Last Updated on November 26, 2025 by Bilal Hasdemir
Cardiac stents help keep blood flowing through blocked arteries. At Liv Hospital, we focus on what’s best for each patient’s heart health. The number of heart stents needed varies, based on how blocked the arteries are and the patient’s overall heart condition. How many heart stents can you have? Get the expert answer on whether there is a maximum limit and what the safety risks are.
We know every patient is different. Deciding to use a stent is based on careful checks and what’s medically needed. Our aim is to give each patient the care they need for the best results.
Key Takeaways
- The number of heart stents is determined on a case-by-case basis.
- Factors such as artery blockage severity and overall heart health play a crucial role.
- A patient-focused approach is essential for effective heart health management.
- Comprehensive care and thorough evaluations guide stent placement decisions.
- Individual factors influence the limit on the number of stents a person can have.
Understanding Heart Stents and Their Purpose
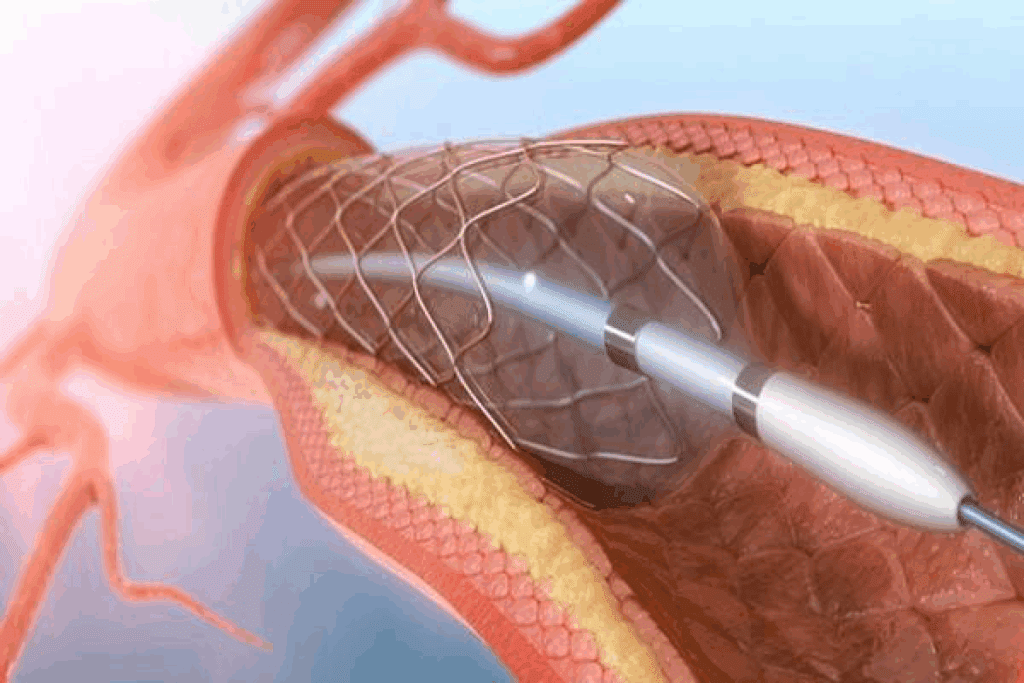
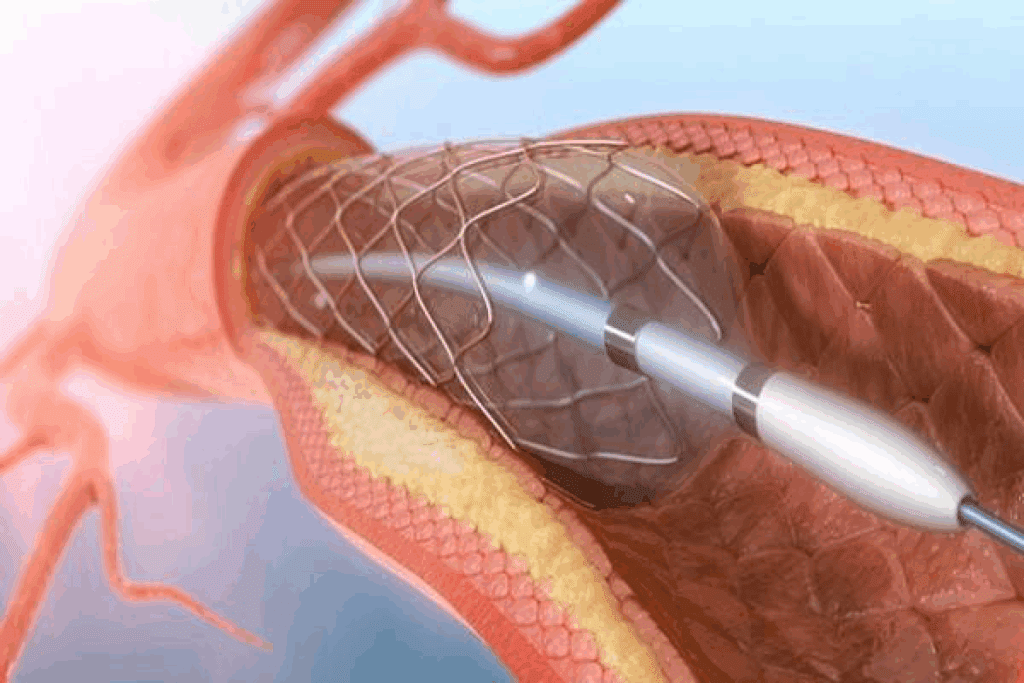
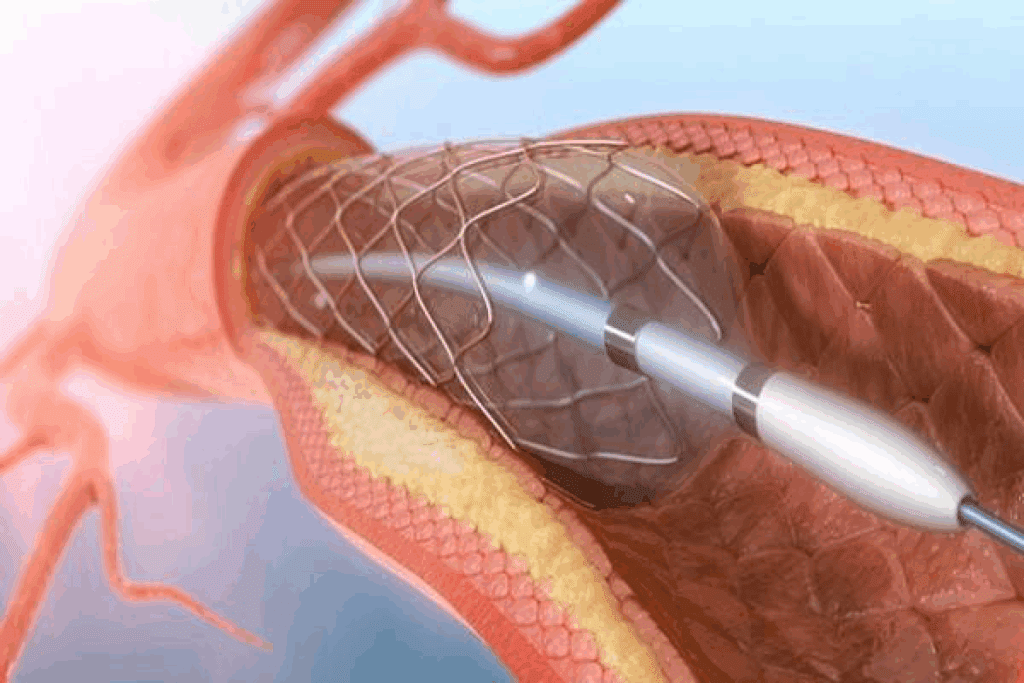
Coronary stents are tiny, expandable devices that help restore normal blood flow to the heart muscle. These small mesh tubes are inserted into the coronary arteries to keep them open. This improves blood supply to the heart. We will explore the details of heart stents, their functionality, and the various types available.
