Last Updated on October 28, 2025 by
We are in a new era of cancer treatment, thanks to CAR-T cell therapy. This method has changed how we treat relapsed/refractory B-cell malignancies and multiple myeloma. It brings hope to patients all over the world.
At Liv Hospital, we aim to provide top-notch healthcare. We support patients from around the globe. Our focus is on making the latest CAR-T therapies, technologies, and FDA approvals available to those who need them.
Key Takeaways
- CAR-T cell therapy has shown significant promise in treating various cancers, including relapsed/refractory B-cell malignancies and multiple myeloma.
- The latest advancements in CAR-T technology are expanding its applications in oncology and autoimmune care.
- Liv Hospital is dedicated to providing internationally trusted, patient-focused care, staying abreast of the latest FDA approvals and technological advancements.
- The future of CAR-T cell therapy looks promising, with ongoing research and development aimed at improving its efficacy and accessibility.
- Patients worldwide can benefit from the comprehensive support offered by Liv Hospital, ensuring they receive the best possible care.
The Revolutionary Impact of Immune Cell Therapy in Oncology
CAR-T immunotherapy is changing cancer treatment. It offers new hope for patients and doctors. This method has shown great promise in fighting blood cancers.
Transforming Treatment Paradigms for Blood Cancers
CAR-T cell therapy is a major breakthrough for blood cancer treatments. It uses a patient’s immune cells to fight cancer. This approach has shown high success rates.
In clinical trials, CAR-T therapy has shown impressive results. For example, it has achieved complete remission in 70% to 90% of patients with relapsed or refractory acute lymphoblastic leukemia (ALL).
The 9% Factor: CAR-T’s Role in Addressing U.S. Cancer Burden
Cancer is a big health problem in the U.S., costing nearly 9% of healthcare expenses. CAR-T cell therapy could be a key solution. It offers a chance for cure in some blood cancers.
The impact of CAR-T therapy on U.S. cancer burden is huge. It’s effective against relapsed or refractory blood cancers. As more research and access to this therapy grow, we’ll see less cancer-related illness and death.
| Cancer Type | CAR-T Therapy Efficacy | Remission Rates |
|---|---|---|
| Relapsed/Refractory ALL | High | 70-90% |
| Relapsed/Refractory DLBCL | Moderate to High | 50-70% |
| Relapsed/Refractory Follicular Lymphoma | Emerging | 40-60% |
As CAR-T cell therapy evolves, it will play an even bigger role in fighting U.S. cancer. It brings hope to patients and doctors.
Understanding Chimeric Antigen Receptor T Cells: Mechanism and Manufacturing
Learning about CAR-T cells is key to understanding their benefits. CAR-T cell therapy is a new way to treat some blood cancers. It’s a big step forward in medicine.
The Science Behind CAR-T Cell Engineering
CAR-T cells are made to find and kill cancer cells. First, T cells are taken from a patient’s blood. Then, they are changed to carry a special receptor that targets cancer cells. After that, these cells are put back into the patient.
“The engineering of CAR-T cells is a major breakthrough in immunotherapy,” say experts. It gives hope to those with hard-to-treat cancers.
The CAR has parts that help it find and attach to cancer cells. This makes CAR-T cells very good at fighting tumors.
From Patient to Product: The CAR-T Manufacturing Journey
Making CAR-T cells is a detailed process. It starts with taking T cells from the patient’s blood. These cells are then sent to a lab for genetic changes.
After that, the T cells grow in number. This can take a few days to weeks. The final step is to prepare the cells for the patient’s treatment.
Key steps in CAR-T manufacturing include:
- Leukapheresis to collect T cells
- Genetic modification to introduce the CAR
- Cell expansion to increase the number of CAR-T cells
- Formulation and quality control of the final product
This detailed process needs careful checks to make sure the treatment is safe and works well. As CAR-T cell therapy grows, making the process better will help more people get this treatment.
