depends on many things. Doctors look at how bad the symptoms are, what’s causing them, and the patient’s health. For things like colon cancer, IBD, and diverticulitis, surgery is needed when medicine fails or the problem is urgent.
Key factors influencing this decision include:
- The severity and extent of the disease
- The presence of complications such as obstruction or perforation
- The patient’s response to medical therapy
- The presence of high-risk features or precancerous conditions
Emergency vs. Planned Procedures
Bowel resection can be urgent or planned. Urgent surgeries are for sudden problems like blockages or tears. Planned surgeries are for conditions that aren’t as urgent but need surgery.
| Condition | Type of Procedure | Typical Indications |
| Colorectal Cancer | Planned | Tumor removal, potentially curative |
| Inflammatory Bowel Disease (IBD) | Planned or Emergency | Severe disease, complications like obstruction |
| Diverticulitis | Emergency or Planned | Acute diverticulitis, recurrent episodes |
| Intestinal Obstruction | Emergency | Immediate relief of obstruction |
Diagnostic Process Leading to Surgery
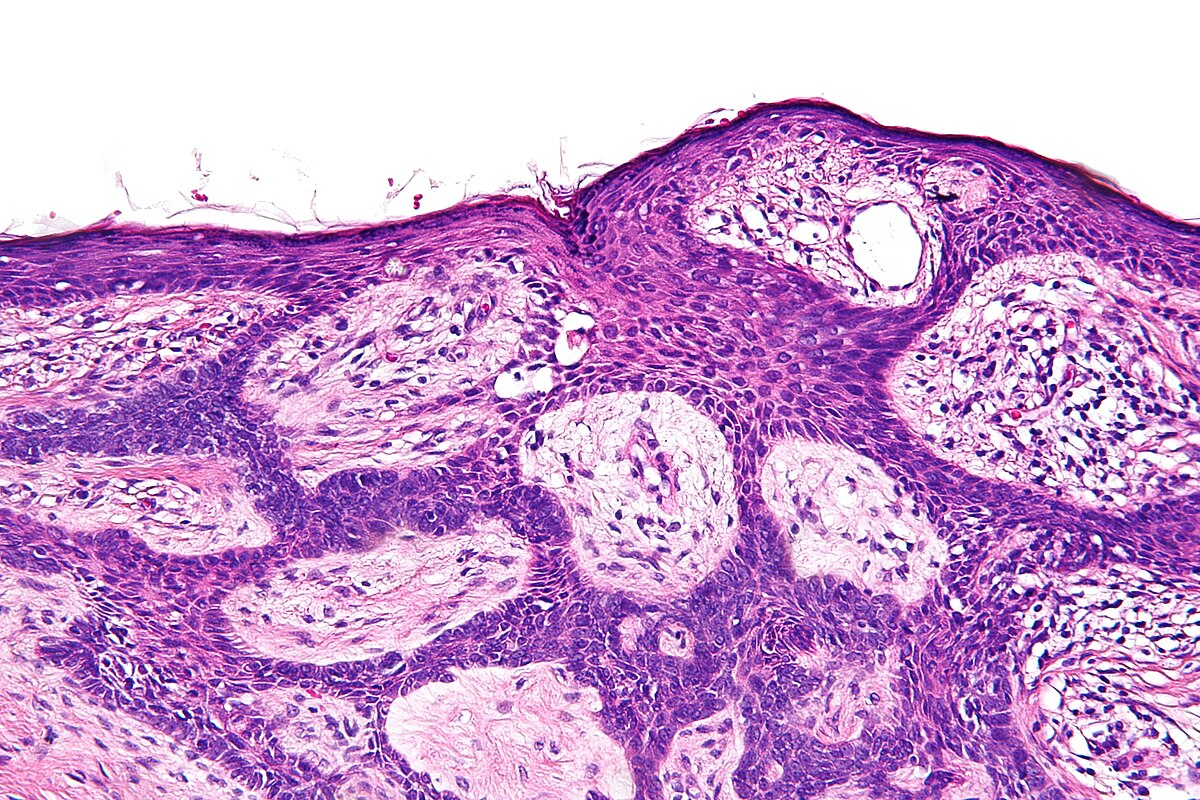
Tests and checks help find out why a patient is sick and how bad it is. This might include CT scans, endoscopy, and biopsies to see the bowel’s condition.
