Last Updated on October 28, 2025 by
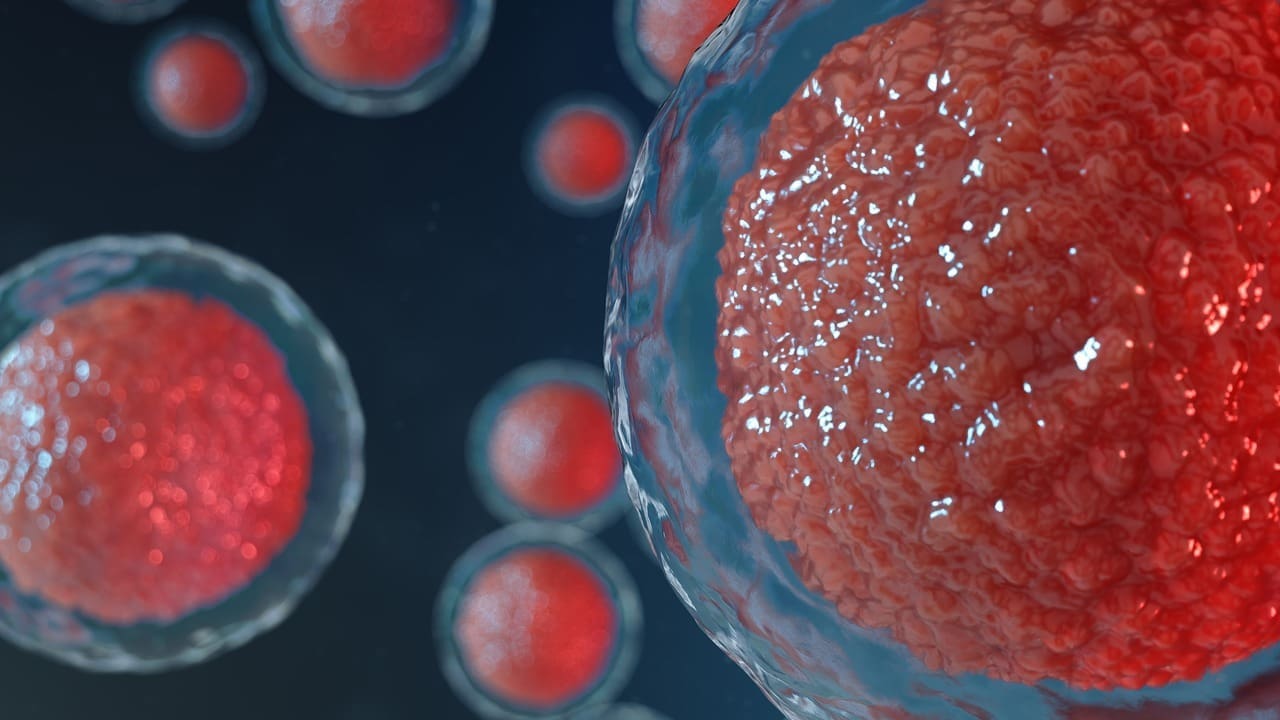
At Liv Hospital, we aim to offer top-notch healthcare to all patients. Hematopoietic stem cells (HSCs) are key in making blood and immune cells all our lives.
These cells are at the top of the blood and immune system’s cell line. They create every blood and immune cell type. We’ll dive into the important facts about HSCs and their lineage. This will help us understand their role in health and sickness.
Knowing how HSCs can grow and change into different cell types shows their big role in the blood system.
Key Takeaways
- HSCs are vital for making blood and immune cells.
- They can grow and change into many cell types.
- HSCs are key in the blood system.
- Learning about HSCs helps us see their role in health and sickness.
- Liv Hospital is dedicated to giving the best healthcare.
The Fundamental Nature of Hematopoietic Stem Cells
Hematopoietic stem cells have special abilities that help them support blood cell production forever. They can renew themselves and turn into different cell types. This makes them key for keeping the right balance of blood cells in our bodies.
Definition and Core Properties
Hematopoietic stem cells are multipotent stem cells that can become all blood cell types. Their ability to do this is a key feature of HSCs. It lets them make cells from both the myeloid and lymphoid lineages. Research in Nature shows how important understanding these properties is for knowing their role in making blood cells.
