Last Updated on November 27, 2025 by Bilal Hasdemir
Aortic valve stenosis is a serious heart condition. It happens when the aortic valve gets narrower. This blocks blood flow from the heart to the rest of the body. At Liv Hospital, we offer top-notch care for those with this condition.
Not treating aortic stenosis can lead to heart failure. It can be caused by many things, like being born with a heart defect, calcification, or rheumatic fever. Symptoms include shortness of breath, chest pain, and feeling dizzy.
Key Takeaways
- Aortic stenosis is a serious heart condition that obstructs blood flow.
- The condition can be caused by congenital defects, calcification, or rheumatic fever.
- Symptoms include shortness of breath, chest pain, and dizziness.
- If left untreated, aortic stenosis can lead to heart failure.
- Advanced care is available at Liv Hospital for patients with aortic stenosis.
Aortic Stenosis Meaning and Basics
Aortic stenosis is when the aortic valve gets narrower. This blocks blood flow from the heart to the rest of the body. If not treated, it can cause serious health problems.
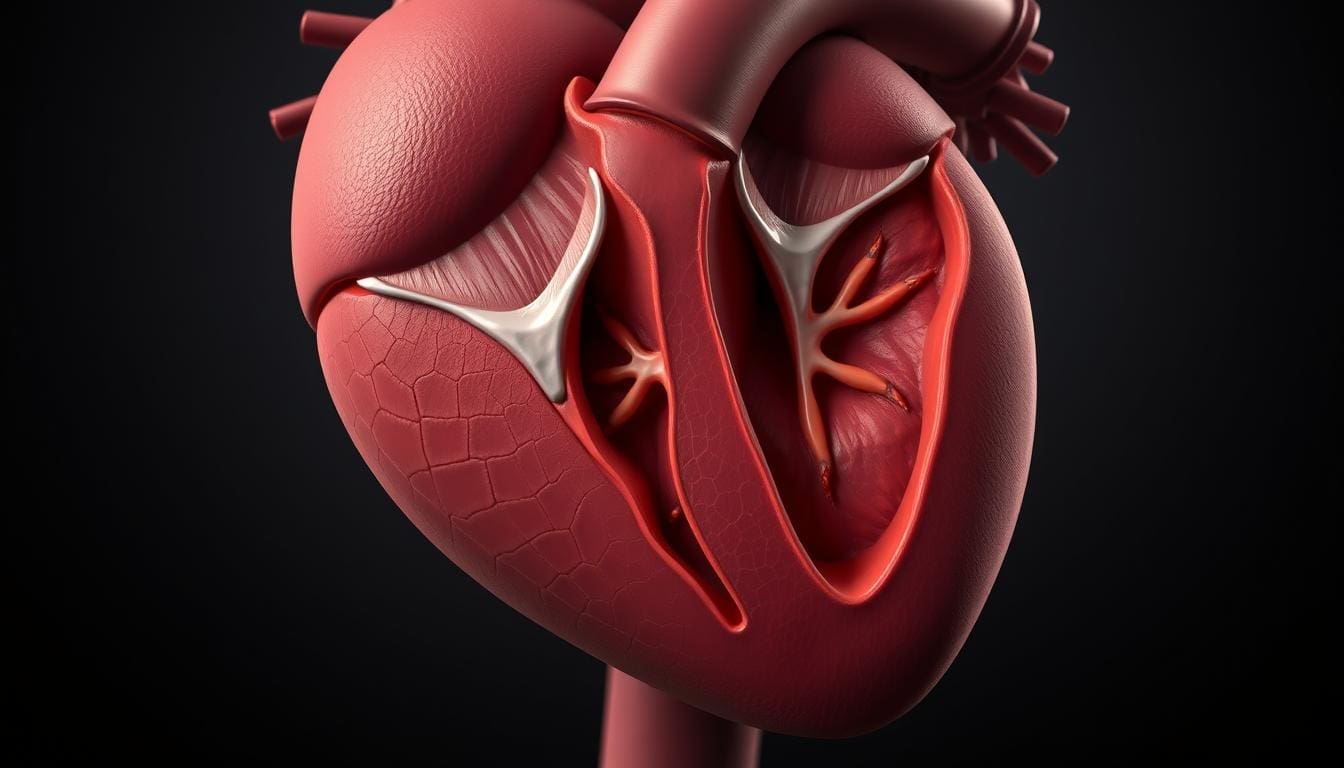
Definition and Mechanism of Valve Narrowing
The aortic valve is key for the heart’s function. It lets blood flow from the left ventricle into the aorta, the biggest artery. Aortic stenosis happens when the valve’s leaflets get thick or calcified, making it hard to open fully. This makes it tough for blood to flow, forcing the heart to work harder.