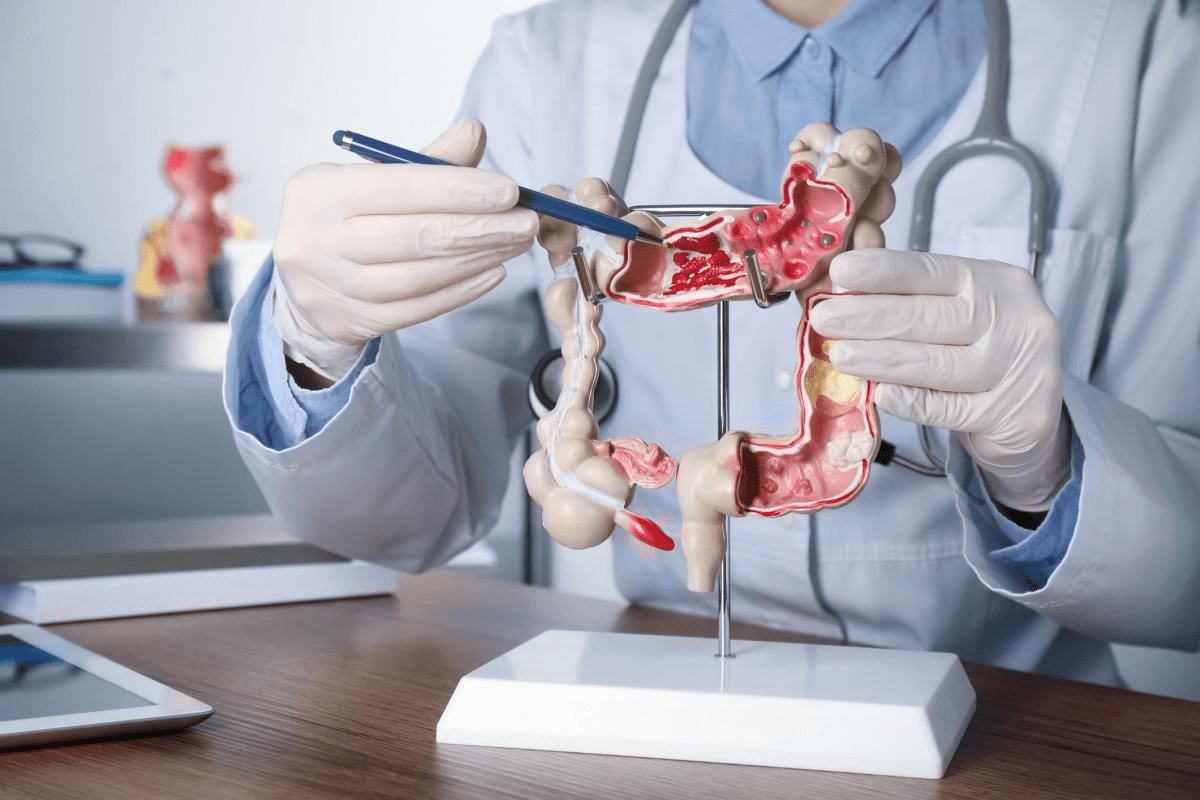
Advancement 1: Expanding CAR-T Therapies Beyond Hematological Malignancies
The field of CAR-T cell therapy is moving towards treating solid tumors. This is a big step in cancer treatment. Understanding the challenges and opportunities in this new area is key.
Breaking the Solid Tumor Barrier
One big challenge in treating solid tumors with CAR-T therapy is the complex tumor environment. Solid tumors have many different types of cells, making it hard for CAR-T cells to find and kill cancer cells.
Researchers are working on new ways to get around this problem. For example, armored CAR-T cells are being made to release substances that help fight tumors. They are also testing combinations of CAR-T therapy with other treatments to make it more effective.
Innovative Approaches to Overcome Tumor Microenvironment Challenges
The tumor environment is a big obstacle for CAR-T cell therapy. It can suppress the immune system and block T cells from getting to the tumor. To solve this, scientists are creating next-generation CAR-T cells that can better fight cancer and get into tumors.
Another approach is to change the tumor environment itself. Using viruses and radiation to make the environment more welcoming for CAR-T cells is being explored. These methods aim to boost the effectiveness of CAR-T therapy in solid tumors.
“The development of CAR-T cell therapy for solid tumors represents a significant advancement in the field of immuno-oncology. By addressing the unique challenges posed by solid tumors, we can unlock the full next-generation CAR-T cells that can better fight cancer and get into tumors.
Another approach is to change the tumor environment itself. Using viruses and radiation to make the environment more welcoming for CAR-T cells is being explored. These methods aim to boost the effectiveness of CAR-T therapy in solid tumors.