What Are Heart Stents?
Heart stents, also known as coronary stents, are small, expandable metal mesh tubes. They are designed to be inserted into the coronary arteries, which supply blood to the heart muscle. The primary purpose of a stent is to keep the artery open, thereby improving blood flow to the heart.
How Stents Work to Improve Blood Flow
When a coronary artery is narrowed or blocked due to plaque buildup (a condition known as atherosclerosis), it can lead to reduced blood flow to the heart. This can cause chest pain or even a heart attack. Stents work by being placed at the site of the blockage.
Once in place, the stent is expanded, pushing the plaque against the artery wall and keeping the artery open. This procedure, known as angioplasty with stenting, restores normal blood flow to the heart muscle.
Types of Coronary Stents Available
There are several types of coronary stents available, each with its own characteristics and benefits.
- Bare-metal stents: These are the original type of stent and are made of metal mesh.
- Drug-eluting stents: These stents are coated with medication that helps prevent the artery from re-narrowing.
- Bioresorbable stents: These stents are made of materials that gradually dissolve in the body over time.
| Stent Type | Description | Benefits |
| Bare-metal | Made of metal mesh | Simple design, less expensive |
| Drug-eluting | Coated with medication to prevent re-narrowing | Reduced risk of artery re-narrowing |
| Bioresorbable | Made of materials that dissolve over time | May reduce long-term complications, restore natural artery function |
Understanding the different types of heart stents and their purposes is crucial for patients and healthcare providers alike. By knowing how stents work and the options available, individuals can make informed decisions about their cardiovascular care.
How Many Heart Stents Can You Have?
Many things affect how many heart stents a person can have. The disease’s complexity, where blockages are, and the patient’s health are key. These factors play a big role.
Is There a Definitive Numerical Limit?
There’s no fixed number for heart stents. Studies show stent numbers vary greatly among patients. Doctors decide based on each patient’s unique situation and heart anatomy.
Documented Cases of Multiple Stent Placements
Some patients have had more than five stents. This is due to severe coronary artery disease. These cases are often handled in specialized centers with a team of experts. Success depends on the patient’s heart health and other health issues.
Factors That Influence Maximum Stent Numbers
Several important factors affect the number of stents:
- The extent and severity of coronary artery disease
- The location and complexity of coronary blockages
- The patient’s overall heart function and health status
- The presence of comorbidities such as diabetes or kidney disease
Knowing these factors helps doctors make better decisions about stent placement.
Common Scenarios: 2-3 Stents in Heart
Putting 2-3 stents in the heart is a common way to treat complex heart disease. It’s often needed when there are many blockages or complex problems in the heart’s arteries.
Clinical Situations Requiring 2 Heart Stents
Two stents might be used when there are blockages in different heart arteries or in the same artery but in different spots. For example, a blockage in the left anterior descending artery and another in the circumflex artery. This helps get blood flowing again and relieves symptoms.
3 Stents in Heart: When Is This Necessary?
Three stents are used for severe heart disease that affects many arteries or has complex problems. This could mean stenting several major arteries or dealing with many issues in one artery. The choice to use three stents depends on the patient’s health, the disease’s complexity, and other factors.
Outcomes and Success Rates with 2-3 Stents
The results for patients with 2-3 stents can differ based on their health, the disease’s complexity, and how well the stenting goes. Most studies show that these patients see big improvements in symptoms and life quality.
| Number of Stents | Success Rate | Complication Rate | Average Hospital Stay |
| 1 Stent | 95% | 5% | 2 days |
| 2 Stents | 92% | 8% | 3 days |
| 3 Stents | 90% | 10% | 4 days |
In summary, using 2-3 stents is a common and effective way to treat complex heart disease. Knowing when and how these procedures work helps doctors take better care of their patients and improve outcomes.
