Last Updated on November 27, 2025 by Bilal Hasdemir
Aortic stenosis is a serious condition where the aortic valve gets narrower. At Liv Hospital, we know how important it is to catch this early. This way, we can start treatment right away.
When the aorta narrows, it blocks blood flow from the heart. This can lead to serious problems if not treated. Our team works hard to give top-notch care. We use the latest methods to help patients from all over.
It’s key to know the symptoms and causes of aortic stenosis. We’ll look at the seven main signs of aorta narrowing. These signs tell us a lot about your heart’s health.
Key Takeaways
- Early detection of aortic stenosis is key for good management.
- Aortic stenosis can block blood flow, leading to serious issues.
- Liv Hospital offers patient-focused care and new ways to help.
- Spotting aorta narrowing signs can save lives.
- Quick medical action is vital for treating aortic stenosis.
Understanding Aortic Stenosis: A Progressive Cardiac Condition
The aortic valve is key to heart function. Its narrowing can cause serious health problems. Aortic stenosis happens when the aortic valve gets narrower, blocking blood flow from the heart.
Definition and Function of the Aorta
The aorta is the main artery from the heart. It carries oxygen-rich blood to the body. It starts in the left ventricle and goes up and down through the chest and belly, splitting into smaller arteries.
The aortic valve is vital. It lets blood flow from the left ventricle into the aorta and stops it from flowing back. The valve has three leaflets that open and close with each heartbeat.
How Narrowing Obstructs Blood Flow
In aortic stenosis, the aortic valve narrows. Its leaflets become stiff or stuck together, making it hard for blood to flow. This forces the heart to work harder to push blood through.
As a result, the heart muscle thickens, and the heart’s pumping ability drops. This can cause symptoms like chest pain, shortness of breath, and tiredness. These are signs of aortic narrowing.
“Aortic stenosis is a serious condition that requires prompt medical attention to prevent complications such as heart failure.”
Knowing about the aorta and how narrowing affects blood flow is key. It helps spot the warning signs of aortic stenosis and get the right medical help.
The Anatomy of a Narrowed Aorta
The aorta’s anatomy is key to understanding its narrowing. It’s the main artery that carries blood from the heart to the body. Its structure and function are vital for blood circulation.
Normal Aortic Valve Structure
The normal aortic valve has three cusps that open to let blood flow. These cusps are thin and flexible, ensuring they open and close right with each heartbeat. The aortic valve’s normal function is essential for efficient blood flow.
Pathological Changes During Stenosis
During stenosis, the aortic valve cusps narrow, blocking blood flow. This can happen due to calcium buildup, congenital issues, or rheumatic fever. As the valve narrows, the heart must work harder to pump blood.
The changes in stenosis can cause chest pain (angina), shortness of breath (dyspnea), and fatigue. These symptoms happen because the heart doesn’t get enough oxygen and nutrients due to less blood flow.
Thickening Process of the Aortic Valve
The thickening of the aortic valve is a key sign of stenosis. As it thickens, the valve can’t open properly, narrowing the valve opening. This thickening can be due to age, congenital conditions, or other diseases.
- The valve leaflets become stiff and less flexible.
- Calcium deposits form on the valve, further restricting its movement.
- The valve orifice narrows, obstructing blood flow.
Understanding these changes is vital for diagnosing and managing aortic stenosis. We will look at diagnostic methods and treatment options next.
Primary Causes of Aortic Narrowing
The aorta’s narrowing is a serious issue. It can happen due to aging or birth defects. Knowing why it happens helps doctors treat it better.
Age-Related Calcium Buildup on Valve Leaflets
Calcium buildup on the aortic valve is a big reason for narrowing. This happens as people get older. It’s more common in seniors and can really affect their life.
Calcium on the valve can make it hard for blood to flow. This is because the valve can’t open as well as it should.
Congenital Bicuspid Valve Abnormalities
Born with a bicuspid aortic valve is another reason for narrowing. This means the valve has only two cusps, not the usual three. It can cause problems with the valve over time.
People with a bicuspid valve are more likely to get aortic stenosis early. This is compared to those with a normal tricuspid valve.
Rheumatic Fever Complications
Rheumatic fever is an inflammatory disease. It can happen after a Streptococcus pyogenes infection. It can cause scarring and narrowing of the aortic valve, leading to stenosis.