“The development of CAR-T cell therapy for solid tumors represents a significant advancement in the field of immuno-oncology. By addressing the unique challenges posed by solid tumors, we can unlock the full next-generation CAR-T cells that can better fight cancer and get into tumors.
Several clinical trials are underway to test CAR-T therapies in solid tumors like glioblastoma, ovarian cancer, and pancreatic cancer. Early results show promise, with some patients seeing a big reduction in tumors.
| Cancer Type | CAR-T Target | Clinical Outcome |
|---|---|---|
| Glioblastoma | EGFRvIII | Partial response in 30% of patients |
| Ovarian Cancer | FRα | Stable disease in 50% of patients |
| Pancreatic Cancer | Mesothelin | Tumor reduction in 25% of patients |
While there are challenges, the progress in CAR-T therapy for solid tumors is encouraging. As research continues, we can expect better outcomes for patients with these hard-to-treat cancers.
Advancement 2: Dual-Targeting Receptors and Multi-Antigen Recognition
CAR-T cell therapy is getting better with new dual-targeting receptors and multi-antigen recognition. This makes CAR-T cells better at finding and attacking cancer cells. It also helps prevent cancer cells from evading treatment, leading to better results.
Combating Antigen Escape with Bi-specific CAR Designs
One big problem with CAR-T cell therapy is when cancer cells hide from the treatment. Bi-specific CAR designs help by letting T cells attack two different antigens at once. This has shown to be more effective in killing cancer cells and reducing the chance of them evading treatment.
Key benefits of bi-specific CAR designs include:
- Enhanced cancer cell targeting
- Reduced risk of antigen escape
- Potential for improved clinical outcomes
Tandem CARs and Logic-Gated Approaches
Tandem CARs and logic-gated CARs are new ways to target cancer cells. Tandem CARs link two CARs to target multiple antigens at once. Logic-gated CARs only work when they find a specific set of antigens, making them more precise and reducing harm to healthy cells.
Creating these complex CAR designs needs advanced engineering and a deep understanding of cancer.
Clinical Evidence for Enhanced Efficacy with Multi-targeting
Early studies show that CAR-T cell therapies targeting multiple antigens work better. Patients treated with these therapies have shown deeper and longer-lasting responses. This is a big step forward in treating cancer.
| Clinical Trial | Target Antigens | Response Rate |
|---|---|---|
| Trial A | CD19, CD20 | 80% |
| Trial B | BCMA, CD38 | 75% |
These results are exciting. They show that targeting multiple antigens could change CAR-T cell therapy for the better. This gives hope to those fighting tough cancers.
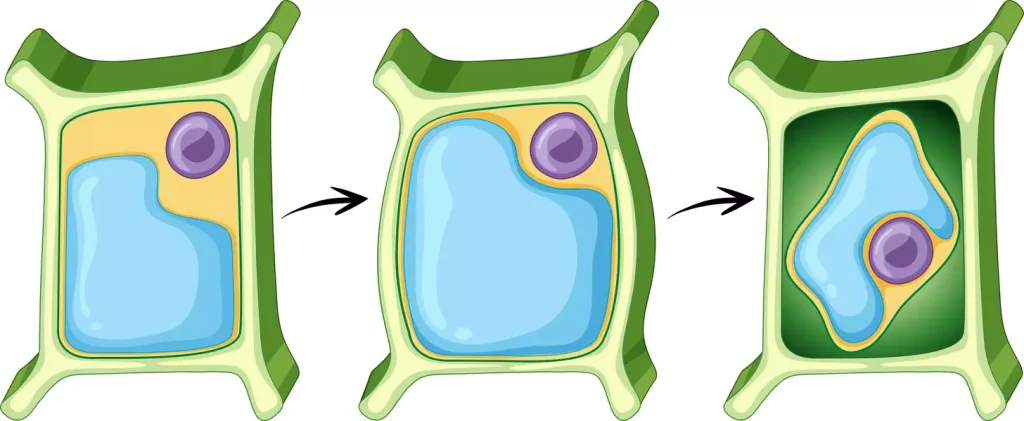
Advancement 3: In Vivo Engineering of CAR T Cell Therapies
In vivo engineering of CAR-T cells is a major leap in cancer treatment. It changes T cells directly in the patient, skipping the need for complex outside lab work.