Complex Cases: 4-5 Stents in Heart
Dealing with complex coronary artery disease is tough. It often means using more than one stent. Understanding how 4 or 5 stents help fix heart problems is key.
4 Stents in Heart: Managing Multi-Vessel Disease
Using 4 stents to tackle multi-vessel disease is a detailed job. Multi-vessel disease means many arteries are blocked. This raises the risk of heart attacks and other heart problems.
By putting stents in different arteries, we boost blood flow to the heart. This helps lessen symptoms and improves health outcomes.
“The use of multiple stents in multi-vessel disease has revolutionized the treatment of complex coronary artery disease,” says a leading cardiologist. “With advancements in stent technology and procedural techniques, we’re able to offer patients more effective and safer treatment options.”
5 Stents in Heart: Challenging Anatomies and Approaches
Putting 5 stents in the heart is even harder. It’s needed for very complex cases or severe disease. Challenging anatomies include twisted vessels or hard-to-reach blockages.
Advanced imaging and careful planning are crucial for success. This ensures the stents are placed correctly.
- Advanced imaging techniques to visualize complex anatomies
- Meticulous procedural planning to ensure precise stent placement
- Use of specialized stents designed for complex lesions
Long-Term Prognosis with Multiple Stents
The future looks good for patients with 4 or 5 stents, depending on several factors. These include the patient’s overall health, the extent of heart disease, and following doctor’s orders after the procedure.
While multiple stents can greatly improve life quality, it’s vital to stay on top of care. This includes making lifestyle changes, taking medications as directed, and attending regular check-ups.
As an expert doctor notes, “Long-term success with multiple stents requires a comprehensive approach to care, including lifestyle modifications, medication adherence, and regular follow-up appointments.”
Extreme Cases: Can You Have 6 or More Stents in Your Heart?
It’s rare, but some people have had more than 6 stents in their hearts. These cases often involve very complex heart disease. They pose big challenges for heart doctors.
Documented Cases of Patients with 6+ Stents
There are cases where patients got 6 or more stents because of severe heart disease. A study in a cardiology journal showed several such cases. These patients had stents placed over many procedures.
“In our experience, patients with multiple stents often have complex disease patterns that require tailored treatment strategies,” said a leading cardiologist in an interview.
These cases usually involve disease in many heart vessels, blocked arteries, or failed stents before. Doctors decide on more stents based on the patient’s health, disease severity, and the benefits and risks of further treatment.
Special Considerations for Extensive Stenting
Having 6 or more stents raises several concerns. These include higher risks of complications during and after the procedure. There’s also a chance of the stented area narrowing again, which might need more treatment.
| Consideration | Description | Impact |
| Procedural Risks | Increased risk of complications during and after the procedure | Higher risk of adverse outcomes |
| Restenosis Risk | Potential for the stented area to narrow again | May require additional interventions |
| Long-term Health | Impact on the patient’s overall cardiac health and function | May influence future treatment options |
When Alternatives May Be Preferred
In some cases, doctors might prefer other treatments over many stents. These could be coronary artery bypass grafting (CABG) or treatments focusing on lifestyle changes and medication.
Alternatives to Extensive Stenting:
- Coronary Artery Bypass Grafting (CABG)
- Optimized medical therapy
- Lifestyle modifications
The choice between many stents and other treatments depends on many factors. These include the patient’s condition, overall health, and personal preferences. A team of healthcare professionals works together to find the best treatment plan.
Factors That Determine the Number of Stents Needed
The number of stents a patient needs depends on several important factors. It’s key for doctors and patients to understand these to make the best treatment choices.
Coronary Anatomy and Blockage Locations
The shape of the coronary arteries and where blockages are located matter a lot. Complex coronary anatomy might mean more stents are needed for good blood flow. For example, blockages in many parts of the arteries could mean using several stents.