Even though rheumatic fever is less common now, it’s a big problem in some places. It can cause a lot of aortic valve disease.
To sum up, here are the main reasons for aortic narrowing:
| Cause | Description | Demographic Most Affected |
|---|---|---|
| Age-Related Calcium Buildup | Calcium deposits on valve leaflets | Older Adults |
| Congenital Bicuspid Valve | Abnormal valve with two cusps | Individuals with Congenital Condition |
| Rheumatic Fever | Inflammatory disease causing valve scarring | Populations with High Incidence of Rheumatic Fever |
Risk Factors for Developing Aortic Stenosis
Knowing the risk factors for aortic stenosis is key for early detection and treatment. Several factors can increase the chance of getting this condition. This can greatly affect a person’s quality of life.
Age and Gender Considerations
Getting older is a big risk for aortic stenosis. The risk grows, mainly after 65. Also, men are more likely to get it than women, showing a gender link.
Key demographic risk factors include:
- Age over 65
- Male gender
Genetic Predispositions
Genetics also matter in aortic stenosis. People with a family history of heart issues or a bicuspid aortic valve are at higher risk. This means certain genes can make you more likely to get it.
Cardiovascular Disease History
Having heart disease in the past is another big risk. High blood pressure, coronary artery disease, and past heart valve problems can lead to aortic stenosis.
Notable cardiovascular risk factors include:
- Hypertension
- Coronary artery disease
- Previous heart valve issues
Lifestyle and Environmental Factors
Smoking, high cholesterol, and not being active can also raise your risk. Staying healthy can help lower some of these risks.
Healthcare providers can spot high-risk individuals by knowing these factors. Early action and care are vital for better outcomes in aortic stenosis patients.
Narrowing of Aorta Symptoms: The 7 Critical Warning Signs
Aortic narrowing shows through several warning signs that need quick action. As the aorta gets more stenotic, patients may feel symptoms that mean they need to see a doctor.
Chest Pain (Angina) During Activity
Chest pain, or angina, is a key symptom of aortic stenosis. It happens when you’re active. This pain is because your heart has to work harder to push blood through the narrowed valve.
Shortness of Breath (Dyspnea)
Shortness of breath, or dyspnea, is another symptom of aortic stenosis. It’s more common when you’re active or lying down. This happens because your heart has to work harder to pump blood, putting more pressure on your lungs.
Persistent Fatigue and Weakness
Fatigue and weakness are common in aortic stenosis patients. The heart has to work harder because of the narrowed aorta. This makes patients feel tired and weak.
Dizziness and Lightheadedness
Dizziness or lightheadedness can happen because of less blood to the brain. This is a serious sign because it means your heart might not be pumping enough.
Other warning signs include:
- Fainting or near-fainting episodes
- Palpitations or irregular heartbeats
- Swollen ankles and feet due to fluid buildup
It’s important to know these 7 warning signs for aortic stenosis. If you or someone you know has these symptoms, get medical help right away.
The Connection Between Symptoms and Underlying Pathology
Understanding the link between aortic stenosis symptoms and its cause is key. Symptoms like reduced blood flow and heart strain are direct results. This knowledge helps in managing the condition effectively.
How Reduced Blood Flow Causes Chest Pain
Chest pain, or angina, is a common symptom of aortic stenosis. It happens when the heart muscle doesn’t get enough oxygen-rich blood. This is usually during physical activity or stress.
The narrowed aortic valve restricts blood flow. This leads to an imbalance between the heart’s oxygen demand and supply. We feel this as chest pain, which can spread to the arms, back, or jaw.
The mechanism behind angina in aortic stenosis involves the increased pressure gradient across the narrowed valve. As the heart pumps harder to overcome this obstruction, it requires more oxygen. But the reduced blood flow limits the oxygen supply, resulting in chest pain.
Cardiac Strain and Breathing Difficulties
As aortic stenosis progresses, the heart works harder to pump blood through the narrowed valve. This leads to cardiac strain. The heart becomes less efficient, causing breathing difficulties or dyspnea.
Patients may experience shortness of breath during exertion or even at rest in advanced cases. The underlying cause of dyspnea in aortic stenosis is multifactorial. It involves the increased pressure in the left ventricle, leading to pulmonary congestion, and potentially, heart failure.