Direct Patient Modification
This method makes CAR-T cell therapy simpler. It cuts down on the time and cost needed for treatment. It also lowers the chance of T cells getting tired during the making process, making treatments more effective.
Delivery Systems for In-Patient CAR-T Generation
Good delivery systems are key for in vivo CAR-T engineering. Scientists are looking at viral vectors and nanoparticles to get the CAR gene into T cells. They aim to make sure the CAR gene works right in T cells without harming other cells. New tech in nanotechnology is showing great promise in this area.
Potential for Democratizing Access to CAR-T Treatment
In vivo CAR-T cell engineering could make this therapy more available. It could make treatments cheaper and easier to get. This could help more people get the treatment they need, even in places where it’s hard to get.
Dr. Carl June, a leading expert, believes this could change the game. “In vivo CAR-T cell therapy could make this treatment more widely available,” he said. As research keeps going, we’ll see big changes in how we treat cancer.
Advancement 4: RNA Medicines and Nanotechnology in CAR T Cell Technology
RNA medicines and nanotechnology are making CAR T cell therapies better. They help solve problems like making the therapy and dealing with side effects.
mRNA-Based Engineering Approaches
mRNA-based engineering is a new way to improve CAR T cell therapy. It uses mRNA to make CARs on T cells. This might lower the chance of long-term side effects.
Benefits of mRNA-based approaches include:
- Reduced risk of insertional oncogenesis
- Flexibility in CAR design and expression
- Potential for repeated dosing to maintain efficacy
Nanoparticle Delivery Systems for Precise T Cell Modification
Nanoparticles are being studied for precise T cell modification. They can target specific cells and deliver genetic material well.
| Nanoparticle Type | Characteristics | Application in CAR-T |
|---|---|---|
| Lipid Nanoparticles | Biocompatible, efficient delivery | mRNA delivery for CAR expression |
| Polymeric Nanoparticles | Customizable, controlled release | Delivery of CAR-encoding DNA |
Transient CAR Expression: Benefits for Safety and Control
Transient CAR expression is safe and controlled. It lets doctors manage CAR T cell activity. This lowers the risk of serious side effects.
“The ability to control CAR T cell activity through transient expression systems is a significant advancement in making these therapies safer for patients.”
Advancement 5: “Off-the-Shelf” Allogeneic CAR-T Cell Products
Researchers are working on allogeneic CAR-T products. These could change how we fight cancer. The idea of “off-the-shelf” CAR-T therapies is exciting. It could make this treatment easier for patients to get.
Universal Donor Approaches to CAR Immunotherapy
Allogeneic CAR-T cells come from healthy donors, not patients. This means we could have a lot of these cells ready to use. It also means we don’t have to make each treatment from scratch, saving time and money.
Key benefits of universal donor approaches include:
- Reduced manufacturing time
- Increased availability of CAR-T cells
- Potential for treating more patients simultaneously
Gene Editing to Prevent Rejection and GVHD
One big challenge with allogeneic CAR-T therapy is stopping graft-versus-host disease (GVHD). Gene editing, like CRISPR/Cas9, is helping. It changes donor T cells to lower GVHD risk. This makes it safer for patients.
Commercial and Logistical Advantages of Allogeneic Products
Creating “off-the-shelf” allogeneic CAR-T products has many benefits. It makes making these cells faster and cheaper. It also makes it easier to store and send them out.
| Advantages | Description | Impact |
|---|---|---|
| Streamlined Manufacturing | Batch production of CAR-T cells | Reduced production time and costs |
| Cryopreservation | Long-term storage of CAR-T cells | Improved distribution flexibility |
| Universal Applicability | Potential use across multiple patients | Increased treatment accessibility |
As research keeps moving forward, “off-the-shelf” allogeneic CAR-T cell products will be key in fighting cancer.
Advancement 6: Repurposing CAR-T for Autoimmune Conditions
CAR-T therapy is being tested for autoimmune diseases, giving hope to patients. Autoimmune conditions, like lupus, MS, and rheumatoid arthritis, happen when the immune system attacks the body. CAR-T cell therapy, first for cancer, is now being explored for autoimmune diseases.
