Last Updated on October 28, 2025 by
Meta description: Explore eight common muscle and bone pain side effects after a stem cell transplant and how to manage post-transplant recovery effectively.
Recovering from a stem cell transplant is tough, with muscle and bone pain being a big problem. At Liv Hospital, we know how important it is to manage these side effects. This helps make the recovery smoother.
Stem cell transplants can cause many side effects, from mild to severe. But with our advanced care and focus on the patient, we can make symptoms better. This helps keep patients comfortable and safe during their transplant journey.
We know that muscle pain is a big issue for many patients. Our team is ready to help at every step of the recovery. We offer personalized support to make sure patients get the best care.
Key Takeaways
- Muscle and bone pain are common side effects after a stem cell transplant.
- Advanced protocols and patient-centered care can alleviate symptoms.
- A multidisciplinary approach ensures comprehensive support throughout recovery.
- Managing side effects is crucial for a successful recovery.
- Liv Hospital is committed to delivering world-class healthcare with international patient support.
Understanding Stem Cell Transplants and Their Effects on the Musculoskeletal System
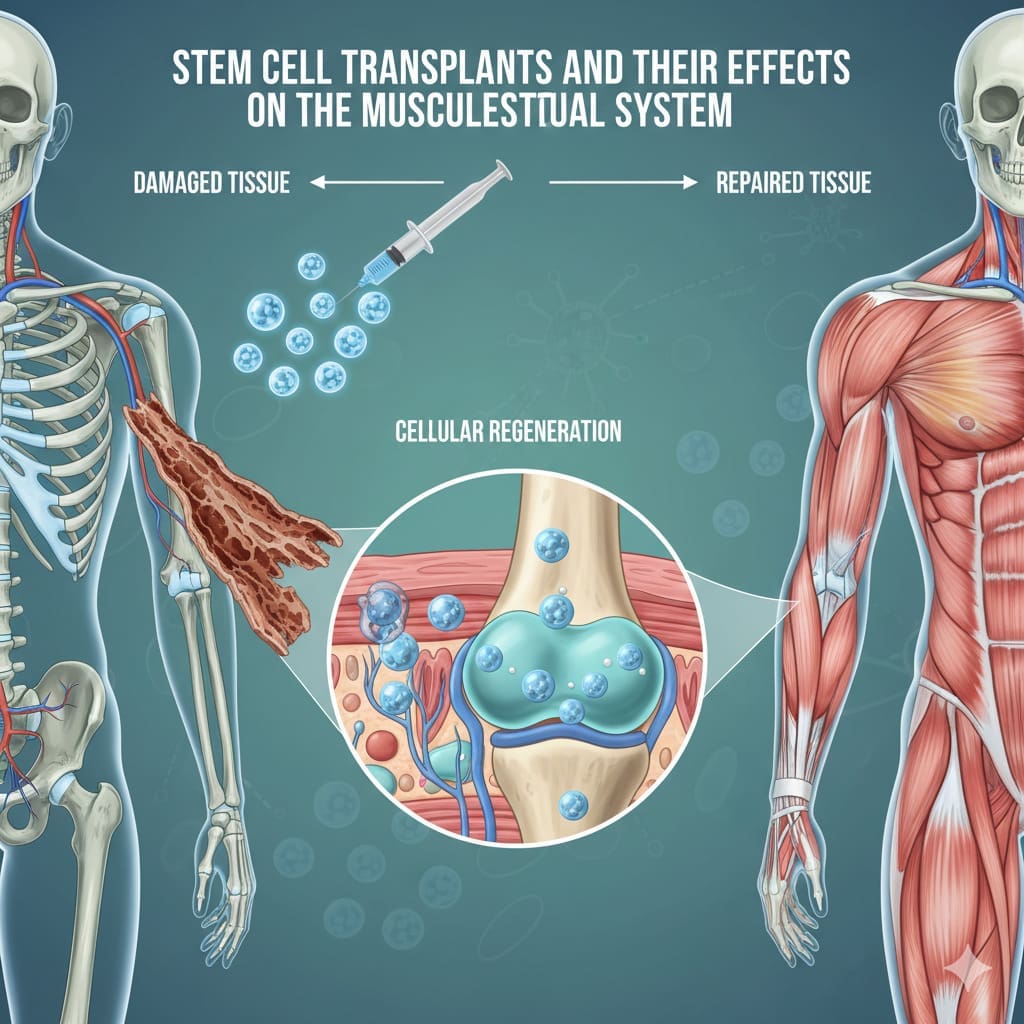
It’s important to know how stem cell transplants affect muscles and bones. These transplants are a complex medical process. They prepare the body for new cells but can cause muscle and bone pain.
