Last Updated on October 21, 2025 by mcelik
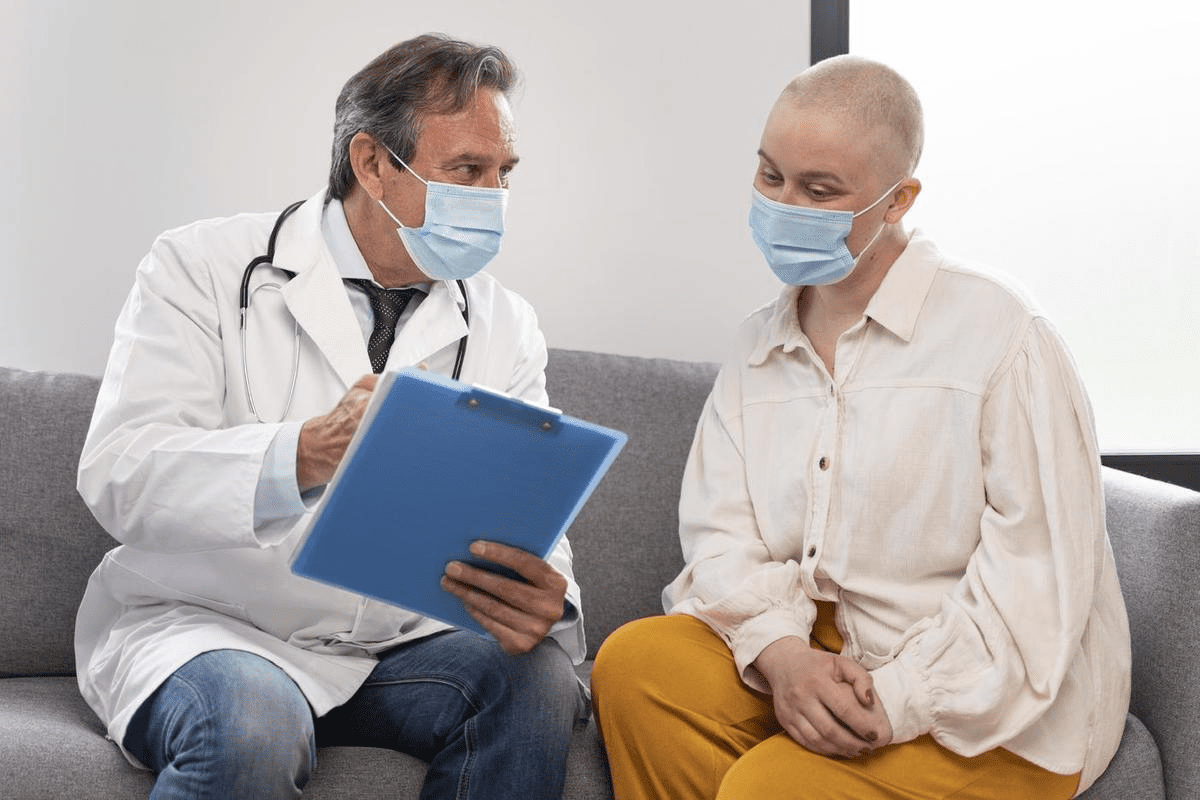
At Liv Hospital, we lead in embryonic stem cell research. We use human embryonic stem cells to change medical science. Our focus on patients and high standards push the limits of stem cell treatments, bringing hope to people everywhere.
Es cells are key to making medicine just for you and fixing damaged tissues. As a top healthcare provider, we aim to grow stem cell research. This way, our patients get the newest and best treatments.
Our exploration of stem cells is based on the latest studies and deep knowledge. We encourage you to learn about the seven important facts about human es cells. They are shaping the future of health care. For more on our stem cell treatments, visit Liv Hospital’s stem cell page.
Key Takeaways
- Embryonic stem cells can become any cell type.
- Stem cell research is key for medical progress.
- Human ES cells are essential for personalized medicine.
- Stem cell therapies offer new ways to treat diseases.
- Liv Hospital is a leader in stem cell research and therapy.
- Stem cells are present at birth and are vital for growth.
- Understanding stem cells shows their value in medical research.
The Science Behind Human ES Cells and Their Discovery
The discovery of human embryonic stem cells (ES cells) was a big step in medical research. These cells, from the inner cell mass of a blastocyst, can grow and change into many cell types. This makes them very useful for studying human growth and for new treatments.
