
A colostomy bag is a medical device used to collect waste. It’s for people who can’t use their colon or anus to pass stool. This is due to various medical or surgical reasons.Discover why would someone need a colostomy bag, medical causes, and long-term management.
Certain medical conditions, like colorectal cancer, inflammatory bowel diseases, and diverticulitis, may need a colostomy. These conditions can damage the colon a lot. So, surgery is needed to make a new path for waste elimination.
Liv Hospital offers trusted, patient-centered care. They ensure high-quality outcomes for those facing colostomy surgery. They provide full support throughout the treatment process.
Key Takeaways
- Colostomy bags are used to collect waste when the colon is damaged or blocked.
- Medical conditions like colorectal cancer and inflammatory bowel diseases may require a colostomy.
- Surgical procedures are necessary to create a colostomy.
- Liv Hospital provides patient-centered care for individuals undergoing colostomy surgery.
- Colostomy bags are an essential intervention for individuals with certain medical conditions.
Understanding Colostomy Bags and Their Purpose
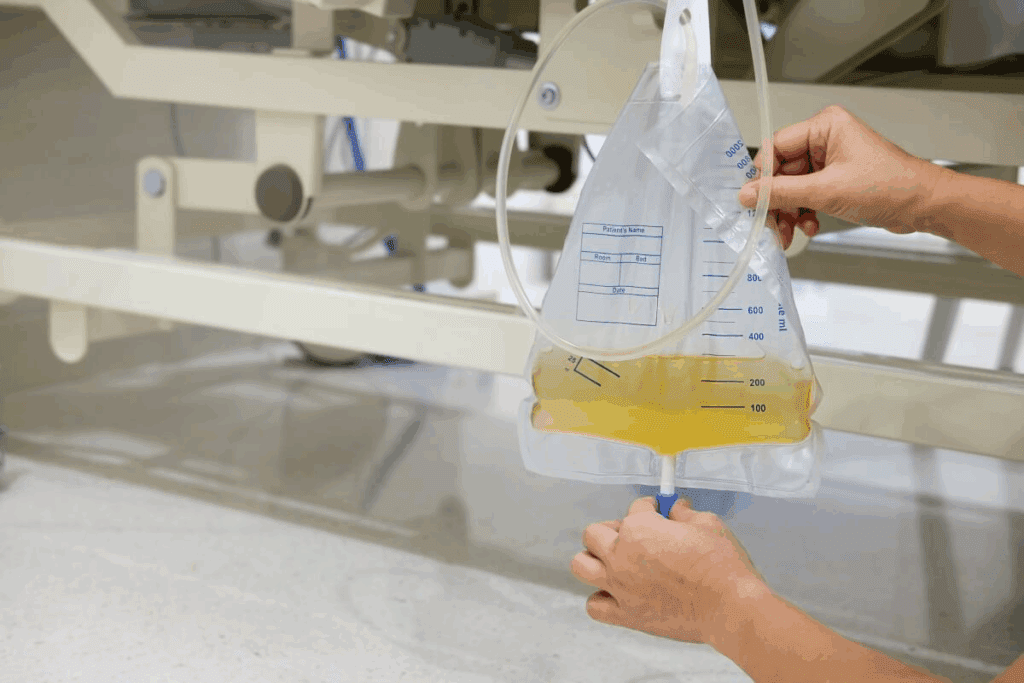
A colostomy bag is a device that collects waste when the body can’t use its natural way. It’s key for people who have had ostomy surgery. This surgery makes an opening in the belly, called a stoma, to move waste.
What Is a Colostomy Bag?
A colostomy bag, or ostomy pouch, is worn outside the body. It’s attached to the stoma, made for waste to leave the body. It’s made to be hidden, comfy, and secure, helping people manage their waste easily.
The bag is made of flexible material for easy wear under clothes. It comes in many sizes and styles to fit different needs. Some bags are for one use, while others can be emptied and used again.