Self-Renewal Capacity
The ability of hematopoietic stem cells to renew themselves is vital for making blood cells for life. This lets HSCs replace themselves, keeping a steady supply of stem cells. The balance between renewing themselves and differentiating is very important. If this balance is off, it can cause blood disorders.
| Property | Description | Importance |
|---|---|---|
| Multipotency | Ability to differentiate into multiple blood cell types | Essential for producing all blood cells |
| Self-Renewal | Capacity to replenish themselves | Critical for maintaining a lifelong supply of stem cells |
| Regulation | Tight regulation of self-renewal and differentiation | Prevents blood disorders |
Understanding Hematopoietic Stem Cells and Their Unique Abilities

Hematopoietic stem cells (HSCs) are special cells. They can turn into all kinds of blood cells. This is key for making blood cells throughout our lives.
Multipotency Explained
Multipotent hematopoietic stem cells can become many different blood cell types. They can make red blood cells, platelets, and white blood cells. These cells are vital for carrying oxygen, clotting blood, and fighting off infections.
A leading researcher said,
“The multipotency of HSCs is a critical feature that enables the hematopoietic system to respond to the body’s needs for different types of blood cells.”
This skill helps the body keep a good balance of blood cells. It also helps the body fight off stress or injury.
Lifelong Blood Cell Production
Hematopoietic cells from HSCs are key for making blood cells forever. They start as HSCs, then become progenitor cells, and then mature into different blood cells. This process is controlled by the cells themselves and signals from the bone marrow.
| Cell Type | Function | Lineage |
|---|---|---|
| Red Blood Cells | Oxygen Transport | Myeloid |
| Platelets | Blood Clotting | Myeloid |
| T Cells | Immune Response | Lymphoid |
| B Cells | Immune Response | Lymphoid |
The hemopoetic or hematopoeitic system depends on HSCs to keep blood cells balanced. Knowing how HSCs work is important for finding new treatments for blood disorders.
The Distinction Between HSCs and Hematopoietic Progenitor Cells
It’s important to know the difference between hematopoietic stem cells (HSCs) and hematopoietic progenitor cells (HPCs). Both are key to the hematopoietic system. Yet, they have unique traits that make them different.
Functional Differences
HSCs can grow and turn into any blood cell type. On the other hand, HPCs can only grow into certain types of blood cells.
Proliferation vs. Self-Renewal Capabilities
The main difference is in how much they can grow and renew themselves. HSCs can renew themselves a lot, keeping the stem cell pool alive for a lifetime.
Short-Term vs. Long-Term Repopulating Cells
HSCs are divided into short-term and long-term repopulating cells. Long-term repopulating HSCs keep producing blood cells for life. Short-term repopulating cells have a shorter time of activity.
| Cell Type | Self-Renewal Capacity | Lineage Commitment |
|---|---|---|
| HSCs | High | Multipotent |
| HPCs | Limited | Oligopotent/Unipotent |
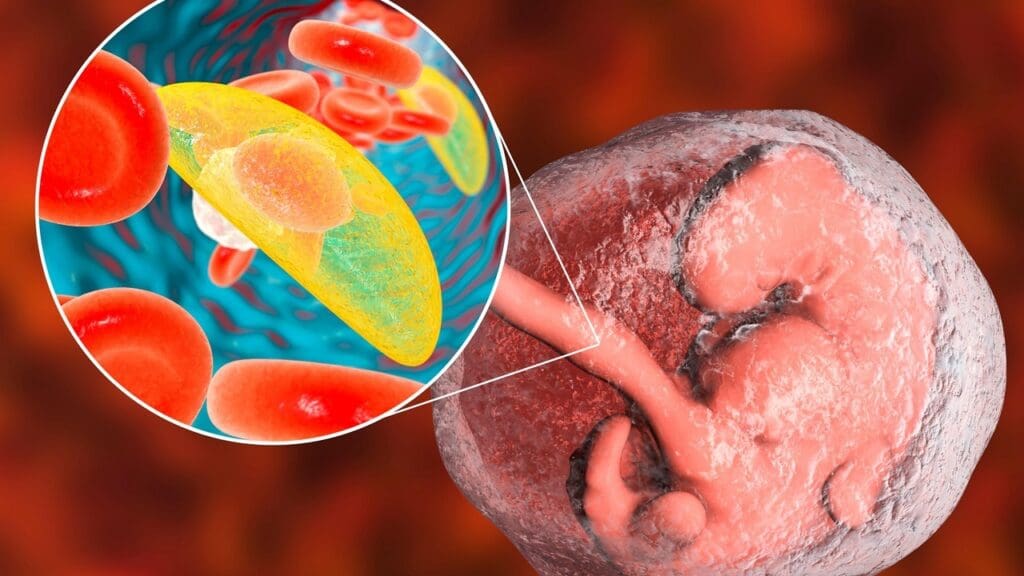
Exploring the Complete Hematopoietic Hierarchy
The process of making blood cells is like a tree, showing how stem cells turn into different types of blood cells. This tree model helps us understand how blood cells are made.