Accurate diagnosis is key for knowing if bowel resection is needed. The findings help the surgical team decide how much to remove and if they need to make an ostomy.
Colorectal Cancer as a Leading Cause
Colorectal cancer is a major reason for bowel surgery. It requires a deep understanding of how to treat it. The surgery depends on the cancer’s stage, location, and the patient’s health.
Colon Cancer Staging and Surgical Approaches
Staging colon cancer is key to choosing the right surgery. The stage, from early (Stage I) to advanced (Stage IV), decides between a segmental resection or a bigger colectomy. Early cancer might need a simpler surgery, while advanced cancer might require a more complex one.
Rectal Cancer Treatment Considerations
Rectal cancer treatment is different because of its location. It often involves neoadjuvant therapy (chemo and radiation) followed by surgery. The surgery, like total mesorectal excision (TME), is very important for good results.
“The integration of neoadjuvant therapy with precise surgical techniques has significantly improved outcomes in rectal cancer patients.”
Preventive Resection for High-Risk Patients
People at high risk of colorectal cancer, like those with a family history or genetic syndromes, might get preventive surgery. This can greatly lower their risk of getting cancer.
- Genetic screening to find high-risk patients
- Talking about the risks and benefits of preventive surgery
- Deciding based on genetics, family history, and health
Inflammatory Bowel Disease (IBD) Management
Managing IBD means controlling symptoms and preventing complications. It includes Crohn’s disease and ulcerative colitis. These are chronic conditions that can cause a lot of problems if not managed well.
Crohn’s Disease: When Surgery Becomes Necessary
Crohn’s disease can affect any part of the GI tract. Medical therapy is the main treatment. But, surgery is needed for complications like narrowing or fistulas.
Surgery helps relieve symptoms and improves life quality. It’s considered when medical treatment fails or complications arise. Options include bowel resection or draining abscesses.
Ulcerative Colitis and Total Colectomy
Ulcerative colitis affects only the colon. If medical therapy fails or complications like dysplasia or cancer occur, removing the colon is an option. This can cure the disease but might require an ileal pouch or ileostomy.
The surgery choice depends on disease extent, complications, and health. Removing the colon can greatly improve life quality for those with severe ulcerative colitis.
Surgical Options for Refractory IBD
For IBD that doesn’t respond to medicine, several surgeries are available. These include removing the diseased part of the intestine. The right surgery depends on the disease and patient’s health.
Surgical management of IBD needs a team effort. This includes pre-op evaluation, surgery, and post-op care. A team of gastroenterologists, surgeons, and other experts is key for the best results.
In conclusion, treating IBD often requires both medicine and surgery. Knowing when surgery is needed for Crohn’s and ulcerative colitis is vital for effective care.
Diverticular Disease and Diverticulitis
When diverticula in the colon wall become inflamed, it results in diverticulitis. This is a complication of diverticular disease. Diverticular disease is when pouches form in the colon wall. It’s common in adults over 40 in the United States.
Diverticulitis can be mild or severe. Symptoms include abdominal pain, changes in bowel habits, and fever. Treatment depends on how severe it is and the patient’s health.
Acute Diverticulitis Requiring Immediate Surgery
In severe cases, immediate surgery is needed. This is for complications like abscesses, perforation, or significant bleeding. Emergency surgery is for risks of peritonitis, a serious infection.
The choice to operate is based on symptoms, complications, and how well treatments work.
Recurrent Diverticulitis Management
For those with recurring diverticulitis, management aims to prevent future attacks. This includes dietary changes and possibly surgery after inflammation goes down.
Elective surgery is for those with recurring diverticulitis. It removes the affected colon part to prevent future episodes.