Valve narrowing is caused by many factors, like age, birth defects, and inflammation. These factors can make the valve opening get smaller over time, affecting the heart’s performance.
Impact on Blood Flow and Heart Function
The narrowing of the aortic valve affects blood flow and heart function. As the valve gets more stenotic, the heart has to work harder to push blood. This can make the heart muscle thicken (hypertrophy), which can lead to heart failure if not treated.
Also, the blocked blood flow can cause symptoms like chest pain, shortness of breath, and fainting. Knowing these symptoms is key for early diagnosis and treatment.
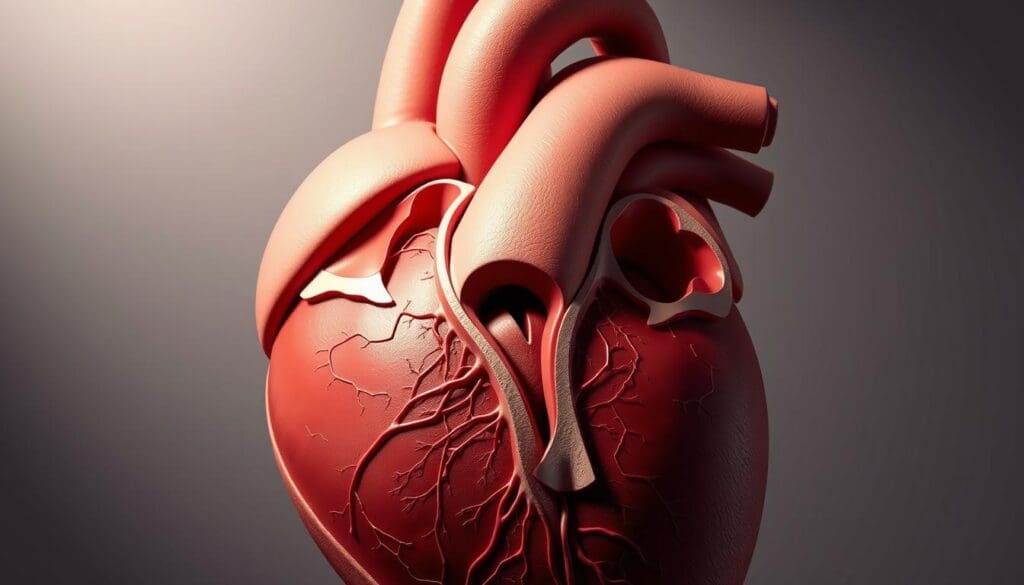
Anatomy and Function of the Aortic Valve
The aortic valve is key to the heart’s efficiency. It’s between the left ventricle and the aorta. It makes sure blood flows right from the heart to the aorta, the biggest artery.