What happens during a stem cell transplant
Patients get treatments like chemotherapy and radiation therapy during a transplant. These treatments kill old bone marrow to make room for new cells. But, they can also harm muscles and bones.
Looking into the effects of stem cell transplants, we must also consider graft-versus-host disease. It can make recovery harder.
How conditioning treatments affect muscles and bones
Conditioning treatments in stem cell transplants can harm muscles and bones. Chemotherapy can weaken muscles and cause pain. Radiation therapy can damage bones and lead to osteoporosis.
Some medications used in these treatments can cause muscle cramps and spasms. Also, some patients may face negative effects of stem cell therapy that affect their muscles and bones.
These treatments can also disrupt the musculoskeletal system. This can lead to long-term issues like muscle weakness and bone pain. Knowing these effects helps in managing pain and improving life quality for transplant patients.
Muscle Pain After Stem Cell Transplant: Prevalence and Characteristics
Muscle pain is a common issue after a stem cell transplant. It affects many patients. Knowing how common and what muscle pain is like helps us manage it better. We look at how often it happens and how long it lasts to understand it better.
Survey Data on Frequency of Muscle Pain
More than half of patients who get stem cell transplants experience muscle cramps. These cramps are often very painful. This shows muscle pain is a big problem for these patients.
Studies show muscle pain is not just common. It also causes a lot of distress for patients. The pain can come from different things, like the treatment before the transplant or problems after it.
Typical Onset and Duration of Symptoms
Muscle pain can start early in recovery and last for weeks or months. Knowing when and how long it lasts helps doctors help patients better.
What affects when and how long muscle pain lasts includes the type of transplant and the treatment used. By understanding these, doctors can better manage muscle pain and help patients recover better.
Severe Muscle Cramps and Spasms
Stem cell transplantation can lead to severe muscle cramps and spasms. These symptoms can be very distressing and slow down recovery.
Why Transplant Recipients Experience Painful Cramps
Transplant recipients often get painful cramps for several reasons. Conditioning treatments before the transplant can cause electrolyte imbalances. These imbalances can disrupt muscle function, causing cramps.
Also, some transplant medications can lead to muscle cramping. These drugs can affect electrolyte levels or nerve function, causing cramps.
Common Triggers and Patterns
Several factors can trigger or worsen muscle cramps in transplant recipients. These include:
- Dehydration or inadequate fluid intake
- Electrolyte imbalances, particularly low levels of potassium, calcium, or magnesium
- Certain medications, such as diuretics or those that affect electrolyte levels
- Muscle fatigue or overuse
Knowing these triggers can help manage and reduce muscle cramps.
Differentiating Normal from Concerning Cramps
Some muscle cramping is normal after a transplant. But, we must know when cramps are a sign of a serious issue. It’s important to tell the difference between typical cramps and those that need medical attention.
Concerning cramps are often severe, last a long time, and don’t get better with self-care. They may also be accompanied by muscle weakness, numbness, or tingling.
If cramps are severe, last a long time, or have other concerning symptoms, seek medical help. This is to check for any underlying complications.
Bone Pain and Joint Discomfort
People who have had a stem cell transplant often feel bone pain and joint discomfort. These symptoms can really affect their quality of life. It’s important to know why they happen and how to deal with them.
Medication-induced Bone Pain
Some medicines used in stem cell transplants can cause bone pain. Granulocyte-colony stimulating factor (G-CSF) is one of these medicines. We’ll look into how these drugs lead to pain and what can help lessen it.
G-CSF can cause bone pain because it affects the bone marrow. This pain is usually short-lived but can be quite intense. It’s key to manage this pain to help the patient feel better and recover faster.
Graft-versus-Host Disease Effects on Bones
Graft-versus-host disease (GVHD) is a possible complication after a stem cell transplant. GVHD can harm different parts of the body, including bones and joints. We’ll talk about how GVHD leads to bone pain and joint discomfort.
GVHD can cause inflammation in the joints and bones, leading to pain and discomfort. It’s important to manage this condition well to avoid lasting damage and to ease symptoms.
Distinguishing Bone Pain from Muscle Pain
It’s important to tell bone pain from muscle pain to manage it better. Both can happen after a stem cell transplant, but they have different causes and treatments.