What Defines Embryonic Stem Cells
Embryonic stem cells can grow into all kinds of body cells. They come from the inner cell mass of an early embryo. The way these cells grow is controlled by special proteins and signals. Learning about these controls is key to using ES cells for healing.
These cells can keep growing in a lab as long as they have the right food. Their ability to grow and change makes them great for studying human growth and diseases.
Historical Milestones in ES Cell Research
The journey of ES cell research has seen big steps. In 1981, scientists first got ES cells from mouse embryos. But it wasn’t until 1998 that James Thomson and his team made the first human ES cell lines. This breakthrough opened doors for studying human growth, diseases, and new treatments.
| Year | Milestone | Research Significance |
|---|---|---|
| 1981 | Derivation of ES cells from mouse embryos | Established the foundation for ES cell research |
| 1998 | Derivation of the first human ES cell lines | Enabled research into human development and disease |
| 2006 | Introduction of induced pluripotent stem cells (iPSCs) | Provided an alternative to ES cells for research and therapy |
These key moments show how fast ES cell research has grown. From mice to humans, and beyond. The work keeps going, showing the many ways ES cells can help in medicine.
Fact 1: Pluripotency – The Defining Feature of Embryonic Stem Cells
Embryonic stem cells are special because they can turn into any cell in the body. This is key for their use in fixing damaged tissues and organs.
We’ll dive into the details of pluripotency and why it’s so important in stem cell studies. Knowing how embryonic cells stay pluripotent is vital for their use in medicine.
Understanding What Makes Embryonic Cells Pluripotent
Pluripotency in embryonic stem cells comes from a mix of genes and how those genes are turned on or off. Important genes like Oct4, Sox2, and Nanog keep these cells in a pluripotent state. This lets them grow and change into different cell types.
The control of pluripotency is complex. It involves how cells work on their own and how they respond to their surroundings. Grasping these details is key for using embryonic stem cells to help people.
Differentiation into All Three Germ Layers
Another big plus of embryonic stem cells is their ability to become cells from all three germ layers. This means they can become cells from the ectoderm, mesoderm, and endoderm. This wide range of possibilities is a big plus for fixing damaged tissues and organs.
For example, cells from the ectoderm can become brain cells and skin cells. Cells from the mesoderm can become muscle and blood cells. And cells from the endoderm can become cells from the pancreas and lungs. This ability to make so many different cell types makes embryonic stem cells very useful for research and treatments.
Fact 2: Origin and Derivation of Human ES Cells
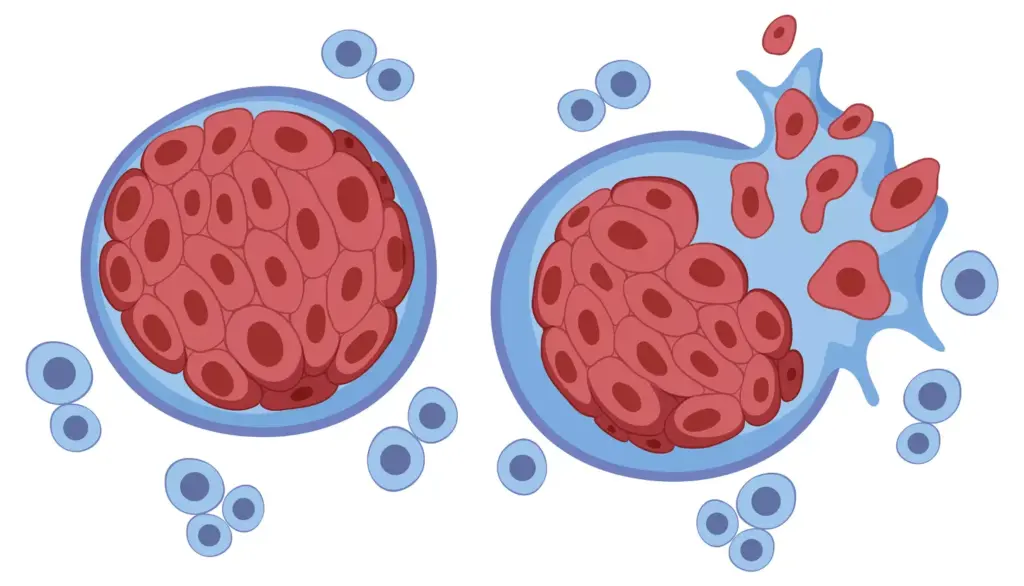
Human ES cells come from a stage in the embryo called the blastocyst. This stage is key because it has the inner cell mass. From this, ES cells are taken.