Elective Surgery After Multiple Episodes
Deciding on elective surgery depends on several factors. These include episode frequency and severity, overall health, and patient preferences. Colon resection is a common surgery for diverticulitis, removing the diseased colon part.
Understanding the condition and treatment options helps patients and healthcare providers make informed decisions.
Intestinal Obstruction and Blockages
Intestinal obstruction happens when the intestine gets blocked. This blockage stops the normal flow of food and waste. If not treated quickly, it can cause serious problems like tissue damage and death.
Mechanical vs. Functional Obstructions
Intestinal obstructions are divided into two types: mechanical and functional. Mechanical obstructions are caused by physical barriers like adhesions, hernias, or tumors. Functional obstructions, or ileus, happen when the muscles that move food and air don’t work right.
Adhesions as a Common Cause
Adhesions are a main reason for mechanical obstructions. They are fibrous bands that can form between intestine loops or between the intestine and other organs. Adhesions often come from past surgeries, but can also be caused by inflammation or injury.
Surgical Approaches for Different Types of Blockages
The surgery needed to fix an intestinal obstruction depends on the cause. For adhesions, the surgery might be to cut the adhesions. If a tumor or hernia is causing the blockage, the surgery could involve removing the tumor or fixing the hernia.
Surgery is key when there’s a risk of bowel damage or perforation. Quick treatment can stop serious problems and help the patient get better.
Bowel Perforation and Trauma
Intestinal perforation is a serious medical emergency. It happens when a hole forms in the intestinal wall. This allows contents to leak into the abdominal cavity, causing a severe infection called peritonitis. This infection needs immediate treatment.
Causes of Intestinal Perforation
Intestinal perforation can come from diseases or injuries. Knowing the causes helps doctors diagnose and treat it well.
- Diseases: Conditions like diverticulitis, inflammatory bowel disease (IBD), and colorectal cancer can weaken the intestinal wall, leading to perforation.
- Trauma: Physical trauma to the abdomen can cause intestinal perforation, either through blunt force or penetrating injuries.
Traumatic Bowel Injuries
Traumatic bowel injuries are a big worry in abdominal trauma. They are hard to diagnose but need a quick and careful look based on how the injury happened and how the patient feels.
| Type of Trauma | Common Causes | Clinical Features |
| Blunt Trauma | Motor vehicle accidents, falls | Abdominal pain, tenderness, guarding |
| Penetrating Trauma | Stab wounds, gunshot wounds | Visible wounds, abdominal pain, peritonitis |
Emergency Surgical Management Protocols
Emergency surgery is often needed for bowel perforation and traumatic bowel injuries. The aim is to stop the leak, fix or remove the damaged part, and avoid more problems.
Surgical Principles:
- Prompt diagnosis and decision-making
- Adequate resuscitation and stabilization of the patient
- Exploratory laparotomy to assess and manage the injury
- Repair or resection of the damaged bowel segment
- Thorough peritoneal lavage to reduce contamination
Managing bowel perforation and trauma well needs a team effort. Surgeons, radiologists, and other healthcare workers must work together. Quick action and treatment are key to better outcomes for these patients.
Benign Tumors, Polyps, and Precancerous Conditions
It’s important to understand benign tumors and polyps to choose the right treatment. These growths are not cancerous but can cause big problems. Large or many growths might lead to bowel blockage or bleeding.
Large Polyps Requiring Surgical Removal
Big polyps in the bowel can be a big issue. They might cause stomach pain, changes in bowel habits, or bleeding. Some polyps can turn cancerous over time. So, removing them surgically is often advised to avoid these issues and ease symptoms.
Whether to remove a polyp surgically depends on its size, where it is, and what it looks like under a microscope. There are advanced ways to remove big polyps. But sometimes, a more serious surgery is needed.
Familial Polyposis Syndromes
Familial polyposis syndromes, like Familial Adenomatous Polyposis (FAP), are genetic. They cause many polyps in the colon and rectum. Without treatment, people with FAP almost surely get colorectal cancer by age 40.
For those with FAP, removing the colon or rectum is often suggested to stop cancer. When to do surgery depends on the polyps’ number and type, and the person’s health.