The Surgical Creation of a Stoma
Making a stoma is a big part of ostomy surgery. It involves moving part of the intestine to the belly’s surface. This creates an opening for waste to pass through. The stoma is usually on the left side of the belly, but it can vary.
The surgery is done under general anesthesia. The surgeon brings the intestine to the skin’s surface and secures it with stitches. The stoma takes a few weeks to heal.
Types of Ostomy Appliances
There are many types of ostomy appliances for different needs. The main types are:
- One-piece systems: These are a pouch and adhesive in one unit, easy to apply and remove.
- Two-piece systems: These have a pouch and flange (adhesive barrier) separately, allowing pouch change without removing the flange.
- Closed-end pouches: For one-time use, these are for colostomies with solid stool.
- Drainable pouches: These can be opened for drainage, good for ileostomies or urostomies.
Knowing about these appliances is important for managing your condition well. The right choice depends on personal preference, lifestyle, and stoma needs.
Why Would Someone Need a Colostomy Bag?

People need a colostomy bag for many medical reasons. It’s used when the body can’t move waste normally. This happens due to illness or injury.
Normal Digestive System Function
The digestive system breaks down food into nutrients. It starts in the mouth and goes through the esophagus, stomach, small intestine, and colon. The colon absorbs water and forms stool, which is then passed through the anus.
A healthy digestive system works well, allowing for regular bowel movements. But, some medical conditions can stop this process.
When Natural Waste Elimination Is Compromised
Many medical conditions can make it hard for the bowel to work right. This leads to the need for a colostomy bag. These include:
- Colorectal cancer
- Inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis
- Diverticulitis
- Bowel obstructions
- Trauma or injury to the abdomen
When these conditions severely affect the bowel, a colostomy may be needed.
The Decision-Making Process for Colostomy Surgery
Deciding on colostomy surgery is a big step. It involves talking to healthcare professionals. They assess the medical condition, the damage to the bowel, and the surgery’s benefits.
Those thinking about colostomy surgery should talk to their doctor. They should discuss the risks and benefits to make a well-informed choice.
| Condition | Description | Potential Need for Colostomy |
| Colorectal Cancer | Cancer affecting the colon or rectum | Often requires colostomy |
| Inflammatory Bowel Disease (IBD) | Chronic inflammation of the gastrointestinal tract | May require colostomy in severe cases |
| Diverticulitis | Inflammation of diverticula in the colon | Can require colostomy if complications arise |
Statistics and Prevalence of Colostomy Procedures
In the United States, many people have ostomy surgeries each year. This shows how important it is to know about these surgeries. About 100,000 ostomy surgeries are done annually, showing a big need for them.
Annual Ostomy Surgeries
Every year, the U.S. sees about 100,000 ostomy surgeries. These surgeries include colostomies, ileostomies, and urostomies. They are key in treating many medical conditions.
Demographics of Colostomy Recipients
People from all walks of life get colostomies. Most are older adults. They often get them for conditions like colorectal cancer or diverticulitis. Knowing this helps in giving better support and care.
Temporary vs. Permanent Colostomy Statistics
Colostomies can be either temporary or permanent. It depends on the medical condition and the surgery’s purpose. Many colostomies are temporary, with the chance to reverse them later.
| Type of Colostomy | Percentage | Typical Duration |
| Temporary | 40% | Several months to a few years |
| Permanent | 60% | Lifetime |
The numbers show how different people’s outcomes can be. It also shows the need for care that fits each person’s situation.
Colorectal Cancer as a Leading Cause
Colorectal cancer is a major reason for needing a colostomy. It impacts bowel function a lot. This cancer is common in the colon or rectum and often requires surgery to treat.
How Cancer Affects Bowel Function
Colorectal cancer can block waste flow in the intestines. This leads to severe constipation or bowel obstruction. As the cancer grows, it can spread to nearby tissues and organs, making bowel issues worse.