Bone pain feels like a deep, dull ache. Muscle pain is more like a strain or spasm. Knowing the difference helps in finding the right treatment.
| Characteristics | Bone Pain | Muscle Pain |
|---|---|---|
| Description | Deep, dull ache | Strain or spasm |
| Location | Specific bones or joints | Muscle groups |
| Causes | Medication, GVHD | Conditioning regimen, medication |
Understanding the difference between bone and muscle pain helps doctors give better pain relief. This improves the patient’s recovery experience.
Peripheral Neuropathy and Nerve Damage
Nerve damage and peripheral neuropathy can happen after a stem cell transplant. Peripheral neuropathy is when nerves are damaged or diseased. This can affect how you feel sensations, move, or even function in other ways.
Chemotherapy-Related Nerve Pain
Chemotherapy can lead to nerve damage and peripheral neuropathy. Some chemotherapy drugs can harm nerves. This can cause pain, numbness, and tingling in your hands and feet.
Chemotherapy-induced peripheral neuropathy can be mild or severe. Sometimes, it goes away after treatment stops. But, in other cases, it can last and need ongoing care.
Symptoms of Transplant-Related Neuropathy
The symptoms of peripheral neuropathy from stem cell transplants vary. Common signs include:
- Numbness or tingling in your hands and feet
- Pain that feels sharp, burning, or stabbing
- Muscle weakness
- Sensitivity to touch
These symptoms can really affect your life. It’s important to find ways to manage them.
Long-Term Nerve Damage Concerns
Long-term nerve damage is a worry for those who have had a stem cell transplant. Risks include the type of treatment, graft-versus-host disease, and past exposure to harmful therapies. We stress the need for ongoing care to watch for and treat neuropathy symptoms.
Early detection and treatment can greatly help patients with peripheral neuropathy. This means checking for symptoms and using the right pain management plans.
Persistent Muscle Weakness and Fatigue
Recovering from a stem cell transplant can be tough due to persistent muscle weakness and fatigue. These symptoms can really impact a patient’s life and recovery. They are common but can make things hard.
Causes of Post-Transplant Weakness
Many things can cause muscle weakness after a stem cell transplant. The treatments before the transplant, like chemotherapy and radiation, can harm muscle cells. Also, some medicines after the transplant can make muscles weak.
Graft-versus-host disease (GVHD) can also cause muscle weakness. It can harm many tissues and organs. Plus, not moving much during recovery can make muscles weak and smaller.
Impact on Mobility and Daily Activities
Muscle weakness can make it hard to move around and do daily tasks. Even simple things like walking or getting dressed can be tough. This can hurt both your body and mind, leading to feelings of frustration or sadness.
Getting stronger is key for both your body and mind. Doctors often suggest physical therapy and special programs to help. These are designed to improve muscle strength and mobility.
Timeline for Strength Recovery
How long it takes to get stronger varies from person to person. It depends on your health before the transplant, the treatment’s intensity, and if you have GVHD.
Most people start to feel stronger a few months after the transplant. But, it can take longer to fully recover. It’s important to keep in touch with your healthcare team. They can help adjust your recovery plan as needed.
Gastrointestinal Complications Contributing to Muscle Pain
Patients after a stem cell transplant often face muscle pain due to gastrointestinal issues. These problems can come from the treatment, medicines, and the transplant itself. It’s important to understand how these issues affect muscle pain to find better ways to manage it.
Nutritional Deficiencies Affecting Muscle Health
Nutritional problems are a big issue for muscle health after a transplant. Gastrointestinal issues make it hard for the body to take in important nutrients. This can cause a lack of vitamins and minerals needed for muscle recovery.
- Protein deficiency: Impairs muscle repair and regeneration.
- Vitamin D deficiency: Affects muscle strength and function.
- Magnesium and potassium deficiencies: Contribute to muscle cramps and spasms.
Fixing these nutritional gaps with food changes or supplements is key to keeping muscles healthy and easing pain.
Medication Side Effects on the Digestive System
Medicines after a transplant, like immunosuppressants and antibiotics, can harm the digestive system. These effects can cause nausea, vomiting, diarrhea, and stomach pain.
Nausea and vomiting can lead to dehydration and imbalances in electrolytes, making muscle cramps and pain worse. Diarrhea can also cause the body to miss out on nutrients, adding to nutritional deficiencies.