The Classical Tree Model of Hematopoiesis
The blood cell-making process is shown as a tree. At the base are hematopoietic stem cells (HSCs). These cells turn into different types of cells as they move up the tree.
Stages of Differentiation
The journey from stem cells to blood cells has many steps. Multipotent HSCs become multilineage progenitor cells. Then, these cells turn into more specific types of cells.
From Stem Cells to Mature Blood Cells
The last step is when cells become fully formed blood cells. This includes red blood cells, platelets, and white blood cells. Here’s a table that shows the main stages in making blood cells:
| Stage | Cell Type | Description |
|---|---|---|
| 1 | HSCs | Multipotent stem cells capable of self-renewal |
| 2 | Multilineage Progenitors | Progenitor cells with limited self-renewal capacity |
| 3 | Lineage-Restricted Progenitors | Progenitors committed to specific blood cell lineages |
| 4 | Mature Blood Cells | Fully differentiated cells, including red blood cells, platelets, and white blood cells |
Knowing about the hematopoietic hierarchy helps us understand how blood cells are made. It shows the important role of HSCs in creating new blood cells throughout our lives.
Myeloid and Lymphoid Pathways in Blood Cell Development
HSCs create all blood and immune system cells through the myeloid and lymphoid pathways. These two main paths lead to different blood and immune cells.
The Myeloid Lineage and Its Derivatives
The myeloid lineage makes many blood cells. These include:
- Erythrocytes (red blood cells)
- Megakaryocytes (platelet-producing cells)
- Granulocytes (such as neutrophils, eosinophils, and basophils)
- Monocytes (which mature into macrophages)
These cells are key for oxygen transport, blood clotting, and fighting off infections.
The Lymphoid Lineage and Immune Cell Formation
The lymphoid lineage creates lymphocytes, which are vital for our immune system. The main types are:
- B cells (responsible for antibody production)
- T cells (involved in cell-mediated immunity)
- Natural Killer (NK) cells (which play a role in innate immunity)
These immune cells help protect us from infections and diseases.
In summary, the myeloid and lymphoid lineages are key for making different blood and immune cells. This shows how complex and important blood cell production is.
Terminology Variations in Hematopoietic Science
In hematopoietic science, spelling and terminology can vary. This makes it important to know the right terms. The field uses different words and abbreviations for hematopoietic stem cells (HSCs) and related ideas.
Alternative Spellings: Haematopoietic, Hemopoetic, and Hematopoietic
The spelling of “hematopoietic” changes in different places. In American English, it’s spelled “hematopoietic.” But in British English, it’s “haematopoietic.” You might also see “hemopoetic,” but it’s not as common. All these terms mean the same thing: how blood cells are made.
| Spelling Variation | Regional Preference | Usage Context |
|---|---|---|
| Hematopoietic | American English | Research papers, clinical reports |
| Haematopoietic | British English | Research papers, clinical reports |
| Hemopoetic | Less common | Older literature, some research contexts |
HSC Medical Abbreviation and Clinical Terminology
The “HSC” abbreviation stands for Hematopoietic Stem Cells. In medical settings, knowing this is key for clear communication. The HSC medical abbreviation is often talked about in hematopoietic stem cell transplants and regenerative medicine.
“The use of HSCs in clinical settings has revolutionized the treatment of various hematological disorders.”