A tumor can also narrow the bowel, making it hard for stool to move. Sometimes, the cancer blocks the bowel completely, requiring quick medical action.
Surgical Interventions Requiring Colostomy
Surgery is a key treatment for colorectal cancer. Sometimes, this surgery includes creating a colostomy. The choice to do a colostomy depends on the cancer’s location and stage.
If the cancer is in the lower rectum, surgeons might remove part of the rectum. They then create a colostomy to divert waste. This helps patients recover and may allow for more treatment.
Recovery and Adaptation After Cancer Surgery
Recovering from colorectal cancer surgery, like getting a colostomy, takes time. Patients must learn to manage their colostomy. This includes changing the appliance and watching for complications.
With the right care and support, many patients adjust well to life with a colostomy. They can lead active, happy lives. The recovery also includes regular check-ups with doctors to watch for cancer coming back.
Inflammatory Bowel Diseases and Colostomy Necessity
Inflammatory bowel diseases, like Crohn’s and ulcerative colitis, may require a colostomy. These conditions cause inflammation and damage in the digestive tract. This can lead to complications that need surgery.
Crohn’s Disease Complications
Crohn’s disease can affect any part of the digestive tract. It can cause the intestine to narrow, create fistulas, and abscesses. In severe cases, surgery might be needed to remove damaged parts of the intestine, leading to a stoma.
Crohn’s Disease Complications Table
| Complication | Description | Potential Outcome |
| Stricture | Narrowing of the intestine | Surgery to remove the stricture |
| Fistulas | Abnormal connections between the intestine and other organs or the skin | Surgical repair or removal |
| Abscesses | Pockets of infection | Drainage or surgical removal |
Ulcerative Colitis and Surgical Intervention
Ulcerative colitis mainly affects the colon. If medical treatment fails or complications occur, removing the colon might be needed. This can lead to a stoma, either temporarily or permanently.
The decision to undergo surgery is typically considered when:
- Severe symptoms persist despite medical treatment
- Dysplasia or cancer is detected
- Complications such as toxic megacolon occur
Managing IBD with Ostomy Solutions
For those with IBD needing a colostomy, managing life with an ostomy is key. This includes choosing the right ostomy appliance, learning to care for the stoma, and adjusting to lifestyle changes.
Managing IBD with ostomy solutions requires a team effort. Healthcare providers, ostomy nurses, and support groups play a big role. Understanding IBD complications and the role of colostomy helps individuals navigate their treatment and improve their quality of life.
Diverticulitis and Related Complications
Diverticulitis is a condition where the diverticula in the colon get inflamed. This can lead to severe complications, sometimes requiring a colostomy bag. Diverticula are small pouches in the colon wall. When they get inflamed, it causes a lot of pain and can be dangerous.
Acute vs. Chronic Diverticulitis
Diverticulitis can be acute or chronic. Acute diverticulitis happens suddenly, with severe pain, fever, and changes in bowel habits. Chronic diverticulitis is when the inflammation keeps coming back over time. Knowing the difference is key to the right treatment.
Treating diverticulitis depends on its severity and type. Mild cases might just need antibiotics and diet changes. But severe cases or those with complications might need surgery.
Perforation and Peritonitis
Perforation is a serious complication of diverticulitis. It happens when the inflamed diverticulum bursts, leading to peritonitis, an infection in the abdominal cavity. Peritonitis is a medical emergency that needs quick surgery to clean the cavity and find the infection source.
When there’s perforation and peritonitis, a colostomy might be needed. It helps by diverting feces away from the affected area, allowing it to heal. This procedure is often life-saving and is done with other surgeries to treat diverticulitis complications.
Hartmann’s Procedure and Colostomy Formation
Hartmann’s procedure is used in emergencies with complicated diverticulitis, like perforation. It removes the affected colon part and creates a colostomy to divert feces. The remaining rectal stump is closed, and the colostomy lets the area heal.
