Last Updated on October 28, 2025 by
We are seeing a big change in cancer treatment with CAR T therapy. This new treatment is changing how we fight cancer.
CAR T-cell therapies are very effective against certain cancers. They work by guiding T cells to find and destroy cancer cells.
The FDA’s approval has helped make these treatments available to patients. We aim to provide top-notch healthcare and support to patients worldwide.
Key Takeaways
- CAR T therapy is a groundbreaking treatment for blood cancers.
- FDA-approved CAR T-cell therapies have shown significant efficacy.
- Chimeric antigen receptor technology is revolutionizing oncology.
- CAR T-cell therapies target specific cancer cells.
- We are committed to delivering comprehensive care for global patients.
The Revolutionary Approach of CAR T Therapy in Modern Medicine

CAR T cell therapies have changed the game in fighting cancer. They use the body’s immune system to attack cancer cells. This is a big step forward in treating certain cancers.
Defining Chimeric Antigen Receptor T-Cell Therapy
CAR T cell therapy is a way to fight cancer with the immune system. It starts by taking T cells from the blood. Then, these cells are changed to find and kill cancer cells.
This personalized approach makes T cells better at finding and destroying cancer cells. It’s a new way to treat cancer.
The Transformation of Cancer Treatment Paradigms
CAR T therapy has changed how we treat cancer. It’s a targeted way to fight cancer, unlike old treatments like chemotherapy. CAR T cell therapies aim to only harm cancer cells, not healthy ones.
| Treatment Aspect | Traditional Cancer Treatments | CAR T Cell Therapies |
|---|---|---|
| Targeting | Non-specific, affecting both cancerous and healthy cells | Specific to cancer cells, minimizing damage to healthy cells |
| Treatment Approach | Often involves chemotherapy and radiation | Involves genetic modification of T cells to fight cancer |
| Side Effects | Can have severe side effects due to non-specific targeting | Can have unique side effects such as cytokine release syndrome |
Understanding CAR T therapy shows its big impact on cancer treatment. As research grows, CAR T cell therapies are getting better. They offer new ways to treat cancer and help patients more.
How CAR T Cell Technology Works to Fight Cancer
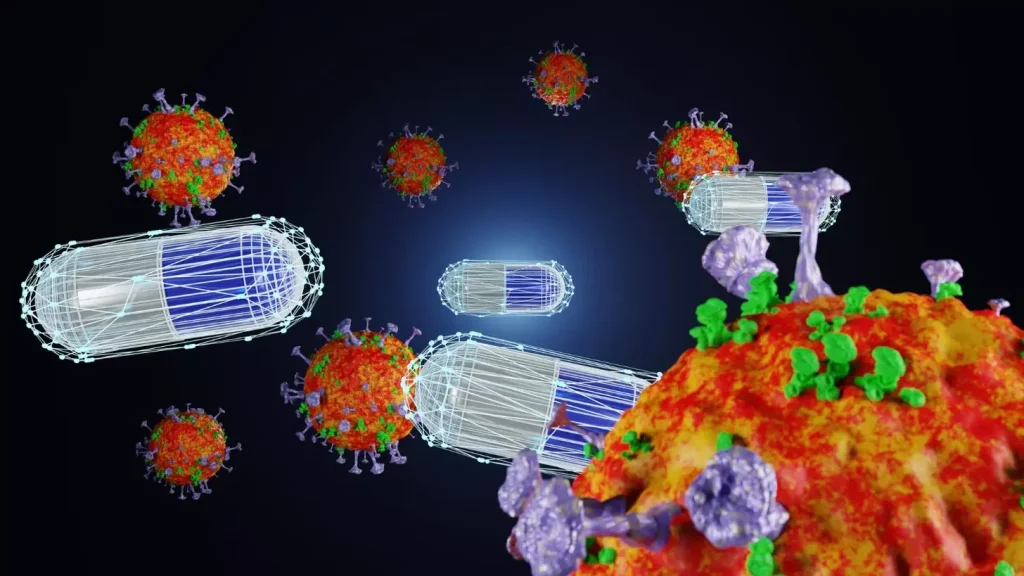
CAR T cell technology starts by taking T cells from a patient. These cells are then changed to spot cancer cells. After that, they are put back into the patient. This method has shown great promise in fighting different cancers.
The Engineering Process Behind CAR-T Cells
The journey starts with leukapheresis, a method to collect T cells from the blood. These T cells are then taken to a lab. There, they are made to carry a chimeric antigen receptor (CAR) that finds specific cancer antigens.