We know that the terms and abbreviations in hematopoietic science can be tricky. By explaining these differences, we hope to make things clearer. This helps researchers and doctors talk better about their work.
Classification of Multipotent Hematopoietic Stem Cells
Multipotent hematopoietic stem cells are divided into different groups. Each group has its own way of developing into various cell types. This division helps us understand their roles in creating blood cells.
Myeloid-Biased HSCs
Myeloid-biased HSCs mainly turn into cells like monocytes, macrophages, and granulocytes. These cells are key for our body’s defense against infections and keeping tissues healthy.
Lymphoid-Biased HSCs
Lymphoid-biased HSCs, by contrast, mostly become T cells and B cells. These cells are important for our body’s ability to fight off infections and diseases. The right balance between these cells is essential for a strong immune system.
Balanced HSC Populations
Some HSCs can develop into both myeloid and lymphoid cells. These balanced cells are vital for our body’s ability to make new blood cells. They help keep our immune system in balance.
Learning about the different types of HSCs can help us understand how blood cells are made. It could also lead to new ways to treat blood-related diseases.
Regulation of the Hematopoietic Stem Cell Lineage
The balance between what’s inside the cell and outside factors is vital for keeping hematopoietic stem cells in check. These cells are in charge of making blood cells for our whole lives. Keeping them regulated is key to healthy blood production.
Intrinsic Regulatory Mechanisms
Things inside the cell, like genes and proteins, help control how HSCs work. These include:
Transcription Factors
Transcription factors are proteins that turn genes on or off. They help HSCs decide whether to grow more or become different types of blood cells.
Epigenetic Regulation
Epigenetic changes, like DNA methylation, also affect HSCs. These changes can turn genes on or off without changing the DNA itself.
Extrinsic Factors and the Bone Marrow Niche
The bone marrow niche is a special area that helps HSCs stay healthy. Signals from this niche and the surrounding tissue guide how HSCs behave.
| Regulatory Mechanism | Key Components | Function |
|---|---|---|
| Intrinsic Regulation | Transcription Factors, Epigenetic Modifications | Control gene expression, influence HSC self-renewal and differentiation |
| Extrinsic Factors | Bone Marrow Niche, Niche Cells, Extracellular Matrix | Provide supportive microenvironment, regulate HSC behavior |
Understanding how both inside and outside factors work together is key. By studying these interactions, we can learn more about how HSCs are kept in balance. This knowledge helps us understand what goes wrong in blood disorders.
Identification and Isolation of HSC Cell Populations
To study HSCs, researchers must first identify and isolate these cells. They use specific markers and assays for this. The identification of hematopoietic stem cells (HSCs) is key to understanding their role in blood cell production. We use a mix of surface marker analysis and functional assays to study their activity and characteristics.
Surface Markers and Phenotypic Identification
HSC identification relies on certain surface markers. These markers, like CD34 and CD38, help distinguish HSCs from other cells. For more on HSC phenotyping panels, check out Stemcell.com.
Functional Assays for HSC Activity
Functional assays are key to understanding HSC activity. These assays fall into in vitro and in vivo tests.
In Vitro Colony-Forming Assays
In vitro colony-forming assays test HSCs’ ability to form blood cell colonies. This shows their multipotency and growth ability.
In Vivo Transplantation Assays
In vivo transplantation assays transplant HSCs into animals. This tests their ability to repopulate the blood system. For more on what stimulates HSCs, see Liv Hospital.
By using surface marker analysis and functional assays, we can accurately identify and isolate HSC populations. This helps us understand their biology and their clinical uses.
Clinical Applications of Hematopoietic Stem Cells
HSCs are being used in many ways, like in hematopoietic stem cell transplantation and gene therapy. This method is key for treating blood-related diseases, such as leukemia and lymphoma.
Hematopoietic Stem Cell Transplantation
This process moves HSCs from a donor or the patient to fix the blood system. It’s a lifesaver for those with blood diseases.
Autologous vs. Allogeneic Transplantation
There are two main types of this transplant: autologous and allogeneic. Autologous uses the patient’s own HSCs. Allogeneic uses HSCs from a donor. The choice depends on the patient’s condition and disease.