Preventive Surgery for High-Risk Conditions
People at high risk, like those with a family history of colorectal cancer or certain genetic syndromes, might consider preventive surgery. The aim is to remove risky tissue before cancer starts.
Choosing preventive surgery is a big decision. It involves weighing the risks and benefits. Age, health, and personal wishes are key in making this choice.
| Condition | Surgical Options | Benefits |
| Large Polyps | Advanced Polypectomy, Bowel Resection | Prevents Complications, Alleviates Symptoms |
| Familial Polyposis Syndromes | Total Colectomy, Proctocolectomy | Prevents Colorectal Cancer |
| High-Risk Conditions | Preventive Colectomy | Reduces Cancer Risk |
In summary, benign tumors, polyps, and precancerous conditions need careful handling to prevent problems and lower cancer risk. Surgery, when needed, can be very effective in managing these issues.
Intestinal Ischemia and Necrosis
The intestines need blood to work right. If they don’t get enough, ischemia happens. This can be acute or chronic, each with its own symptoms.
Acute Mesenteric Ischemia
Acute mesenteric ischemia is a big emergency. It’s when blood flow to the intestines suddenly stops, usually because of a blockage. Quick intestinal ischemia treatment is key to stop the intestines from dying.
It shows up with very bad stomach pain. This pain is often worse than what the doctor finds. Doctors use CT scans to find the problem early.
Chronic Intestinal Ischemia
Chronic intestinal ischemia happens when arteries slowly narrow. This is often because of atherosclerosis. It causes long-term stomach pain, weight loss, and malnutrition.
Doctors might suggest lifestyle changes, medicines, or surgery to fix it. Surgery is needed to get blood flowing right again.
Surgical Management of Dead Bowel Tissue
When ischemia causes the intestines to die, surgery is needed. Bowel necrosis surgery removes the dead parts. This stops more problems like holes in the intestines and infection.
Mesenteric ischemia surgery might also try to fix the blood flow or remove the dead parts. The choice depends on how bad the problem is and the patient’s health.
Congenital and Developmental Bowel Conditions
Bowel conditions that start at birth or develop in childhood can affect patients a lot. They need a detailed plan for diagnosis and treatment. This plan includes both medical and surgical steps.
Pediatric Indications for Bowel Surgery
In kids, bowel surgery is needed for many reasons. These include intestinal blockages, atresia, or other issues that stop the bowel from working right. Surgery fixes these problems to help the child’s digestive system work well.
Doctors decide on surgery after checking the child with tests and exams. The aim is to fix the bowel’s shape and function. This improves the child’s life a lot.
Hirschsprung’s Disease and Other Congenital Disorders
Hirschsprung’s disease is when the colon and rectum lack nerve cells. This causes a blockage because the bowel can’t relax and move stool. Surgery removes the bad part and connects the good parts.
Other conditions like intestinal malrotation or Meckel’s diverticulum also need surgery. Malrotation can twist the intestine, cutting off blood. Meckel’s diverticulum can cause bleeding or blockages.
Adult Manifestations Requiring Surgical Intervention
Some bowel conditions aren’t found until adulthood. This is because they might not have shown symptoms in childhood or were missed later. Adults might have symptoms like bowel blockage, chronic pain, or need surgery for other reasons.
Adults with these conditions need careful planning for surgery. Doctors consider the patient’s health, the condition’s details, and any past surgeries. The goal is to fix symptoms, solve problems, and better the patient’s life.
Preparation for Bowel Resection Surgery
To ensure a smooth recovery, proper preparation for bowel resection surgery is key. This includes preoperative testing, bowel preparation, and managing medications before surgery.
Preoperative Testing and Evaluation
Before surgery, patients must undergo various tests to check their health. These tests include blood work, CT scans, and MRI. They help assess the bowel and surrounding tissues.
Preoperative testing is vital for spotting risks or complications. It helps the surgical team tailor their approach for each patient, improving outcomes.