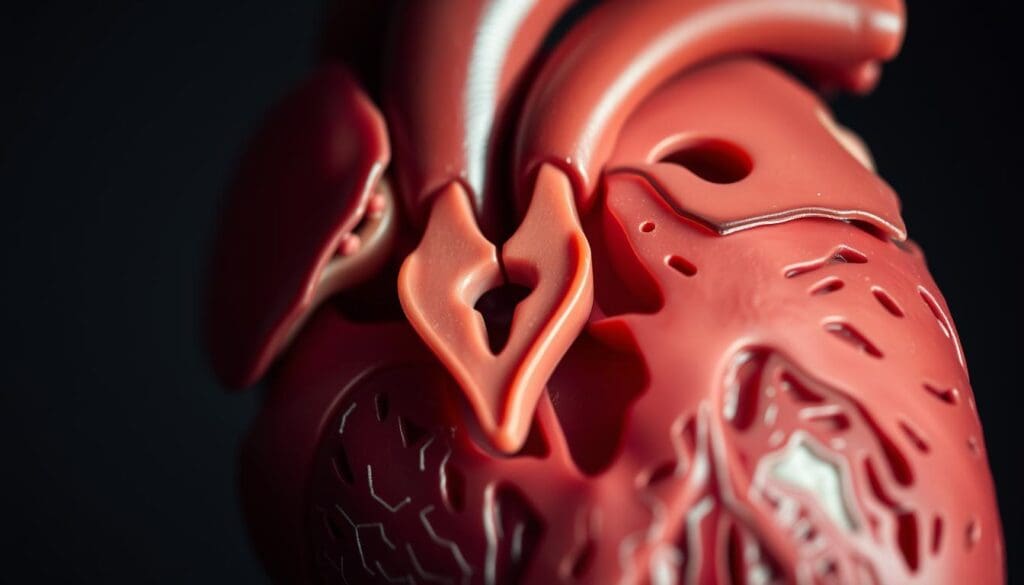
Structure of the Aortic Valve Leaflets
The aortic valve has three leaflets, or cusps. These are thin, flexible tissues. They’re attached to the valve annulus, a ring that supports them.
The leaflets open and close with each heartbeat. This lets blood flow forward and stops it from going back.
Normal Leaflet Function: When the left ventricle contracts, the leaflets open. This lets blood flow into the aorta. When the ventricle relaxes, the leaflets close. This stops blood from flowing back into the heart.
Normal Blood Flow Through the Aortic Valve
Blood flows smoothly through the aortic valve. The valve’s leaflets open fully during systole. This lets blood flow maximally.
During diastole, the leaflets close tightly. This ensures blood keeps flowing forward. It brings oxygen and nutrients to the body’s tissues.
Efficient Valve Function: The aortic valve must work right for good circulation. Any problem, like aortic valve stenosis, can cause big heart issues.
Primary Causes of Aortic Stenosis
Aortic stenosis is a serious heart condition. It’s caused by age-related changes and congenital abnormalities. Knowing these causes helps us find at-risk individuals and manage their care.
Age-Related Calcification and Degeneration
Calcification with age is a big factor in aortic stenosis. As we get older, calcium builds up on the aortic valve. This makes the valve stiff and narrow, blocking blood flow.
Congenital Bicuspid Valve Abnormalities
A congenital bicuspid aortic valve has only two leaflets, not three. This makes the valve work poorly. People with this condition are more likely to get aortic stenosis, often at a younger age.
Rheumatic Fever and Valve Damage
Rheumatic fever can damage heart valves, including the aortic valve. It causes inflammation and scarring, leading to stenosis. Though rare in many places, it’s a big cause of aortic stenosis in some areas.
| Cause | Description | Impact on Aortic Valve |
|---|---|---|
| Age-Related Calcification | Calcium deposits on valve leaflets due to aging | Stiffening and narrowing of the valve opening |
| Congenital Bicuspid Valve | Abnormal valve with two leaflets instead of three | Impaired valve function and possible stenosis |
| Rheumatic Fever | Inflammation and scarring from streptococcal infection | Thickening and stenosis of the valve |
Understanding aortic stenosis causes helps doctors spot risks early. They can then plan better care for these patients.
Risk Factors for Developing Aortic Stenosis
Aortic stenosis risk factors include age, genetics, and health conditions. Knowing these factors helps identify those at higher risk. It also helps in preventing or slowing the condition’s progression.
Age and Gender Considerations
Age is a big risk factor for aortic stenosis, with older adults being more affected. About 2.5 percent of adults over 75 have aortic stenosis. This shows how aging affects the aortic valve.
Men are more likely than women to get aortic stenosis as they age. As we get older, our aortic valve can change. These changes, like calcification and thickening, can make it harder for the valve to work right. Regular check-ups are key for early detection, mainly for older adults.
Genetic and Familial Factors
Genetics also play a part in aortic stenosis. People with a family history of heart valve issues or congenital heart defects are at higher risk. Certain genetic conditions, like bicuspid aortic valve, can also raise the risk.