Circulatory Insufficiency and Fatigue
Fatigue is another prevalent symptom in patients with aortic stenosis. The reduced blood flow and cardiac output lead to inadequate perfusion of peripheral tissues and organs. As a result, patients often report feeling weak and tired, even after resting.
The circulatory insufficiency associated with aortic stenosis affects the body’s ability to deliver oxygen and nutrients to tissues. This inefficiency can impair physical performance and contribute to the overall feeling of fatigue.
Cerebral Perfusion Issues and Dizziness
Dizziness or lightheadedness can occur in patients with severe aortic stenosis due to reduced cerebral perfusion. The narrowed valve limits the heart’s ability to increase cardiac output during exertion, potentially leading to a decrease in blood pressure and cerebral blood flow.
When standing up quickly or exerting oneself, patients may experience dizziness or even syncope (fainting). This symptom is concerning as it indicates a significant reduction in cardiac output and may signal advanced disease.
Classification and Progression of Aortic Valve Stenosis
It’s important to know how aortic stenosis is classified. This helps in managing the condition effectively. The severity of aortic stenosis is key, as it affects symptoms.
Mild Stenosis: Subtle Signs
In the early stages, aortic stenosis is mild. At this point, symptoms are not obvious. But, as it gets worse, slight signs may appear. These include shortness of breath when doing hard activities.
Moderate Stenosis: Emerging Symptoms
When aortic stenosis becomes moderate, symptoms get clearer. People might feel increased fatigue, dizziness, and shortness of breath even when doing light activities.
Severe Stenosis: Critical Manifestations
Severe aortic stenosis shows more serious symptoms. These include chest pain (angina), severe shortness of breath, and fainting. These signs mean urgent medical help is needed.
The Progressive Nature of Valve Thickening
Aortic valve stenosis gets worse over time if not treated. The valve’s leaflets thicken and calcify, blocking blood flow more.
But, with the right medical care, its progression can be managed. We’ll look at treatment options next.
- Aortic stenosis is classified as mild, moderate, or severe.
- The severity of the condition correlates with the presence and intensity of symptoms.
- Understanding the classification is key for effective management.
Diagnostic Approaches for Aortic Narrowing
Healthcare professionals use a mix of physical checks, imaging, and lab tests to find aortic narrowing. This detailed method helps us see how serious the narrowing is. It also helps us choose the best treatment.
Physical Examination Findings
A detailed physical check is key in spotting aortic stenosis. We look for signs like a heart murmur, which sounds like a whoosh at the right second space. Other signs include a weak pulse and a delayed heartbeat.
Key Physical Examination Findings:
- Heart murmur
- Pulsus parvus et tardus
- Low blood pressure
- Elevated jugular venous pressure
Imaging Techniques
Imaging is very important in finding and checking how bad aortic stenosis is. We use echocardiography, cardiac MRI, and CT scans for this.
Imaging Modalities:
| Imaging Technique | Description | Benefits |
|---|---|---|
| Echocardiography | Uses sound waves to create images of the heart | Assesses valve function and stenosis severity |
| Cardiac MRI | Provides detailed images of the heart structure | Evaluates cardiac function and anatomy |
| CT Scans | Uses X-rays to create detailed cross-sectional images | Assesses valve calcification and coronary anatomy |
Laboratory Tests and Biomarkers
Lab tests and biomarkers help us see how well the patient is doing and how bad the stenosis is. We use ECGs and blood tests to check the heart’s function and if there’s damage.
Laboratory Tests:
- Electrocardiogram (ECG)
- Blood biomarkers (e.g., troponin, BNP)
- Lipid profiles
By using all these methods together, we can accurately find and treat aortic narrowing. This helps improve patient results.
Complications of Untreated Aortic Stenosis
Untreated aortic stenosis can cause severe and life-threatening problems. This section explores how not treating this condition can harm a patient’s health and well-being.
Heart Failure Development
Untreated aortic stenosis can lead to heart failure. The heart works harder to pump blood through a narrowed valve. This can weaken the heart muscle, causing heart failure. Symptoms include shortness of breath, fatigue, and swelling in the legs and feet.
Heart failure is a serious condition that needs immediate medical attention. If you have symptoms, seek help right away.
Arrhythmias and Electrical Disturbances
Untreated aortic stenosis can cause arrhythmias and heart electrical problems. As the condition worsens, it can disrupt the heart’s electrical activity. This can lead to irregular heartbeats, such as atrial fibrillation and ventricular tachycardia. These problems can worsen heart function and increase the risk of sudden death.