Bowel Preparation Protocols
Bowel preparation is essential to clean the bowel and reduce infection risk. It involves dietary changes, laxatives, and sometimes antibiotics. This reduces bacterial load in the bowel.
The bowel preparation protocol varies based on the surgeon and patient’s condition. It’s important for patients to follow these instructions closely to prepare the bowel for surgery.
Medication Management Before Surgery
Managing medications before surgery is critical. Patients must tell their healthcare providers about all medications they take. This includes prescription drugs, over-the-counter medications, and supplements.
Some medications may need to be adjusted or stopped before surgery. For example, anticoagulants may be stopped to prevent bleeding. The healthcare team will guide on managing medications before surgery.
By following these preoperative guidelines, patients can greatly help their surgery’s success and recovery.
Surgical Approaches and Techniques
Surgical methods for bowel resection have changed a lot. Now, patients have options from open surgery to new, less invasive ways. The choice depends on the patient’s health, the surgeon’s skills, and the surgery’s needs.
Open Surgery: Indications and Process
Open surgery is a traditional method for bowel resection. It involves a big cut in the belly to reach the bowel. This method is used for complex cases or when direct access is needed.
- Indications: Open surgery is for patients with severe bowel disease, lots of adhesions, or when other methods can’t be used.
- Process: The surgeon makes a big cut to get to the bowel. They then find and remove the diseased part.
Minimally Invasive Options: Laparoscopic and Robotic
Minimally invasive surgery is now more common for bowel resection. It has smaller cuts, less pain, and faster recovery.
Laparoscopic surgery uses a thin, lighted tube with a camera and special tools. It’s done through small cuts.
- Benefits: It lowers the risk of complications, reduces pain, and shortens hospital stays.
- Limitations: It needs special training. Not all patients can have it due to adhesions or complex disease.
Robotic surgery is a more advanced minimally invasive method. It uses a robotic system to improve the surgeon’s skills. It offers better control, vision, and precision.
- Advantages: It gives better vision, precision, and is easier on the surgeon.
- Indications: It’s good for complex cases and patients needing precise surgery.
Ostomy Creation: Temporary vs. Permanent
Ostomy creation is sometimes needed during bowel resection surgery. An ostomy is a surgically made opening in the belly for waste.
- Temporary Ostomy: It’s made to let the bowel heal after surgery. It’s usually removable.
- Permanent Ostomy: It’s needed when a big part of the bowel is removed or the disease requires a permanent solution.
The choice between a temporary or permanent ostomy depends on the patient’s condition and the surgery’s extent.
Risks and Complications of Bowel Resection
It’s important for patients to know the risks of bowel resection surgery. This surgery, like any major surgery, can have complications. These can affect how well you recover and your long-term health.
Short-Term Surgical Complications
Bowel resection surgery has risks of immediate complications. These can include:
- Infection: Surgical site infections or intra-abdominal infections can occur.
- Bleeding: Hemorrhage during or after surgery is a risk.
- Adhesions: Scar tissue can form in the abdomen, potentially leading to bowel obstruction.
- Anastomotic leakage: Leaks at the site where the bowel is reconnected can happen.
Medical professionals say, “The risk of complications highlights the need for careful patient selection and precise surgical technique.”
Long-Term Functional Consequences
After bowel resection, some patients face long-term bowel function changes. These can include:
- Changes in bowel habits: Diarrhea or constipation can occur.
- Malabsorption: Depending on the extent and location of the resection, nutrient absorption can be affected.
- Ostomy complications: For those requiring an ostomy, there are risks of skin irritation, pouch leakage, and other complications.
“The impact of bowel resection on quality of life varies among individuals, highlighting the need for personalized care and follow-up.”
Risk Factors for Poor Surgical Outcomes
Certain factors can increase the risk of complications after bowel resection. These include:
- Age: Older patients may have higher risks due to comorbidities.
- Nutritional status: Poor nutrition can impair healing.
- Pre-existing conditions: Conditions like diabetes or heart disease can affect surgical outcomes.
Understanding these risks helps patients and healthcare providers work together. This way, they can minimize risks and improve outcomes.