Familial factors can also affect the risk. If family members have aortic stenosis, talking to a healthcare provider is important. This helps understand the risks and necessary steps.
Medical Conditions That Increase Risk
Some medical conditions can increase the risk of aortic stenosis. These include conditions that cause inflammation or calcification, like rheumatic fever. Keeping the heart healthy by managing these conditions can lower the risk.
High blood pressure, high cholesterol, and kidney disease are also risk factors. These can harm the aortic valve over time. Managing these conditions through lifestyle changes and treatment is vital to reduce the risk of aortic stenosis.
The Progressive Nature of Aortic Stenosis
It’s important to understand how aortic stenosis gets worse. This condition makes the aortic valve narrow. Over time, it changes the heart’s shape and how it works.
Early Stages and Valve Thickening
In the early stages, the aortic valve gets thick and stiff. This happens because of age-related calcification. At first, this might not cause many symptoms. But as it gets worse, the valve blocks blood flow from the heart.
At first, aortic stenosis might not show symptoms. So, it’s key for people at risk to get checked regularly. When the valve gets too narrow, symptoms like chest pain or trouble breathing can start.
Advanced Progression and Cardiac Remodeling
As aortic stenosis gets worse, the heart changes a lot. The heart muscle gets thicker to work harder. This helps at first but can lead to heart failure if not treated.
Stages of Aortic Stenosis Progression
| Stage | Characteristics | Symptoms |
|---|---|---|
| Early Stage | Valve thickening, mild stenosis | Often asymptomatic |
| Moderate Stage | Progressive valve narrowing | Possible chest pain, shortness of breath |
| Advanced Stage | Severe stenosis, cardiac remodeling | Significant symptoms, heart failure risk |
Getting aortic stenosis treated early is key to avoiding serious problems. Regular check-ups and the right treatment can greatly help patients.
Recognizing Symptoms of Aortic Stenosis
The symptoms of aortic stenosis can be hard to spot at first. But knowing them is key to managing the condition well. Early detection is important for better treatment results.
Asymptomatic Phase and Silent Progression
Aortic stenosis often starts without symptoms. Patients might not feel anything even though the valve is getting narrower. Regular check-ups are important to catch it early.
Classic Triad: Angina, Dyspnea, and Syncope
As the condition gets worse, patients may feel chest pain, shortness of breath, and fainting. These signs mean the condition has reached a serious stage.
Let’s look at these symptoms closer:
| Symptom | Description | Implication |
|---|---|---|
| Angina | Chest pain or discomfort due to reduced blood flow to the heart | Indicates significant valve narrowing |
| Dyspnea | Shortness of breath, specially during exertion | Suggests increased pressure on the heart |
| Syncope | Fainting or near-fainting episodes | Signals reduced blood flow to the brain |
Exercise Intolerance and Reduced Stamina
Patients with severe aortic stenosis may also feel tired easily and have less stamina. This is because their heart can’t pump enough blood during exercise. It leads to feeling tired and short of breath.
It’s important to recognize these symptoms for timely medical help. If you or someone you know is showing these signs, see a doctor right away.
Severity Classification of Aortic Stenosis
Knowing how severe aortic stenosis is helps doctors decide the best treatment. They look at the valve area, mean gradient, and jet velocity. These are key signs of how bad the stenosis is.
Mild Aortic Valve Stenosis and Monitoring
Mild stenosis means the valve area is over 1.5 cm², the mean gradient is under 20 mmHg, and the jet velocity is under 2.5 m/s. People with mild stenosis usually don’t have symptoms. They are watched closely with echocardiograms to see if the disease gets worse.
Moderate Stenosis and Management
Moderate stenosis has a valve area between 1.0 and 1.5 cm², a mean gradient between 20 and 40 mmHg, and a jet velocity between 2.5 and 4.0 m/s. For moderate stenosis, doctors might suggest closer monitoring, changes in lifestyle, and possibly medicine to manage symptoms and slow the disease.