Severity and Extent of Coronary Artery Disease
The seriousness and spread of coronary artery disease (CAD) are big factors in stent numbers. Patients with widespread CAD might need more stents to cover all blockages or long stretches in arteries.
Overall Heart Function and Health
The heart’s overall health and function are also key. Patients with heart issues or other health problems might need a special stenting plan. This could mean using fewer stents to lower risks.
Age and Comorbidity Considerations
A patient’s age and other health issues can also affect stent numbers. Older patients or those with many health problems might get a more careful approach. This balances the benefits of stenting with the risks.
By looking at these factors, doctors can create a treatment plan that works best for each patient needing stents.
How Many Stents Can Be Placed at One Time
Doctors often place more than one stent in a single session. But, they must carefully consider the patient’s health and the blockages’ complexity. The decision to use multiple stents at once or to do them in stages depends on several factors.
These factors include the patient’s overall health, the severity of the coronary artery disease, and the specific anatomy of the coronary arteries.
Single-Session Multiple Stent Procedures
Single-session multiple stent procedures are often preferred when possible. They reduce the need for repeated catheterizations and can shorten recovery time. This approach is especially beneficial for patients with multiple blockages in close proximity, as it streamlines the treatment process.
However, single-session procedures also carry potential risks. These include increased contrast load and longer procedural times. These can impact kidney function and increase the risk of complications.
Staged Procedures for Complex Cases
For more complex cases or when the patient’s condition is not stable, staged procedures may be preferred. This involves placing stents in separate sessions, allowing for recovery time between procedures.
Staged procedures can reduce the risk of complications associated with longer procedures. They allow for a more gradual recovery. However, they also mean that the patient will undergo multiple catheterization procedures. This can be associated with additional risks and recovery periods.
Recovery Differences Between Approaches
The recovery process can vary significantly between single-session and staged procedures. Patients who undergo single-session multiple stent placements may require closer monitoring post-procedure. This is due to the complexity and length of the procedure.
In contrast, staged procedures allow for a potentially easier recovery after each session. This is because the procedures are typically less complex.
| Procedure Type | Recovery Time | Risk Level |
| Single-Session | Typically longer due to complexity | Higher due to increased contrast load and procedural time |
| Staged Procedures | Gradual recovery between sessions | Variable, depends on individual sessions |
In conclusion, the decision on how many stents can be placed at one time is highly individualized. It takes into account the patient’s specific condition, the complexity of the coronary artery disease, and other relevant factors. Both single-session and staged procedures have their advantages and potential drawbacks. The choice between them should be made based on a thorough evaluation by a cardiologist.
How Many Stents Can Be Placed in One Artery
The number of stents in one artery depends on many things. Cardiologists look at the artery’s shape, the size of the blockage, and the patient’s health. These factors are key in deciding how many stents are safe to use.
Technical Limitations of Single-Vessel Stenting
Single-vessel stenting is common but has its limits. The stent’s length and width, and the artery’s twists and turns, matter a lot. Longer lesions might need more than one stent, which can raise the risk of problems.
Important technical points include:
- The maximum length of stents available
- The risk of overlapping stents and its implications
- The artery’s size and its ability to accommodate stents
Overlapping Stents: Benefits and Risks
Overlapping stents are sometimes needed for long lesions. But, they come with risks. The good sides are:
- Ensuring complete lesion coverage
- Reducing the risk of restenosis
But, there are downsides like more inflammation, clotting, and restenosis at the overlap. It’s vital to plan carefully and place stents precisely to lessen these risks.
Long Lesions Requiring Multiple Stents
For very long lesions, more than one stent is often needed. This needs careful planning to get the right stent size and placement. The aim is to cover the diseased area fully while avoiding complications.