Studies show the importance of watching for arrhythmias in aortic stenosis patients. Early detection and treatment can greatly improve outcomes.
Recent Research on Mortality Rates
Recent studies highlight the high mortality risk of untreated severe aortic stenosis. Within 2-5 years after symptoms start, patients face a high risk of death. A study found that the 5-year survival rate for patients with symptomatic aortic stenosis who didn’t get valve replacement was much lower than those who did.
These findings stress the need for quick diagnosis and treatment of aortic stenosis. Patients with symptoms should seek medical help quickly to discuss treatment options.
In conclusion, untreated aortic stenosis can lead to severe and life-threatening complications. Understanding these risks helps patients and healthcare providers create effective treatment plans to improve outcomes.
- Heart failure development
- Arrhythmias and electrical disturbances
- Increased mortality risk
By addressing aortic stenosis promptly and effectively, we can reduce these risks and improve patients’ quality of life.
Treatment Options for Aortic Narrowing
The treatment for a narrowed aorta varies based on how severe it is and the patient’s health. We’ll look at different treatments, from simple management to more complex procedures.
Medical Management Approaches
For mild aortic stenosis, doctors might start with medical management. This means watching the condition closely and managing symptoms with lifestyle changes and medicine. Regular check-ups are key to tracking the disease’s progress.
Doctors might prescribe medicine to help with symptoms like high blood pressure or heart failure. But, it’s important to know that medicine alone can’t stop the disease from getting worse. Studies, like those on advanced diagnostic techniques, show that accurate diagnosis is vital for the best treatment.
Surgical Valve Replacement
Surgical aortic valve replacement (SAVR) is often a top choice for many patients. This surgery replaces the old valve with a new one, either mechanical or bioprosthetic. SAVR is successful and recommended for younger patients or those with severe symptoms.
Choosing between a mechanical and bioprosthetic valve depends on several factors. Mechanical valves last longer but need lifelong blood thinners. Bioprosthetic valves don’t need blood thinners but don’t last as long.
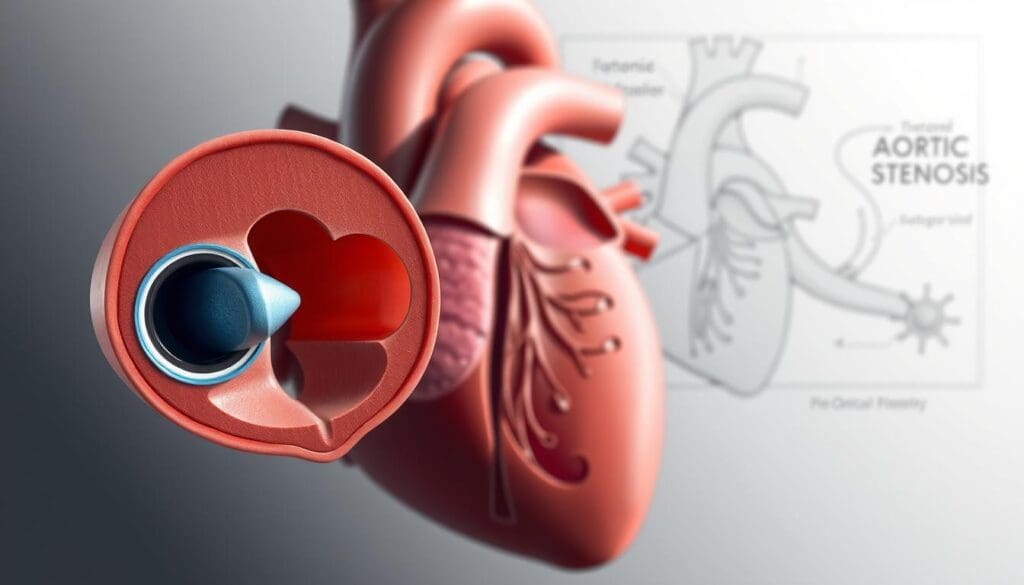
Transcatheter Aortic Valve Replacement (TAVR)
Transcatheter aortic valve replacement (TAVR) is a less invasive option for those at higher risk for surgery. TAVR uses a catheter to place a new valve in the aorta.
TAVR is popular because it’s less invasive and has quicker recovery times. Studies show it can greatly improve symptoms and survival for the right patients.