The Blastocyst as the Source of Embryonic Stem Cells
The blastocyst forms 5-6 days after fertilization. It has two main parts: the trophoblast and the inner cell mass (ICM). The ICM is pluripotent, meaning it can become all three germ layers: ectoderm, endoderm, and mesoderm. This makes the blastocyst perfect for getting human ES cells.
As , a renowned stem cell researcher, once said, “The blastocyst stage is key for getting human ES cells because of its pluripotent nature.”
Isolation of the Inner Cell Mass
Getting the ICM from the blastocyst is a tricky task. It involves taking off the trophoblast layer and growing the ICM in a special medium. This medium helps the ICM grow and stay pluripotent. This step is vital for making human ES cell lines.
“The isolation of the inner cell mass is a technical challenge that requires precision and the right conditions to preserve the cells’ pluripotency.” –
Establishment of Stable ES Cell Lines
After getting the ICM, the next step is to make stable ES cell lines. This means growing the cells in a controlled setting that helps them keep renewing themselves and stay pluripotent. Making stable ES cell lines is a big achievement in stem cell research. It lets scientists study human development and disease modeling.
| Stage | Description | Significance |
|---|---|---|
| Blastocyst Formation | Formation of the blastocyst 5-6 days post-fertilization | Contains the inner cell mass, the source of ES cells |
| ICM Isolation | Removal of the trophoblast and culturing of the ICM | Critical for deriving human ES cells |
| ES Cell Line Establishment | Culturing ICM cells to establish stable ES cell lines | Essential for stem cell research and applications |
In conclusion, getting human ES cells from the blastocyst is a complex but interesting process. Knowing how these cells come from is key for moving forward in stem cell research and its uses.
Fact 3: Self-Renewal Properties of Human ES Cells
Embryonic stem cells can keep renewing themselves forever. This makes them very useful for research and treatments. They can turn into many different cell types because of their ability to self-renew. We will look into how this happens, how they grow, and how scientists keep them in a lab.
Molecular Mechanisms Driving Self-Renewal
The self-renewal of human ES cells involves many molecular steps. Important pathways like Wnt/β-catenin and PI3K/Akt help control this process. These pathways keep the cells’ ability to renew themselves by keeping certain genes active.
Proliferation Characteristics of ESC Stem Cells
ESC stem cells grow quickly in the lab. They can grow a lot because they keep their telomeres long. This helps them stay healthy and stable.
Maintaining Stemness in Laboratory Conditions
To keep ES cells in a lab, scientists need to create the right environment. They use special growth factors and inhibitors. They also use feeder layers or feeder-free systems to help the cells stay in their stem state.
| Factor | Description | Role in Self-Renewal |
|---|---|---|
| Wnt/β-catenin signaling | A key signaling pathway | Regulates pluripotency and self-renewal |
| PI3K/Akt pathway | Supports cell survival and proliferation | Promotes self-renewal by inhibiting differentiation |
| Oct4, Sox2, Nanog | Pluripotency markers | Essential for maintaining ES cell identity |
In conclusion, the self-renewal of human ES cells is complex. It involves many molecular steps and lab conditions. Understanding these is key to using ES cells for medicine and research.
Fact 4: Therapeutic Applications in Regenerative Medicine
Human ES cells have changed the game in regenerative medicine. They offer new ways to treat degenerative diseases. This shift is thanks to their ability to repair damaged tissues.
These cells are used in many ways in regenerative medicine. They can become different types of cells. This makes them great for fixing or replacing damaged tissues.
Cell Replacement Therapies for Degenerative Diseases
Cell replacement therapy uses ES cells to fix damaged cells. This method is promising for diseases like Parkinson’s. It can help by making new dopamine-producing neurons.
- Parkinson’s disease: Replacing dopamine-producing neurons
- Type 1 diabetes: Generating insulin-producing beta cells
- Spinal cord injuries: Repairing damaged neural tissue
These therapies are being tested but offer hope for now untreatable conditions.
Tissue Engineering Using Embryonic Stem Cells
Tissue engineering is another area where ES cells are making a big difference. By mixing ES cells with biomaterials, researchers can make tissue substitutes. These can repair or replace damaged tissues.