The steps to modify the T cells include:
- Isolating T cells from the patient’s blood
- Genetically engineering these T cells to produce CARs
- Expanding the modified T cells to sufficient numbers
- Cryopreserving the CAR-T cells until they are ready for reinfusion
When the CAR-T cells are ready, they are given back to the patient. They can then find and attack cancer cells better.
Targeting Specific Cancer Antigens
CAR-T cells are made to find specific cancer antigens on cancer cells. For example, they might target the CD19 antigen in some leukemias and lymphomas. This way, they can kill cancer cells without harming healthy ones.
The precision of CAR-T cells is a big plus. They can:
- Recognize and bind to cancer cells
- Start an immune attack on the cancer cells
- Grow and stay in the body to keep fighting cancer
Understanding CAR T cell technology shows its huge promise in changing cancer treatment. It lets us make T cells that can find and attack specific cancer markers. This opens up new ways to fight cancer effectively.
The Journey from Laboratory to FDA Approval for CAR T Cell Therapies
The path to FDA approval for CAR T cell therapies is complex. It involves rigorous clinical trials and detailed data analysis. Understanding the stages and challenges is key to bringing these therapies to patients.
Clinical Trial Requirements for CAR T Treatments
Clinical trials for CAR T cell therapies check their safety and effectiveness. These trials have several phases. Phase 1 focuses on safety and dosing. Phases 2 and 3 evaluate how well the treatment works compared to current treatments.
The National Cancer Institute says these trials are vital. They help us understand how CAR T cell therapies work in different patients.
The trial process is long and requires careful monitoring. For example, the FDA approved the first CAR T-cell therapy in 2017 for children with acute lymphoblastic leukemia (ALL). This was a big step forward.
Key aspects of clinical trials for CAR T therapies include:
- Patient selection criteria
- Dosing and administration protocols
- Efficacy endpoints
- Safety monitoring
Demonstrating Efficacy and Managing Toxicity
One big challenge in CAR T cell therapy is showing it works while managing side effects. CAR T therapies are very effective against some blood cancers. But, they can cause severe side effects like cytokine release syndrome (CRS).
To tackle this, researchers and doctors have found ways to reduce CRS and other toxicities. They use tocilizumab, an FDA-approved treatment for CRS, and other supportive care.
“The development of CAR T cell therapies has been a game-changer in the treatment of certain blood cancers. But, managing the toxicities is a big challenge.” – Dr. [Name], CAR T cell therapy researcher
Regulatory Milestones in CAR T Development
The FDA has approved seven CAR T cell therapies for blood cancers. Recent updates have made these treatments more accessible. These milestones show the ongoing effort to improve patient outcomes.
To show the regulatory process, let’s look at some key milestones in a table:
| Regulatory Milestone | Description | Year |
|---|---|---|
| First CAR T-cell therapy approval | FDA approves tisagenlecleucel for children with ALL | 2017 |
| Expanded approval | FDA expands approval for axicabtagene ciloleucel to include relapsed or refractory large B-cell lymphoma | 2018 |
| Label updates | FDA reduces monitoring requirements for certain CAR T therapies | Recent |
The journey from lab to FDA approval is just the start. Ongoing research and updates will shape the future of these treatments.
Seven FDA-Approved CAR T Cell Therapies for Blood Cancers
CAR T cell therapy is a new hope for blood cancer patients. Seven FDA-approved therapies have changed oncology. They offer hope for leukemia and lymphoma patients.
Comprehensive Overview of Approved Therapies
The FDA has approved several CAR T cell therapies. Tisagenlecleucel (Kymriah) and Axicabtagene ciloleucel (Yescarta) were first. They treat relapsed or refractory large B-cell lymphoma and some leukemia types.
Lisocabtagene maraleucel (Breyanzi) is for large B-cell lymphoma. Idecabtagene vicleucel (Abecma) is for multiple myeloma. Each therapy has shown safety and effectiveness in clinical trials.
- Tisagenlecleucel (Kymriah) for pediatric and adult B-cell acute lymphoblastic leukemia and large B-cell lymphoma.
- Axicabtagene ciloleucel (Yescarta) for large B-cell lymphoma.
- Lisocabtagene maraleucel (Breyanzi) for large B-cell lymphoma.
- Idecabtagene vicleucel (Abecma) for multiple myeloma.