Post-Treatment Symptom Resolution
After successful treatment, many patients see big improvements in their symptoms. It’s important to follow up regularly to check on the new valve and heart health.
We help patients with post-procedure care and address any concerns. Knowing the treatment options and their outcomes helps patients make informed decisions about their care.
Living with Aortic Stenosis: Lifestyle Modifications
Managing aortic stenosis needs both medical care and lifestyle changes. It’s key to know how our daily actions affect our health.
Exercise Recommendations and Limitations
Exercise is important for aortic stenosis, but finding the right amount is key. Moderate physical activity keeps the heart healthy. But, too much can be risky.
We suggest:
- Brisk walking or light jogging
- Swimming or water aerobics
- Cycling on flat terrain
But, avoid:
- Contact sports
- High-impact aerobics
- Heavy weightlifting
Dietary Considerations for Heart Health
Eating right is key for aortic stenosis. Focus on:
- Fruits and vegetables
- Whole grains
- Lean proteins
- Less saturated fats and cholesterol
Lower sodium intake helps avoid fluid buildup and heart strain.
Monitoring and Follow-up Care
Regular check-ups and monitoring are vital. We recommend:
- Regular visits to your healthcare provider
- Periodic echocardiograms to check valve function
- Watching for symptoms and reporting any changes
Psychological Aspects of Managing a Chronic Condition
Aortic stenosis affects the mind too. It’s important to:
- Get support from loved ones or groups
- Try stress-reducing activities like meditation
- Stay informed to reduce anxiety
By making these lifestyle changes, people with aortic stenosis can manage their condition better and live a fuller life.
Conclusion: Taking Action Against Aortic Narrowing
It’s important to know the signs and causes of aortic stenosis to get help quickly. We’ve covered the basics of this condition, including its causes, symptoms, treatments, and how to live with it. Spotting the symptoms early can make a big difference for patients.
At Liv Hospital, we’re dedicated to helping those with aortic stenosis. Our team uses the latest technology to diagnose and treat this condition. Getting medical help fast can lead to better treatment options, like surgery or TAVR.
Acting quickly to treat aortic stenosis can really help patients. We urge everyone to look after their heart health and see a doctor if they notice any symptoms. Together, we can fight aortic narrowing and help those affected by it.
FAQ
What are the primary symptoms of aortic stenosis?
Symptoms of aortic stenosis include chest pain during activity and shortness of breath. You might also feel persistent fatigue, dizziness, and fainting. These happen because the aortic valve narrows, reducing blood flow.
What causes aortic stenosis?
Aortic stenosis can be caused by age-related calcium buildup on the valve. It can also come from congenital bicuspid valve abnormalities or rheumatic fever complications. Knowing these causes helps in diagnosing and treating the condition.
How is aortic stenosis diagnosed?
Doctors use physical exams, imaging like echocardiography, and lab tests to diagnose aortic stenosis. These methods help figure out how severe the stenosis is.
What are the treatment options for aortic stenosis?
Treatments range from managing symptoms medically to surgical options like Transcatheter Aortic Valve Replacement (TAVR). The right treatment depends on how severe the stenosis is and the patient’s health.
What lifestyle modifications are recommended for patients with aortic stenosis?
Patients should exercise right, eat heart-healthy, and get regular check-ups. These changes help manage the condition and improve life quality.
What are the complications of untreated aortic stenosis?
Untreated aortic stenosis can cause heart failure, arrhythmias, and increase the risk of death. Getting medical help early is key to avoiding these serious issues.
How does age affect the risk of developing aortic stenosis?
Age is a big risk factor for aortic stenosis. It’s more common in older adults because of calcium buildup on the valve leaflets.
Can aortic stenosis be managed with medication alone?
Medication can help manage symptoms, but severe cases often need surgery like TAVR or valve replacement. Surgery is needed to fix the valve narrowing.
What is the significance of regular monitoring for patients with aortic stenosis?
Regular monitoring is key for patients with aortic stenosis. It helps track the condition’s progress, adjust treatments, and quickly address any new symptoms or complications.
Are there any specific dietary recommendations for patients with aortic stenosis?
Patients should eat a heart-healthy diet. This means lots of fruits, vegetables, whole grains, and lean proteins. They should limit saturated fats, cholesterol, and sodium.
References
American Heart Association (AHA): Problem: Aortic Valve Stenosis