Severe Aortic Stenosis and Intervention Indicators
Severe stenosis is shown by a valve area under 1.0 cm², a mean gradient over 40 mmHg, and a jet velocity over 4.0 m/s. Those with severe stenosis often need surgery or TAVR to relieve symptoms and improve their health. Doctors decide on these treatments based on symptoms, heart function, and other health factors.
In summary, knowing the severity of aortic stenosis is key to managing it well. Understanding the severity helps doctors give tailored care. This improves patient outcomes and aortic stenosis prognosis.
Diagnostic Approaches for Aortic Stenosis
Diagnosing aortic stenosis involves both physical checks and advanced tests. We use different methods to find and measure the severity of aortic stenosis.
Physical Examination and Heart Murmur Detection
First, we do a physical check. A doctor listens for heart sounds with a stethoscope. A systolic murmur, heard at the right second intercostal space, might show aortic stenosis. We also look for slow pulse and low pulse pressure.
Heart murmur detection is key. It can show valve problems early. Our team knows how to spot the murmurs of aortic stenosis.
Echocardiography and Valve Assessment
Echocardiography is a key test for aortic stenosis. It lets us see the aortic valve and check its work. We measure blood flow speed to see how bad the stenosis is.
Echocardiography helps us see the valve’s shape, calcification, and how it moves. Doppler echocardiography lets us measure the pressure difference across the valve. This helps us know how severe the stenosis is.
Advanced Imaging and Cardiac Catheterization
Sometimes, we use advanced imaging like CT or MRI. These tests give detailed views of the valve and heart. They help us plan treatments.
Cardiac catheterization is used to measure the pressure difference across the valve and check for heart artery disease. We use it when other tests don’t give clear results or when we plan to intervene.
By using these methods together, we can accurately diagnose aortic stenosis. We can then plan the best treatment for each patient.
Comprehensive Treatment Options for Aortic Stenosis
Managing aortic stenosis requires a mix of medical, surgical, and interventional methods. It’s important to know the benefits and risks of each treatment.
Medical Management and Symptom Control
First, we focus on controlling symptoms and managing related health issues. We keep a close eye on the disease’s progression and adjust treatment plans as needed.
Key aspects of medical management include:
- Monitoring valve function and overall heart health
- Managing symptoms such as chest pain and shortness of breath
- Controlling risk factors like high blood pressure and high cholesterol
Surgical Aortic Valve Replacement Techniques
Surgical aortic valve replacement (SAVR) is a traditional and effective treatment for severe aortic stenosis. We discuss the surgical techniques and considerations for this procedure.
| Surgical Approach | Description | Benefits |
|---|---|---|
| Mechanical Valve | Replacement with a mechanical prosthetic valve | Durable, long-lasting |
| Bioprosthetic Valve | Replacement with a biological tissue valve | Less need for anticoagulation therapy |
Transcatheter Aortic Valve Replacement (TAVR) Procedure
Transcatheter aortic valve replacement (TAVR) is a less invasive option for those at higher risk for surgery. We outline the TAVR procedure and its advantages.
TAVR involves:
- Accessing the aortic valve through a catheter, typically via the femoral artery
- Deploying a new valve within the existing one
- Restoring normal blood flow with minimal invasion
In conclusion, the choice of treatment for aortic stenosis depends on various factors. These include the severity of the condition, patient health, and preferences. We work closely with patients to find the best treatment plan.
Recovery and Rehabilitation After Valve Intervention
The time after valve intervention is key for a good recovery and rehabilitation. We help patients through each stage, from hospital care to long-term programs.
Post-Procedure Hospital Care
Patients with severe aortic stenosis need close watch in the hospital. This care helps avoid complications and aids in a smooth start to recovery.
- Monitoring for signs of bleeding or cardiac complications
- Managing pain and discomfort
- Initiating early mobilization to prevent complications
Our team works with patients to meet their needs and make recovery comfortable.
Long-term Recovery and Activity Guidelines
After leaving the hospital, living a heart-healthy lifestyle is essential. This means slowly increasing physical activity, eating right, and taking medicines as directed.
| Activity Level | Recommended Actions | Timeline |
|---|---|---|
| Low-Intensity Activities | Short walks, light stretching | First 2-4 weeks |
| Moderate Activities | Brisk walking, light aerobics | 4-8 weeks |
| High-Intensity Activities | Strenuous exercise, heavy lifting | After 8 weeks, with doctor’s approval |
Following these guidelines is important for a safe and effective recovery.