Regenerative Medicine Approaches
Regenerative medicine uses HSCs to fix damaged tissues. Researchers are working on therapies that can repair or replace damaged tissues.
Gene Therapy Utilizing HSCs
Gene therapy with HSCs is a promising field. Scientists modify HSCs to treat genetic blood disorders. This could offer long-term treatment for some conditions.
As research grows, HSCs’ uses in medicine will expand. This brings new hope to those with blood diseases.
Recent Advances in Single-Cell Analysis of Hematopoietic Cells
Recent breakthroughs in single-cell analysis have changed how we see hematopoietic cells. We can now dive deep into the details of how blood cells are made. This is thanks to new single-cell RNA sequencing technologies.
Single-Cell RNA Sequencing Technologies
Single-cell RNA sequencing is a key tool for studying individual cells in the blood system. This technology helps find new cell types and states. It shows us the complex ways blood cells are made.
New Insights into HSC Heterogeneity
Single-cell RNA sequencing has shown us how different HSCs really are. This difference is key to understanding how blood cells are made. It shows how different HSCs work together to keep blood cell production going.
Revised Models of Hematopoiesis
New findings from single-cell analysis have led to updated models of blood cell development. These models include the diversity of HSCs and other blood cell makers. They give us a clearer picture of how blood cells are made.
These advances in single-cell analysis are taking us forward in understanding blood cells. They help us see how these cells play a part in health and disease.
Conclusion: Future Directions in Hematopoietic Stem Cell Research
Our journey through hematopoietic stem cells shows how vital research is. It helps us understand HSC biology and its uses. This field keeps growing, seeking new treatments and therapies.
New tools like single-cell analysis and regenerative medicine are changing things. We expect more studies to reveal how HSCs work and their differences. This will help us find better ways to treat diseases.
These breakthroughs will lead to new treatments, like gene therapy and stem cell transplants. To make progress, we must keep studying HSCs. This will open doors to treating many blood-related illnesses.
FAQ
What are hematopoietic stem cells (HSCs) and their role in the body?
Hematopoietic stem cells (HSCs) can grow and change into all blood cell types. They are key to keeping the right balance of blood cells in our bodies.
What is the difference between hematopoietic stem cells (HSCs) and hematopoietic progenitor cells (HPCs)?
HSCs can grow and change into all blood cell types. HPCs can only grow into certain blood cell types.
What is the hematopoietic hierarchy, and how do HSCs differentiate into mature blood cells?
The hematopoietic hierarchy is a complex system. It shows how HSCs turn into mature blood cells through different stages.
What are the different lineages derived from hematopoietic stem cells?
HSCs create two main types of cells. The myeloid lineage makes red blood cells, platelets, and some white blood cells. The lymphoid lineage makes immune cells like T cells and B cells.
What is the significance of the HSC medical abbreviation in clinical terminology?
The HSC medical term stands for hematopoietic stem cells. They are important for treatments like stem cell transplants and regenerative medicine.
How are hematopoietic stem cells regulated, and what factors influence their behavior?
HSCs are controlled by many factors. These include genes, epigenetics, and the bone marrow environment.
What are the clinical applications of hematopoietic stem cells?
HSCs are used in many treatments. These include stem cell transplants, regenerative medicine, and gene therapy.
How have recent advances in single-cell analysis impacted our understanding of hematopoietic cells?
New single-cell RNA sequencing has shown the diversity of HSCs. It has changed our understanding of blood cell development and HSC biology.
What is the significance of myeloid-biased, lymphoid-biased, and balanced HSC populations?
Myeloid-biased, lymphoid-biased, and balanced HSCs show different ways HSCs can develop. This affects blood cell production and immune function.
How are hematopoietic stem cells identified and isolated?
Scientists use specific markers and tests to find and separate HSCs. These include tests done in the lab and in living organisms.
References
- Development (Biologists): https://journals.biologists.com/dev/article/150/14/dev201609/323874/Revisiting-the-lineage-contribution-of
- National Center for Biotechnology Information (NCBI) / PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC5496982/
- Wikipedia: https://en.wikipedia.org/wiki/Hematopoietic_stem_cell
- Frontiers in Cell and Developmental Biology: https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.903528/full