Managing Stomach Problems to Reduce Pain
It’s crucial to manage gastrointestinal issues to lessen muscle pain. This requires a few steps:
- Dietary modifications: Changing diet to ease stomach stress.
- Medication management: Changing or switching medicines to lessen side effects.
- Nutritional supplements: Using supplements to fix specific nutrient gaps.
- Supportive care: Taking steps to handle symptoms like nausea and diarrhea.
By tackling gastrointestinal problems, healthcare teams can help reduce muscle pain and improve life quality for those who have had a stem cell transplant.
Infection-Related Pain and Inflammation
Patients after a transplant face a higher risk of infections. These infections can cause pain in muscles and bones. It’s important to watch for signs of infections to help with recovery.
Heightened Infection Risk Post-Transplant
After a stem cell transplant, the immune system is weakened. This makes patients more likely to get infections. Knowing the signs of infections is key to getting help quickly.
The risk factors for infections post-transplant include:
- Immunosuppression due to conditioning regimens and GVHD prophylaxis
- Catheter-related infections
- Viral reactivations, such as CMV and herpes zoster
- Bacterial and fungal infections
How Infections Manifest as Muscle and Bone Pain
Infections can cause muscle and bone pain in different ways. Viral infections can directly harm muscle tissues, causing pain. Bacterial infections can lead to sepsis, damaging muscles and causing pain.
Some common infections that can lead to muscle and bone pain include:
| Infection Type | Symptoms | Muscle and Bone Pain Characteristics |
|---|---|---|
| Viral infections (e.g., influenza) | Fevers, chills, cough | Generalized muscle pain, myalgias |
| Bacterial infections (e.g., sepsis) | High fever, chills, confusion | Muscle weakness, pain upon movement |
| Fungal infections | Variable, depending on the site | Localized pain, potentially severe |
Warning Signs Requiring Immediate Medical Attention
It’s important for patients to know the signs of infections that need immediate help. These include:
- High fever (over 38 °C or 100.4 °F)
- Severe chills or sweating
- Confusion or altered mental status
- Severe pain or swelling
- Shortness of breath or difficulty breathing
If you notice any of these symptoms, seek medical help right away. Quick treatment can greatly improve your chances of recovery.
Effective Pain Management and Rehabilitation Strategies
Effective pain management is key after a transplant. It helps patients recover better. We use a mix of medical treatments, physical therapy, and teach patients when to ask for more help.
Medical Interventions for Pain Relief
There are many ways to ease pain after a stem cell transplant. Medications like painkillers and anti-inflammatory drugs are often used. Some patients might try nerve blocks or acupuncture too.
Choosing the right treatment depends on the pain’s type and how severe it is. Our team works with patients to create a pain plan that fits them.
Physical Therapy Approaches
Physical therapy is important for recovery after a stem cell transplant. Gentle exercises and stretches help move better and ease muscle pain. We suggest physical therapy programs that match each patient’s needs.
These programs might include massage, heat therapy, and exercises to help heal and reduce pain.
When to Seek Additional Medical Help
It’s important for patients to know when to get more medical help. Severe or getting worse pain, trouble moving, or pain with fever or swelling means you need to see a doctor right away.
We teach our patients about these signs. We tell them to contact their doctor if they notice anything unusual.
Conclusion: Navigating Recovery and Long-Term Outlook
Recovering from a stem cell transplant needs a full plan to handle muscle and bone pain. We’ve looked at the side effects, like muscle pain, severe cramps, bone pain, and nerve damage.
It’s key to manage pain well, using medicine and physical therapy. Knowing what causes these symptoms helps patients get through recovery better.
We at our institution aim to give top-notch care and support to our patients. We believe the right help and care can help patients beat the side effects of stem cell transplants. This way, they can have a good long-term outcome.
FAQ
What are the common muscle and bone pain side effects after a stem cell transplant?
Muscle and bone pain are common after a stem cell transplant. They affect many patients. These pains can come from treatments, graft-versus-host disease, and medication side effects.
How can I manage muscle pain after a stem cell transplant?
To manage muscle pain, you need to understand the pain’s causes and how to handle it. This includes medical treatments, physical therapy, and changes in your lifestyle.
What are the causes of severe muscle cramps and spasms after a stem cell transplant?
Severe muscle cramps and spasms can happen for many reasons. These include imbalances in electrolytes, side effects from medication, and nerve damage. Knowing the cause helps in finding the right treatment.