Hartmann’s procedure is usually temporary. It might be reversed later when the condition improves. The decision to do Hartmann’s procedure depends on the diverticulitis’s severity and the patient’s health.
Bowel Obstructions Requiring Surgical Intervention
Bowel obstructions are serious and often need surgery, which might include a colostomy. These obstructions block the flow of intestinal contents. This can cause severe problems if not treated quickly.
Causes of Intestinal Obstruction
Many things can cause intestinal obstructions. These include adhesions from past surgeries, hernias, tumors, and some inflammatory diseases. Obstructions can be physical or due to functional issues like ileus.
Adhesions are a common cause, often in those who have had abdominal surgery. Hernias can also cause obstructions if they become trapped or cut off blood supply.
Emergency Management and Decompression
Handling bowel obstructions as emergencies starts with stabilizing the patient. This includes giving fluids and fixing electrolyte imbalances. It’s key to relieve the blockage to avoid serious issues like ischemia or perforation.
Decompression can be done with nasogastric suction or a colostomy tube. The choice depends on the type and location of the blockage.
Recovery and Possible Reversal
After surgery, patients need close monitoring to avoid complications. Whether a colostomy can be reversed depends on the cause of the blockage and the surgery done.
If the blockage is temporary, like from inflammation, reversal might be possible. But if it’s due to something permanent, like a tumor, the colostomy could be permanent.
Trauma and Emergency Situations
In severe trauma cases, a colostomy might be needed. This is often due to injuries in the abdominal area. Such injuries can harm the digestive system, making surgery urgent.
Abdominal Injuries and Surgical Interventions
Severe injuries to the abdomen can happen from accidents or falls. These injuries can damage the digestive tract. Damage control surgery is used to stabilize the patient and treat critical injuries.
Doctors might decide on a colostomy during emergency surgery. This is to keep fecal matter away from the injured area. It helps the area heal and can save lives if the colon is badly damaged.
Battlefield and Accident Trauma
Combat or severe accidents can cause complex injuries. A colostomy might be needed to manage these injuries. This is true for military personnel and accident victims.
Battlefield trauma is challenging due to the remote settings. Damage control surgery helps by stabilizing patients for further care.
Damage Control Surgery and Temporary Colostomy
Damage control surgery is for emergency situations. It aims to control bleeding and stabilize the patient. A temporary colostomy might be created to help the lower GI tract heal.
Temporary colostomies can be reversed when the patient recovers. The decision to reverse depends on the patient’s health and the injury’s extent.
Congenital Conditions and Birth Defects
Some babies are born with issues in their gut that need a colostomy. This surgery makes a hole in the belly for waste. It’s often needed for kids with digestive problems from birth.
Hirschsprung’s Disease
Hirschsprung’s disease means some parts of the colon don’t have nerve cells. This causes trouble with bowel movements. A colostomy is often needed to fix this and help the child go to the bathroom normally.
Doctors usually find Hirschsprung’s in babies early. Signs include trouble passing the first stool, a big belly, and vomiting. Quick treatment is key to avoid serious problems like enterocolitis.
Imperforate Anus and Anorectal Malformations
Imperforate anus means the rectum doesn’t connect to the anus. This makes it hard for stool to pass. The problem can be mild or very serious.
To fix it, surgery is needed. Often, a colostomy is done first. This helps by moving waste away from the bad area, making later surgery easier.
Pediatric Colostomy Management and Outcomes
Looking after a colostomy in kids is very important. It depends on their health, the reason for the colostomy, and future surgeries. Parents and caregivers are key in caring for the colostomy, changing bags, watching for problems, and helping the child feel good.
The future for kids with colostomies can be good. It depends on their condition and surgery success. New ways to care for ostomies and surgery have made life better for these kids. They can now live happy, active lives.
Neurological Disorders Affecting Bowel Function
Neurological conditions can cause severe bowel problems. For some, a colostomy is needed. The impact on bowel function varies by condition and severity.