- Ciltacabtagene autoleucel (Carvykti) for multiple myeloma.
- Brexucabtagene autoleucel (Tecartus) for mantle cell lymphoma and acute lymphoblastic leukemia.
- Lisocabtagene maraleucel (Breyanzi) for large B-cell lymphoma.
Target Populations and Specific Cancer Types
These therapies target blood cancers like leukemia, lymphoma, and multiple myeloma. They cover various cancer types and patient groups. This shows the complexity of blood cancers.
Tisagenlecleucel (Kymriah) targets CD19 in B-cell ALL and lymphoma. Knowing the target populations and cancer types is key for choosing the right treatment.
| Therapy | Target Cancer | Target Population |
|---|---|---|
| Tisagenlecleucel (Kymriah) | B-cell ALL, Large B-cell lymphoma | Pediatric and adult patients |
| Axicabtagene ciloleucel (Yescarta) | Large B-cell lymphoma | Adult patients |
| Lisocabtagene maraleucel (Breyanzi) | Large B-cell lymphoma | Adult patients |
As research grows, we’ll see more uses for these therapies. This could offer new options for more patients.
The Complete CART Therapy Process from Extraction to Reinfusion
The journey to CAR T cell therapy has several steps. It starts with an initial evaluation and ends with the final reinfusion. We will explain the whole process of CAR T cell therapy.
Patient Evaluation and Selection Criteria
The first step is patient evaluation. We check if a patient is eligible for CAR T cell therapy. This includes looking at their medical history and current health status. Eligibility criteria often include specific cancer types and previous treatment outcomes.
We consider many factors during the evaluation. These include the patient’s overall health and the stage of their cancer. We also look at any previous treatments they have had. This helps us decide if CAR T cell therapy is the right choice.
T Cell Collection Through Apheresis
After checking eligibility, the next step is T cell collection. This is done through a process called apheresis. Apheresis takes a few hours and is done on an outpatient basis.
Apheresis uses a machine to separate T cells from the patient’s blood. The remaining blood is then returned to the patient. This step is important because it provides the T cells needed for CAR-T cells.
Laboratory Modification to Create CAR-T Cells
After collection, the T cells go to a laboratory for modification. Here, they are genetically modified to become CAR-T cells. This makes them better at recognizing and targeting cancer cells.
The modification process includes several steps. These include gene transfer and cell expansion. The result is CAR-T cells that are designed to target the patient’s cancer.
| Laboratory Process | Description |
|---|---|
| Gene Transfer | Introduction of the CAR gene into T cells |
| Cell Expansion | Growing the modified T cells to sufficient numbers |
| Quality Control | Testing the CAR-T cells for efficacy and safety |
Reinfusion Protocol and Immediate Monitoring
The final step is the reinfusion of CAR-T cells into the patient. This is done through an intravenous infusion. After reinfusion, patients are closely monitored for any immediate reactions or side effects.
Monitoring includes watching for signs of cytokine release syndrome (CRS). We also provide supportive care for any symptoms that may arise.
“CAR T cell therapy represents a significant advancement in the treatment of certain cancers, giving new hope to patients who have not responded to other treatments.”
Recent FDA Updates Expanding Access to CAR T Cell Therapy
The FDA has made big changes to CAR T cell therapy rules. Now, more patients can get this life-saving treatment. These updates are a big step towards making it more available.
Reduced Monitoring Requirements and Their Impact
One major change is less monitoring for CAR T cell therapy patients. Before, they had to stay close to the treatment center for weeks. Now, they can go home sooner.
Reduced monitoring brings many benefits:
- Patients feel more comfortable and less stressed.
- It costs less because they don’t have to stay in the hospital as long.
- Healthcare resources are used better.
Expanded Patient Eligibility Criteria
The FDA has also made it easier for more patients to get CAR T cell therapy. Now, people with certain health issues or who have tried other treatments can qualify.
These changes mean:
- More people can get this treatment.
- More patients have access to a potentially life-saving option.
- More patients can join clinical trials.
Outpatient Administration Possibilities
Another update is the chance to give CAR T cell therapy outside the hospital. This is being looked into but could be a big change in the future.
Outpatient CAR T cell therapy could change how it’s given. It could save money, improve life quality, and reach more people.
As we watch CAR T cell therapy evolve, these FDA updates are leading to better care. They make the treatment more focused on the patient and more efficient.