Important things to consider for long lesions are:
- Assessing the lesion’s length and complexity
- Choosing the appropriate stent size and type
- Planning for potential overlap between stents
By looking at these factors, doctors can decide how many stents are needed for one artery. They aim to treat the disease effectively while keeping risks low.
Risks and Complications of Multiple Stent Placements
Multiple stent placements are often lifesaving but come with risks. Patients and healthcare providers must consider these carefully. Understanding these risks is key for making informed decisions about coronary artery disease treatment.
Increased Risk of Restenosis
One major concern is the risk of restenosis, or arteries narrowing again. This can happen because the body reacts to the stent. Drug-eluting stents try to prevent this by releasing medicine that stops cell growth.
Even with these stents, restenosis is still a worry, especially with multiple stents. We must think carefully about the benefits and risks for each patient.
Procedural Complications
Putting in multiple stents makes the procedure more complex. This can lead to higher risks of procedural complications. These can include bleeding, damage to blood vessels, and reactions to dye used during the procedure. Though rare, these complications can be serious.
To lower these risks, we use advanced imaging and plan each procedure carefully. We consider the patient’s health and the shape of their arteries.
Long-Term Medication Requirements
Patients with multiple stents often need long-term antiplatelet therapy to stop clots. This medicine is vital but also carries risks, like bleeding.
We help patients manage their medication. We balance the need to prevent clots with the risk of bleeding.
Impact on Future Treatment Options
Having multiple stents can also affect future treatments. In some cases, it might make other surgeries harder or less likely.
When we consider multiple stent placements, we look ahead. We plan with a team of healthcare providers to ensure future care options are considered.
Conclusion: Balancing Need and Risk with Heart Stents
Heart stents are a big deal in heart care. They help blood flow better and ease symptoms. But, they also come with risks like restenosis and complications during the procedure.
When deciding on heart stents, we weigh the benefits against the risks. We look at things like the heart’s shape, how well it works, and the patient’s overall health. This way, we tailor care to each person, aiming for the best results with the least risk.
Getting heart stents right is all about finding the right balance. It’s about giving patients the best treatment for their heart issues. This approach improves their health and life quality.
FAQ
How many heart stents can you have in your heart?
The number of heart stents varies. It depends on the disease’s severity, heart health, and body anatomy. We explore the factors that affect the maximum number of stents.
Is there a limit to the number of stents that can be placed in the heart?
There’s no exact number limit for stents. But, doctors decide based on the heart’s anatomy, disease severity, and function.
How many stents can be placed in one artery?
The number in one artery depends on the lesion’s length and complexity. While possible, placing multiple stents in one artery carries risks. The decision is based on the patient’s needs.
Can you have 6 or more stents in your heart?
Yes, some patients have had 6 or more stents. These cases are complex and require careful risk and benefit assessment.
What are the risks associated with having multiple stents?
Multiple stents increase risks like restenosis and complications. They also require long-term medication and may limit future treatments. Each case is carefully considered.
How many stents can be placed at one time?
The number placed at once varies by case complexity and patient health. Both single-session and staged procedures are used, based on the patient’s needs and doctor’s judgment.
What factors determine the number of stents needed?
Factors include the heart’s anatomy, blockage locations, disease severity, and overall heart function. Age and other health conditions also play a role. A thorough evaluation guides the decision.
Are there alternatives to stenting for coronary artery disease?
Yes, alternatives include other procedures, medical therapy, and lifestyle changes. The choice depends on the patient’s characteristics and disease severity.
How do multiple stents affect long-term heart health?
The long-term effect of multiple stents varies. It depends on the treated condition, other health issues, and post-procedure care. Regular follow-ups with a healthcare provider are crucial.
Can having multiple stents impact future heart surgery or treatments?
Yes, multiple stents can affect future treatments, including surgery. They may influence the complexity and approach of subsequent interventions. Careful planning is essential.
Reference
- Fröhlich, G. M., et al. (2023). Long stent implantation on the left anterior descending artery: Long-term outcomes. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10779530