Tissue engineering applications include:
- Creating artificial organs for transplantation
- Developing tissue models for drug testing
- Repairing damaged heart tissue after a heart attack
Current Clinical Applications and Future Directions
Some ES cell-based therapies are showing promising results in clinical trials. For example, they’re being looked at for treating macular degeneration.
“The use of human ES cells in regenerative medicine has the power to change how we treat diseases. As research moves forward, we’ll see more ES cell-based therapies in trials.” -Stem Cell Researcher
As research keeps improving, we’ll see more uses of human ES cells in regenerative medicine. This will change healthcare in big ways.
Fact 5: Human ES Cells as Models for Development and Disease
Human ES cells have changed the game in developmental biology. They let us study human development in a lab. This is because these cells can turn into many different types of cells.
Studying Human Embryonic Development In Vitro
Using human ES cells is a big plus. We can model early human development in the lab. This helps us understand how embryos grow and develop.
It also helps us learn about developmental disorders. This is because we can see how different cell types form.
Disease Modeling with HESC Cells
Disease modeling with human ES cells is another big advantage. We can study diseases in a dish. This includes conditions like Parkinson’s disease and diabetes.
By studying these diseases in a lab, we can find new treatments. This is because we can see how diseases progress.
Drug Discovery and Toxicity Testing Applications
Human ES cells are also key in drug discovery and testing. They help us test new drugs in relevant cells. This makes it easier to move from lab to human trials.
They also help us find out if drugs are safe. This is important for making sure drugs are safe for people.
In conclusion, human ES cells are very useful. They help us understand development and disease. They are changing how we find and test new treatments.
Fact 6: Advanced Protocols for Directed Differentiation
Human ES cells can turn into specialized cells using advanced methods. This opens up new ways to treat diseases. It’s a big step forward for regenerative medicine.
Generating Specialized Cell Types from ES Cells
Directed differentiation guides ES cells to become specific cell types. It uses controlled signals to help them grow into different cells. This includes:
- Neurons for treating brain disorders
- Cardiomyocytes for heart disease treatments
- Pancreatic beta cells for diabetes care
These cells can help in many ways. They can replace damaged cells, help in studying diseases, and aid in finding new medicines.
Efficiency Considerations in Differentiation Protocols
The success of differentiation depends on how well the process works. Important factors include:
- The right growth factors and signals
- The culture conditions, like the surface and oxygen levels
- When and how long to apply the differentiation signals
Improving these areas is key to getting high-quality cells. It also helps make sure the results are consistent.
Quality Control in Embryonic Stem Cell Applications
Ensuring the safety and effectiveness of ES cell therapies is vital. Important steps include:
- Checking the cell type and purity
- Measuring cell health and function
- Looking for contaminants or genetic issues
Strict quality control is needed. It ensures ES cell products are safe and effective for use in treatments.
Fact 7: Ethical Considerations in Stem Cell Research on Embryos
The use of human embryos in stem cell research raises many ethical questions. These questions include the moral status of embryos and the rules that guide this research.
The Moral Status Debate
The debate is about when life starts and what rights embryos have. Supporters of using embryos for research say the benefits, like finding cures, are worth it. But, others think embryos are too valuable to use for research.
-Researcher
“The human embryo, though small and unseen, is a human being, and human beings are not mere clumps of cells.”
This debate is not just about philosophy. It’s also about personal and cultural values. It’s about finding a balance between medical progress and respecting human life.
Regulatory Frameworks Across Different Countries
Rules for using embryos in research vary by country. This shows how different cultures, ethics, and politics can be. For example, the UK allows research up to 14 days after fertilization. Germany has stricter rules for historical and ethical reasons.
These rules affect where and how research is done. It’s important for researchers and policymakers to understand these rules.
Alternative Research Approaches and Their Limitations
Because of ethical worries, scientists look for other ways to do research. One option is using induced pluripotent stem cells (iPSCs). These cells are made from adult cells, avoiding the need for embryos. But, making iPSCs can be hard and there’s a risk of genetic problems.
Research is trying to make iPSCs better and safer. But, the debate over the best way to do stem cell research continues.
Cutting-Edge Research and Implementation of Human ES Cell Technologies
The field of human ES cell research is making huge strides. It’s changing how we see human biology and disease. We’re entering a new era in regenerative medicine, where human ES cells are key to new therapies.
Recent Breakthroughs in Embryonic Stem Cell Research
In recent years, embryonic stem cell research has seen big leaps. Scientists have better understood how ES cells grow and change. They’ve also found ways to make specific cell types from ES cells more efficiently.