Spinal Cord Injuries and Neurogenic Bowel
Spinal cord injuries can lead to neurogenic bowel. This is when normal bowel function is lost due to nerve damage. It can cause chronic constipation, fecal incontinence, or bowel obstruction.
Managing neurogenic bowel often includes medications, bowel training, and sometimes surgery like colostomy. The aim is to improve bowel function and quality of life.
Multiple Sclerosis and Parkinson’s Disease
Multiple sclerosis and Parkinson’s disease can severely affect bowel function. In multiple sclerosis, nerve damage from demyelination can cause bowel problems.
Parkinson’s disease can lead to constipation and fecal incontinence due to neuron loss. For both, colostomy might be considered if other treatments don’t work.
“For patients with severe bowel dysfunction due to neurological disorders, colostomy can be a life-changing intervention, improving not only their physical health but also their overall well-being and quality of life.”
Quality of Life Improvements with Colostomy
Though colostomy surgery seems scary, many patients see big improvements in their life quality afterward. It helps manage bowel dysfunction, reducing risks of complications like bowel obstruction or fecal incontinence.
- Enhanced dignity and confidence
- Reduced risk of bowel-related complications
- Improved overall well-being
For those with neurological disorders affecting bowel function, colostomy is a potentially life-changing treatment. Understanding the link between these conditions and bowel issues helps healthcare providers support patients in making informed care decisions.
Conclusion: Living with a Colostomy
Learning to live with a colostomy bag is all about understanding and managing your care. You can lead an active life by taking good care of your stoma and appliance.
Good ostomy care means keeping your stoma clean and checking it often. Using the right products and handling any problems is key. Getting help from doctors, support groups, and online resources makes a big difference.
Having a colostomy means making some changes in your life. But, many people find the health benefits and better quality of life worth it. Knowing why you had the surgery helps you deal with your situation better.
Being proactive with your ostomy care and getting help when you need it helps you thrive. It lets you stay independent and live well with a colostomy bag.
FAQ
What causes a colostomy bag?
A colostomy bag is usually needed because of a medical issue or injury. This can be due to colorectal cancer, inflammatory bowel disease, or diverticulitis. Surgery is often required to create a stoma.
Why do people get ostomy bags?
Ostomy bags are needed for many reasons. This includes colorectal cancer, inflammatory bowel disease, and diverticulitis. They are also used for bowel obstructions, trauma, or conditions present at birth.
What are the reasons for having a colostomy bag?
There are several reasons for needing a colostomy bag. These include colorectal cancer, inflammatory bowel disease, and diverticulitis. It’s also used for bowel obstructions, trauma, and conditions present at birth.
Is a colostomy bag temporary or permanent?
A colostomy bag can be either temporary or permanent. It depends on the medical condition and surgery type. Temporary ones help the bowel heal. Permanent ones are for long-term or lifelong bowel diversion.
How does a colostomy bag affect daily life?
Living with a colostomy bag requires some adjustments. You’ll need to manage ostomy care and adapt to bowel changes. It also involves coping with the emotional aspects. But, with the right care and support, many lead active and fulfilling lives.
Can you live a normal life with a colostomy bag?
Yes, many people with colostomy bags live normal, active lives. They make some adjustments to their routines and habits. With proper care, they can travel, participate in activities, and maintain social relationships.
What are the complications associated with colostomy bags?
Complications with colostomy bags include skin irritation and stoma issues. There’s also the risk of bowel obstruction and emotional challenges. Regular care with a healthcare provider can help reduce these risks.
How is a colostomy bag managed?
Managing a colostomy bag involves regular care. This includes cleaning and changing the appliance and monitoring for complications. Individuals often work with healthcare providers or ostomy nurses to create a care plan.
References
Garruti, G., et al. (2018). Cholecystectomy: a way forward and back to metabolic disease? Current Opinion in Lipidology, 29(3), 189-195. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8114797




