How can I differentiate between normal and concerning muscle cramps after a stem cell transplant?
To tell if muscle cramps are normal or not, look at how often, how bad, and how long they last. Also, watch for other symptoms like muscle weakness or numbness.
What is the role of graft-versus-host disease in bone pain after a stem cell transplant?
Graft-versus-host disease (GVHD) can cause bone pain by inflaming and damaging muscles and bones. It can also lead to pain from medication and other issues.
How can I manage bone pain and joint discomfort after a stem cell transplant?
Managing bone pain and joint discomfort needs a full plan. This includes knowing the cause and finding ways to manage pain. This can include medical treatments, physical therapy, and lifestyle changes.
What are the symptoms of peripheral neuropathy after a stem cell transplant?
Peripheral neuropathy can cause numbness, tingling, burning pain, and muscle weakness. These symptoms can come from nerve damage from chemotherapy and other factors.
How can I manage persistent muscle weakness and fatigue after a stem cell transplant?
To manage muscle weakness and fatigue, you need a detailed plan. This includes understanding the cause and finding ways to improve strength and reduce fatigue. This can include physical therapy, lifestyle changes, and medical treatments.
What is the impact of gastrointestinal complications on muscle pain after a stem cell transplant?
Gastrointestinal issues, like nutritional deficiencies and side effects from medication, can cause muscle pain. Managing these issues is key to reducing pain and improving health.
How can I identify warning signs of infection-related pain after a stem cell transplant?
Look for signs of infection like fever, chills, and increased pain or swelling. If you notice these, get medical help right away.
What are the effective pain management strategies after a stem cell transplant?
Effective pain management includes medical treatments, physical therapy, and lifestyle changes. A full plan that understands the pain’s cause and how to manage it is essential for easing muscle and bone pain.
References
Anthony Nolan: Physical Side Effects During Recovery
PubMed Central (NCBI): Infection Risk After Allogeneic Stem Cell Transplant
ASH Publications (Blood): Post-Transplant Pain and Paralysis: Neurologic Complications
FAQ
What are the common muscle and bone pain side effects after a stem cell transplant?
Muscle and bone pain are common after a stem cell transplant. They affect many patients. These pains can come from treatments, graft-versus-host disease, and medication side effects.
How can I manage muscle pain after a stem cell transplant?
To manage muscle pain, you need to understand the pain’s causes and how to handle it. This includes medical treatments, physical therapy, and changes in your lifestyle.
What are the causes of severe muscle cramps and spasms after a stem cell transplant?
Severe muscle cramps and spasms can happen for many reasons. These include imbalances in electrolytes, side effects from medication, and nerve damage. Knowing the cause helps in finding the right treatment.
How can I differentiate between normal and concerning muscle cramps after a stem cell transplant?
To tell if muscle cramps are normal or not, look at how often, how bad, and how long they last. Also, watch for other symptoms like muscle weakness or numbness.
What is the role of graft-versus-host disease in bone pain after a stem cell transplant?
Graft-versus-host disease (GVHD) can cause bone pain by inflaming and damaging muscles and bones. It can also lead to pain from medication and other issues.
How can I manage bone pain and joint discomfort after a stem cell transplant?
Managing bone pain and joint discomfort needs a full plan. This includes knowing the cause and finding ways to manage pain. This can include medical treatments, physical therapy, and lifestyle changes.
What are the symptoms of peripheral neuropathy after a stem cell transplant?
Peripheral neuropathy can cause numbness, tingling, burning pain, and muscle weakness. These symptoms can come from nerve damage from chemotherapy and other factors.
How can I manage persistent muscle weakness and fatigue after a stem cell transplant?
To manage muscle weakness and fatigue, you need a detailed plan. This includes understanding the cause and finding ways to improve strength and reduce fatigue. This can include physical therapy, lifestyle changes, and medical treatments.
What is the impact of gastrointestinal complications on muscle pain after a stem cell transplant?
Gastrointestinal issues, like nutritional deficiencies and side effects from medication, can cause muscle pain. Managing these issues is key to reducing pain and improving health.
How can I identify warning signs of infection-related pain after a stem cell transplant?
Look for signs of infection like fever, chills, and increased pain or swelling. If you notice these, get medical help right away.
What are the effective pain management strategies after a stem cell transplant?
Effective pain management includes medical treatments, physical therapy, and lifestyle changes. A full plan that understands the pain’s cause and how to manage it is essential for easing muscle and bone pain.