Treatment Outcomes: 30,000 Patients and Counting
Over 30,000 patients worldwide have been treated with CAR T cell therapy. This treatment offers hope for those with certain blood cancers. As we learn more, we see how effective it is and its promise for long-term survival.
Statistical Analysis of Response Rates
Clinical trials show CAR T-cell therapies can clear advanced cancers in many patients. Some even achieve apparent cures. The response rates are impressive, with complete remission rates from 50% to 90% in some groups. This highlights CAR T cell therapy’s big impact on blood cancer treatment.
Several factors affect how well CAR T cell therapy works. These include:
- The type of cancer being treated
- The patient’s health and past treatments
- The CAR T cell product and its making process
Long-term Survival Data
Long-term survival data shows CAR T cell therapy’s true power. Many patients who fully respond stay disease-free for years. For example, up to 40% of patients with certain lymphomas survive 5 years.
Here’s a table showing long-term survival data from CAR T cell therapy studies:
| Study | Cancer Type | 5-Year Survival Rate |
|---|---|---|
| Study A | Relapsed/refractory lymphoma | 35% |
| Study B | Refractory leukemia | 28% |
| Study C | Advanced multiple myeloma | 42% |
Quality of Life Assessments Post-Treatment
It’s important to look at patients’ quality of life after treatment. Many see big improvements, like those who fully respond.
Studies show patients often feel:
- Less symptoms
- Better physical function
- Improved emotional health
As CAR T cell therapy gets better, we’ll see even more positive results. Ongoing research and new technologies promise to help more patients.
Managing Side Effects of CAR T Immunotherapy
Managing side effects of CAR T immunotherapy is key for patients’ well-being. This treatment, while groundbreaking, has side effects that need careful attention.
Cytokine Release Syndrome: Recognition and Treatment
Cytokine release syndrome (CRS) is a common side effect of CAR T-cell therapies. It causes symptoms like high fever and low blood pressure. We spot CRS by its symptoms, which can be mild or severe.
Treatment for CRS includes supportive care like hydration and antipyretics. In severe cases, tocilizumab, an anti-IL-6 receptor antibody, is used.
CRS can vary in severity. It’s important to identify patients at higher risk. We use grading systems to assess severity and guide treatment. Early recognition and treatment are critical.
Neurological Toxicities and Their Management
Neurological toxicities, like encephalopathy and aphasia, can happen after CAR T cell infusion. We manage these with supportive care, including seizure prophylaxis and monitoring for increased intracranial pressure. Corticosteroids may be used to reduce inflammation.
The causes of neurological toxicities are complex and not fully understood. We’re researching to improve management. It’s important to educate patients on the risks and signs of these toxicities.
Long-term Monitoring Protocols
Long-term monitoring after CAR T cell therapy is essential. It helps catch late effects like prolonged cytopenias or secondary malignancies. We closely follow patients with regular blood counts and diagnostic tests.
A multidisciplinary team, including hematologists, oncologists, and primary care physicians, is involved in patient follow-up. We stress the importance of attending follow-up appointments and reporting new symptoms promptly.
Innovations in CAR T Cell Technology to Overcome Resistance
Researchers are working hard to improve CAR T cell therapy. They aim to beat resistance and help more patients with cancer. This is key for better results in fighting cancer.
Multi-Target CAR Approaches
One big step is making CAR T cells that can hit multiple targets. This way, tumors are less likely to hide from the treatment. Studies show these multi-target CAR T cells are very effective.
Now, we’re seeing CAR T cells that can find and attack different parts of tumors. This makes the treatment stronger and less likely to fail.
Enhancing CAR T Cell Persistence
Another area of focus is making CAR T cells last longer in the body. They need to stick around to kill all the cancer cells. Scientists are looking at ways to keep CAR T cells alive and growing.
Tests show that CAR T cells that last longer work better. We’re trying to make these strategies even better for lasting results.
Combination Therapies to Improve Outcomes
Combining CAR T cells with other treatments is also being explored. This mix aims to make the therapy more effective and fight resistance. It’s a promising way to help patients more.
| Combination Therapy | Mechanism | Potential Benefit |
|---|---|---|
| CAR T + Checkpoint Inhibitors | Enhances T cell activation | Improved antitumor efficacy |
| CAR T + Oncolytic Viruses | Selective tumor lysis | Enhanced tumor antigen release |
We’re testing different combinations to find the best ones. Our goal is to get stronger and longer-lasting results while keeping side effects low.