Targeting Pathogenic B Cells in Autoimmunity
B cells are key in autoimmune diseases. CAR-T therapy aims to remove these harmful B cells. CD19-targeting CAR-T cells are showing great promise, as CD19 is often found on these B cells.
A study in the New England Journal of Medicine showed CD19-targeting CAR-T cells work well in lupus. The treatment greatly improved disease scores, with many patients experiencing long-term remissions.
“The use of CAR-T cell therapy in autoimmune diseases represents a paradigm shift in our approach to treating these complex conditions.”
Early Clinical Results in Lupus, MS, and Rheumatoid Arthritis
Early trials of CAR-T therapy for autoimmune diseases are promising. In lupus, CAR-T treatment has significantly reduced disease activity. Early data also suggest CAR-T can improve symptoms in MS and rheumatoid arthritis.
| Disease | Treatment Target | Clinical Outcome |
|---|---|---|
| Lupus | CD19 | Significant reduction in disease activity |
| Multiple Sclerosis | CD20 | Reduced relapse rates |
| Rheumatoid Arthritis | CD19/CD20 | Improved joint function, reduced inflammation |
Balancing Efficacy and Immune Suppression
CAR-T therapy is promising for autoimmune diseases but poses a challenge. Depleting B cells can make patients more susceptible to infections. Researchers are working on ways to reduce these risks, like using suicide genes.
As research advances, we can expect better and safer CAR-T treatments for autoimmune conditions.
Advancement 7: Enhanced Safety Profiles Through Next-Generation Designs
We’re seeing big changes in CAR-T cell tech, making it safer. New designs aim to reduce serious side effects like cytokine release syndrome (CRS) and neurotoxicity.
Managing Cytokine Release Syndrome
Cytokine release syndrome is a serious side effect of CAR-T therapy. Researchers are working on new ways to handle CRS, including:
- Early detection biomarkers: Finding patients at high risk of severe CRS.
- Prophylactic treatments: Using drugs like corticosteroids to prevent CRS.
- CRS-specific scoring systems: Creating a standard way to measure CRS severity.
Neurotoxicity Prevention and Treatment Strategies
Neurotoxicity is another serious side effect of CAR-T therapy. It can cause confusion, seizures, or even brain swelling. Researchers are looking into:
- Neuroprotective agents: Finding drugs to protect the brain from CAR-T damage.
- Early intervention protocols: Creating quick treatment plans for neurotoxicity symptoms.
- Advanced imaging techniques: Using MRI and other scans to track and understand neurotoxicity.
Suicide Switches and Tunable CAR Systems
Researchers are also working on “suicide switches” and tunable CAR systems. These allow for better control over CAR-T cells after they’re given. They include:
- Chemical inducers of dimerization: Enabling quick removal of CAR-T cells if needed.
- Synthetic Notch receptors: Giving programmable control over CAR-T cell activity.
- RNA-based CAR designs: Allowing for adjustable or temporary CAR expression.
These new designs are a big step towards making CAR-T therapy safer and more effective. They could help more patients and treat different types of tumors.
CAR T Cell FDA Approval Milestones: Regulatory Landscape and Market Access
Recent FDA approvals have opened new doors for CAR-T cell therapies. They offer hope to patients with few treatment options before. Understanding the regulatory milestones is key to their adoption.
Approved CAR-T Products and Their Indications
The FDA has approved several CAR-T cell products for blood cancers. Tisagenlecleucel (Kymriah) and Axicabtagene ciloleucel (Yescarta) are pioneers in this field. Tisagenlecleucel is for B-cell precursor ALL in kids and young adults, and for adults with DLBCL. Axicabtagene ciloleucel is for adults with DLBCL and aggressive B-cell lymphomas.
These therapies are expanding to treat more cancers and even solid tumors. Trials are ongoing to explore their effectiveness.
| CAR-T Product | Indication | Approval Year |
|---|---|---|
| Tisagenlecleucel (Kymriah) | Relapsed/refractory B-cell precursor ALL in pediatric and young adult patients | 2017 |
| Tisagenlecleucel (Kymriah) | Adult patients with relapsed/refractory DLBCL | 2018 |
| Axicabtagene ciloleucel (Yescarta) | Adult patients with relapsed/refractory DLBCL and other aggressive B-cell lymphomas | 2017 |
Fast Track Designations and Breakthrough Therapy Status
The FDA has given Fast Track and Breakthrough Therapy status to CAR-T cell therapies. These designations help speed up their development and review. They are important for therapies that show big improvements over current treatments.