Recovery and Life After Bowel Resection
After a bowel resection, the care you get is key to a good outcome. It includes immediate care, diet changes, and ongoing check-ups. These steps help you recover well and live a good life.
Immediate Post-Operative Care
Right after surgery, you need careful care to avoid problems. You’ll stay in the hospital for a few days. Doctors will manage your pain, watch for complications, and teach you how to care for yourself at home.
Key aspects of immediate postoperative care include:
- Pain management through medication
- Monitoring for signs of infection or other complications
- Gradual introduction to physical activity
- Education on wound care and ostomy management (if applicable)
Dietary Adjustments and Nutritional Considerations
Changing your diet is important after a bowel resection. You’ll need to eat in a way that helps you feel better and heal faster.
Nutritional considerations include:
- Eating smaller, more frequent meals
- Avoiding foods that can cause discomfort or digestive issues
- Ensuring adequate hydration
- Possibly taking nutritional supplements if recommended by a healthcare provider
Long-Term Follow-Up and Quality of Life
Long-term care is vital to keep an eye on your recovery. Regular visits with your doctor help manage any long-term issues. This improves your quality of life.
Aspects of long-term follow-up include:
- Regular appointments with a gastroenterologist or surgeon
- Monitoring for signs of disease recurrence (if applicable)
- Adjusting dietary and lifestyle habits as needed
- Addressing any concerns or symptoms that arise
Conclusion
Bowel resection is a big surgery that removes part of the intestine. This surgery is performed for various conditions, including cancer and inflammatory bowel disease. This surgery helps treat serious health issues.
A bowel resection summary shows how complex this surgery is. It’s done in different ways, like open surgery or laparoscopic. Knowing why it’s done and how to recover is key for everyone involved.
In short, a colon resection summary and intestinal resection summary stress the importance of careful planning. Patients need a full check-up before surgery, precise surgery, and good care after. This ensures the best results.
Understanding the reasons, methods, and recovery helps patients. It makes their journey through treatment better. And it improves their life after surgery.
FAQ
What is bowel resection surgery?
Bowel resection surgery, also known as colon resection, is a procedure. It removes a part of the intestine. This is done to treat conditions like colorectal cancer and inflammatory bowel disease.
Why is bowel resection surgery necessary?
It’s needed when other treatments don’t work. A healthcare professional will decide if surgery is right after a thorough check-up.
What are the primary indications for bowel resection surgery?
It’s used for colorectal cancer, inflammatory bowel disease, and more. It’s also for diverticulitis, intestinal obstruction, and certain tumors.
How is bowel resection surgery performed?
There are different ways to do it. Open surgery, laparoscopic, and robotic surgery are options. The choice depends on the patient’s needs and the surgeon’s skill.
What are the risks and complications of bowel resection surgery?
Risks include infection and bleeding. There’s also a chance of adhesions and long-term problems. Knowing these risks helps in making informed decisions.
How long does it take to recover from bowel resection surgery?
Recovery takes time. Proper care and follow-up are key. This ensures a smooth healing process and the best outcomes.
What are the dietary adjustments required after bowel resection surgery?
You might need to eat differently. Focus on nutrient-rich foods. Avoid foods that could cause discomfort.
Can bowel resection surgery be performed for inflammatory bowel disease?
Yes, it’s sometimes needed for inflammatory bowel disease. This is to treat complications like narrowing or abscesses.
Is bowel resection surgery a common treatment for colorectal cancer?
Yes, it’s a common treatment for colorectal cancer. The type of surgery depends on the cancer’s stage and location.
What is the difference between a segmental resection and a total colectomy?
Segmental resection removes part of the colon. Total colectomy removes the whole colon. The choice depends on the condition and disease extent.
Can bowel resection surgery be performed for diverticulitis?
Yes, it’s sometimes needed for diverticulitis. This is for complicated cases or when episodes keep coming back.
What is intestinal ischemia, and how is it treated?
Intestinal ischemia happens when blood flow to the intestine is cut off. This can cause damage. Surgery is needed to fix the blood flow and prevent more damage.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK574568/