Beyond Cancer: CAR T Research for Autoimmune Conditions
CAR T cell technology is being tested in clinical trials for various autoimmune conditions. This offers new hope for patients. We’ve seen CAR T therapy change cancer treatment. Now, researchers are exploring its use in autoimmune diseases.
CAR T cell therapy has changed oncology. It’s now being tested for autoimmune conditions. Autoimmune diseases happen when the body attacks itself. Scientists hope to reset the immune system with CAR T technology. This could lead to long-term remission for patients.
Promising Results in Lupus Clinical Trials
Lupus is a chronic autoimmune disease that affects many parts of the body. Recent trials show CAR T cell therapy is promising for lupus patients. The therapy has been observed to significantly reduce disease activity and improve the quality of life for these patients.
Adapting CAR T Technology for Non-Cancer Applications
Adapting CAR T technology for autoimmune diseases requires understanding the disease’s pathology. Researchers are working to find specific targets for CAR T cells. This will help modulate the immune response without broad immunosuppression.
Challenges in Treating Autoimmune Diseases with CAR T
While results are promising, there are challenges. One concern is CAR T cells causing significant immune suppression. This makes patients vulnerable to infections. There’s also a need for long-term follow-up to monitor for late effects.
| Condition | CAR T Target | Clinical Trial Phase |
|---|---|---|
| Lupus | CD19 | Phase 2 |
| Rheumatoid Arthritis | CD4 | Phase 1 |
| Multiple Sclerosis | CD20 | Pre-clinical |
As research advances, CAR T cell therapy may become a valuable treatment for autoimmune conditions. Ongoing and future trials will be key in determining its safety and efficacy.
Conclusion: The Evolving Future of CAR T Therapy
CAR T therapy is a new way to fight cancer and maybe other diseases too. It’s getting better fast, thanks to new tech and ideas. This makes it safer and more effective.
The future looks bright for CAR T therapy. Scientists are working hard to make it even better. They want to make it work for more people and with fewer side effects.
As CAR T therapy gets better, more people will be able to get it. It might even be possible to get it without staying in the hospital. This will make it easier for people to get the treatment they need.
CAR T therapy is changing how we fight cancer. It’s going to be a big part of healthcare in the future. Thanks to new ideas and research, it will help more people get the care they deserve.
What is CAR T cell therapy?
CAR T cell therapy is a way to fight cancer. It starts by taking T cells from your blood. Then, these cells are changed to find and kill cancer cells. After that, they are put back into your body.
How does CAR T cell therapy work?
It works by making T cells find and attack cancer cells. This is done by adding a special receptor to the T cells. This receptor helps them spot and destroy cancer cells.
What types of cancer can CAR T cell therapy treat?
It mainly treats blood cancers like leukemia and lymphoma. These are cancers that other treatments haven’t worked for.
What is the process of CAR T cell therapy?
The process includes several steps. First, you’re checked to see if you’re a good candidate. Then, T cells are collected from your blood. Next, these cells are changed in a lab to make CAR-T cells. Lastly, the CAR-T cells are put back into your body.
What are the side effects of CAR T cell therapy?
Side effects can include cytokine release syndrome and infections. These can be managed with the right care and monitoring.
How has the FDA expanded access to CAR T cell therapy?
The FDA has made it easier to get CAR T cell therapy. They’ve reduced monitoring needs and made more people eligible. They’re also looking into treating patients outside of the hospital.
What are the outcomes of CAR T cell therapy?
Many patients have seen their cancer shrink or even disappear. This has led to better survival rates and quality of life.
Can CAR T cell therapy be used for autoimmune conditions?
Yes, research is looking into using CAR T cell therapy for conditions like lupus. Early trials show promising results.
What innovations are being made in CAR T cell technology?
New ideas include making CAR T cells target more than one cancer type. They’re also working on making these cells last longer in the body. This could lead to better treatment results and ways to fight resistance.
What is the future of CAR T therapy?
The future looks bright with ongoing research and new ideas. It could help treat more than just cancer, giving hope to many patients.
How is CAR T cell therapy managed for side effects?
Managing side effects involves treating cytokine release syndrome and neurological issues. Long-term monitoring is also key to keeping patients safe.
Are there different types of CAR T cell therapies?
Yes, there are several CAR T cell therapies approved by the FDA. Each targets different cancers and patient groups. Researchers are always working on new and better treatments.