Fast Track is for drugs that treat serious conditions and meet an unmet medical need. Breakthrough Therapy is for drugs that treat serious conditions and show significant improvement over current treatments.
Regulatory Challenges in the Evolving Cell Therapy Landscape
The cell therapy landscape is changing, bringing regulatory challenges. Ensuring CAR-T therapies are safe and effective while speeding up approval is a challenge. Issues like manufacturing consistency, long-term follow-up, and side effects like CRS and neurotoxicity are being closely watched.
There’s a team effort from regulatory bodies, manufacturers, and the medical community to tackle these challenges. They aim to make way for the next generation of CAR-T therapies.
Current Efficacy Statistics: The Promise and Limitations of CAR-T Treatment
Looking at CAR-T cell therapy, we see both promise and complexity. It has shown great results in fighting blood cancers. Remission rates range from 50% to 90% in different studies.
Remission Rates from 50% to 90% in Hematological Cancers
Studies show CAR-T cell treatment works well against blood cancers. 50% to 90% of patients with B-cell lymphomas and leukemias see complete remission. A study in Nature shows its high success rate in these cases.
Durability of Response and Long-term Outcomes
While initial results are good, how long these results last is key. Many patients stay disease-free for 1-2 years after treatment. But, we need more data to understand long-term effects and late relapses.
Economic Barriers and Access Disparities
Despite its success, CAR-T therapy is expensive and hard to get. The high cost and complex process limit access for many. It’s important to make this treatment more available for everyone.
Conclusion: The Future Trajectory of CAR-T Cell Therapy
The field of CAR-T cell therapy is growing fast. New research and discoveries are making treatments better. The seven key advancements in CAR-T cell technology have changed how we treat many cancers.
We see a bright future for CAR-T cell therapy. Innovations in in vivo engineering, RNA medicines, and nanotechnology will make treatments more effective and safe. These changes will also make CAR-T treatments more accessible to everyone.
As CAR-T cell therapy gets better, it will help more people. We expect it to be used for solid tumors and autoimmune diseases too. The possibilities for improving patient care are huge, and we’re excited to see what’s next.
FAQ
What is CAR-T cell therapy?
CAR-T cell therapy is a type of immunotherapy. It removes T cells from a patient’s blood. Then, it modifies them to attack cancer cells. After that, the T cells are put back into the body.
How does CAR-T cell therapy work?
It works by making T cells recognize and attack cancer cells. This is done by adding a chimeric antigen receptor (CAR) to the T cells. This CAR lets the T cells find and destroy cancer cells.
What types of cancer can be treated with CAR-T cell therapy?
It’s approved for some blood cancers like leukemia and lymphoma. Researchers are also looking into treating solid tumors with it.
What are the benefits of CAR-T cell therapy?
It has shown great results in treating certain blood cancers. It can lead to high response rates and improved survival. It might even cure some patients.
What are the possible side effects of CAR-T cell therapy?
Side effects include cytokine release syndrome and neurotoxicity. B cell aplasia is another possible side effect. These can be managed with care and sometimes require hospital stays.
How is CAR-T cell therapy manufactured?
First, T cells are taken from the patient’s blood. Then, they are modified to have a CAR. The cells are grown and expanded before being given back to the patient.
What is the role of gene editing in CAR-T cell therapy?
Gene editing, like CRISPR/Cas9, is used to make T cells better. It improves their function and safety. It also helps prevent graft-versus-host disease in donor cells.
What is the difference between autologous and allogeneic CAR-T cell therapy?
Autologous uses the patient’s own T cells. Allogeneic uses donor T cells. This makes allogeneic a ready product for many patients.
What is the current status of CAR-T cell therapy FDA approvals?
The FDA has approved several CAR-T cell therapies for blood cancers. More are in development.
What are the challenges and limitations of CAR-T cell therapy?
It can have serious side effects. Its success can be limited by cancer changes and tumor diversity. Its high cost and complexity also make it hard to access.
What is the future of CAR-T cell therapy?
The future looks bright with ongoing improvements. Gene editing, CAR design, and manufacturing are areas of focus. These advancements could lead to better treatments and outcomes for patients.