Some major achievements include:
- Creating induced pluripotent stem cells (iPSCs) from adult cells, a big step for personalized medicine.
- Improvements in gene editing technologies like CRISPR/Cas9, making precise changes to ES cell genes.
- Learning more about epigenetic regulation of ES cells, helping us understand their pluripotency.
Medical Institutions Advancing ES Cell Applications
Many medical institutions are leading the way in ES cell research. Places like the Stanford University School of Medicine and the University of Cambridge are pushing the boundaries of ES cell biology and its uses.
These places are not just studying ES cells. They’re also working on using this knowledge to help patients. They’re teaming up with companies to create new treatments based on human ES cells.
Personalized Medicine Approaches Using Human Embryonic Cells
Using human ES cells in personalized medicine is very promising. By making ES cells from patient-specific iPSCs, researchers can create treatments that fit each person perfectly. This reduces the chance of the body rejecting the treatment.
“The use of human ES cells in personalized medicine has the power to change how we treat diseases. It lets us offer treatments that are made just for each person’s needs.”
We’re seeing a big move towards personalized medicine with human embryonic cells. Researchers are finding new ways to use ES cells to make treatments that are made just for each patient.
Conclusion: The Future Landscape of Human Embryonic Stem Cell Research
Human embryonic stem cell research could change how we do medical research and treatments. ES cells can turn into any cell type, which is great for medical studies and treatments. They can also keep growing and renewing themselves, opening new doors for fixing damaged tissues.
As human embryonic stem cell research keeps getting better, we’ll see big steps forward in treating diseases and injuries. The future looks bright for hESC cells, with more clinical trials on the way. These trials aim to use ES cells for different treatments.
We’re looking forward to learning more about human development and diseases from ES cells. This knowledge will help us find new ways to solve medical problems. But, we must also think about the ethics and rules around using human embryonic stem cells.
FAQ
What are human ES cells, and how are they derived?
Human ES cells, or embryonic stem cells, come from the inner cell mass of a blastocyst. This is an early stage in embryonic development. They can grow and change into different cell types.
What is pluripotency, and why is it significant in ES cells?
Pluripotency means a cell can turn into any cell type from the three germ layers. This makes ES cells very useful for research and possible treatments. They can become any cell in the body.
How are human ES cells used in regenerative medicine?
Human ES cells are being studied for regenerative medicine. They could help replace damaged cells in diseases and help build new tissues. Their ability to change into specific cells is promising.
What are the ethical considerations surrounding ES cell research?
Using human embryos for ES cell research is a big ethical issue. It’s about the moral value of the embryo. Countries have different rules for this research, and debates are ongoing.
How are ES cells used in disease modeling and drug discovery?
ES cells help model human diseases in a lab. This lets researchers study and test treatments. They also help in finding and testing drugs, making them safer and more effective.
What is the significance of self-renewal in ES cells?
Self-renewal is key for ES cells. It lets them grow forever in the lab while keeping their ability to become many cell types. Knowing how this works is important for keeping ES cells alive in the lab.
What are the challenges in directed differentiation of ES cells?
Directed differentiation is hard because it’s about making ES cells into specific cell types. The big challenges are getting the right cell type efficiently and making sure they work well and are safe for use.
Are embryonic stem cells pluripotent?
Yes, embryonic stem cells can become any cell type from the three germ layers. This is what makes them pluripotent.
What is the role of hESC cells in biomedical research?
Human embryonic stem cells (hESCs) are very important in biomedical research. They help us understand human development, model diseases, and find new drugs.
How do regulatory frameworks vary across countries for ES cell research?
Rules for ES cell research differ a lot between countries. This shows the different views on using human embryos for research, based on ethics, culture, and society.
References:
- International Society for Stem Cell Research. (n.d.). Section 2: Pluripotency and the Undifferentiated State. In Standards for Human Stem Cell Use in Research. Retrieved from https://www.isscr.org/standards-document/pluripotency isscr.org
- International Society for Stem Cell Research. (n.d.). Basic Research Standards. Retrieved from https://www.isscr.org/basic-research-standards isscr.org
- ISSCR standards for the use of human stem cells in basic research. Stem Cell Reports, 18(9), 1744–1752. doi:10.1016/j.stemcr.2023.08.003 PMC+1
- University of Wisconsin. (n.d.). UW‑4025: [Title of UW‑4025 Policy]. UW Policy Library. Retrieved from https://policy.wisc.edu/library/UW-4025