Cardiac Rehabilitation Programs
Cardiac rehabilitation includes exercise, heart-healthy education, and stress counseling. It’s made to help patients get the best results after aortic stenosis treatment.
Being in cardiac rehab can improve heart health, lessen symptoms, and boost quality of life.
We know recovery from valve intervention needs a full plan. With medical care, lifestyle changes, and rehab, we help patients get the best recovery and health benefits.
Living with Aortic Stenosis: Management Strategies
Living with aortic stenosis can be tough, but the right strategies can help. A diagnosis means big changes in lifestyle. Yet, with the right approach, managing the condition is possible.
Lifestyle Modifications and Heart-Healthy Habits
For aortic stenosis, a heart-healthy lifestyle is key. This means eating right, exercising, and not smoking. A diet full of fruits, veggies, and whole grains is good for your heart. Eating foods low in saturated fats and high in omega-3 fatty acids is also beneficial.
Regular exercise, like walking or swimming, boosts heart health. But, always talk to a doctor before starting new exercises. Managing stress through meditation or yoga can also help your well-being.
“A heart-healthy lifestyle is not just about diet and exercise; it’s about making sustainable changes that improve your overall quality of life.”
Regular Monitoring and Follow-up Protocol
Regular checks are essential for managing aortic stenosis. This includes doctor visits, echocardiograms, and other tests. Tracking symptoms like chest pain or shortness of breath is important. These signs can mean the condition is getting worse.
- Schedule regular appointments with your cardiologist.
- Keep a log of your symptoms and any changes.
- Adhere to recommended diagnostic testing schedules.
By making lifestyle changes and getting regular check-ups, patients can do better. Early recognition and management of symptoms of aortic stenosis are vital. This helps avoid serious problems.
Conclusion
Understanding aortic stenosis is key to knowing its severity. This condition affects blood flow and heart function. If not treated, it can lead to serious problems.
The causes of aortic stenosis vary. They include age-related calcification, congenital valve issues, and rheumatic fever. Spotting these causes early is vital for treatment.
Symptoms like chest pain, shortness of breath, and fainting are signs the disease is getting worse. Treatment options range from medication to surgery. The right choice depends on the condition’s severity and the patient’s health.
Knowing about aortic stenosis, its causes, and treatments helps patients and doctors manage it well. Early detection and proper care are essential for better outcomes.
FAQ
What is aortic stenosis?
Aortic stenosis is a heart problem. It happens when the aortic valve gets narrower. This blocks blood flow from the heart to the aorta.
What are the primary causes of aortic stenosis?
Main causes include age-related wear and tear, congenital valve issues, and rheumatic fever.
What are the symptoms of aortic stenosis?
Symptoms include chest pain, shortness of breath, and fainting. People may also feel tired easily and have trouble exercising.
How is the severity of aortic stenosis classified?
It’s divided into mild, moderate, and severe. Treatment plans change based on the severity.
What diagnostic methods are used to detect aortic stenosis?
Doctors use physical checks, echocardiograms, and imaging tests. Cardiac catheterization is also used.
What are the treatment options for aortic stenosis?
Options include medication, open-heart surgery, and a less invasive procedure called TAVR.
What is the recovery process like after valve intervention for aortic stenosis?
Recovery involves hospital care and following long-term guidelines. Cardiac rehab is also important.
How can patients manage aortic stenosis and improve their quality of life?
Patients can improve their life by eating well, exercising, and following up with doctors regularly.
What is the prognosis for patients with severe aortic stenosis?
Timely treatment greatly improves outcomes. Surgery or TAVR can significantly help.
Can aortic stenosis be prevented?
Some risks can’t be avoided, but managing high blood pressure and a healthy lifestyle can help.
References
NCBI Bookshelf (National Library of Medicine): Aortic Stenosis (Specific NCBI ID)
MedlinePlus (National Library of Medicine): Aortic Valve Stenosis





