Last Updated on November 26, 2025 by Bilal Hasdemir

Cholecystitis is when the gallbladder gets inflamed. This usually happens when gallstones block the cystic duct. It can cause a lot of pain and serious problems if not treated quickly.
What is cholecystitis ? Your ultimate guide explains the alarming causes, symptoms, diagnosis, and management you need to know.
The gallbladder is a small, pear-shaped organ under the liver on the right side. It helps with digestion. Inflammation of this organ can be due to gallstones or other reasons. It can cause a lot of discomfort and health risks.
It’s important to know about the causes, symptoms, diagnosis, and treatment of cholecystitis. At Liv Hospital, we focus on accurate diagnosis and care based on evidence. This helps us treat this serious condition well.
Key Takeaways
- Cholecystitis is the inflammation of the gallbladder, often caused by gallstones.
- The condition can lead to severe abdominal pain and potentially serious complications.
- Prompt diagnosis and treatment are key to managing cholecystitis well.
- Liv Hospital emphasizes reliable diagnosis and patient comfort in treating cholecystitis.
- Understanding the causes and symptoms is important for addressing this condition.
Understanding What Is Cholecystitis

Cholecystitis is when the gallbladder gets inflamed. This can happen suddenly or over time. Gallstones are the main reason for this inflammation.
Definition and Clinical Significance
Cholecystitis is when the gallbladder gets inflamed. This usually happens when a gallstone blocks the cystic duct. This blockage causes chemical irritation and secondary bacterial infection, making the inflammation worse.
This condition can cause a lot of pain. If not treated, it can lead to serious problems. Knowing about cholecystitis is key to getting the right treatment.
Acute vs. Chronic Cholecystitis
Cholecystitis can be either acute or chronic.
- Acute Cholecystitis: This happens suddenly and needs quick medical help. It’s usually caused by a gallstone blocking the cystic duct, causing severe inflammation.
- Chronic Cholecystitis: This is when the gallbladder gets inflamed many times. It can cause scarring and thickening of the gallbladder wall. It may need surgery to manage.
Knowing if it’s acute or chronic is important for treatment. Acute cholecystitis needs fast care, while chronic may need ongoing management and possibly surgery.
It’s important for doctors to understand the difference between acute and chronic cholecystitis. Acute cholecystitis is caused by blockage of bile flow, chemical irritation, and bacterial infection. This shows how complex the condition is.
Epidemiology and Risk Factors

Understanding cholecystitis is key to preventing and treating it. Cholecystitis, often linked to gallstones, is a big health issue worldwide.
Prevalence Statistics
In the UK, gallstones affect over 10% of adults. This shows how common gallbladder disease is. Gallstones are a big risk for cholecystitis.
Demographic Patterns
Some groups face a higher risk of cholecystitis. Women, people with obesity, pregnant individuals, and those in their 40s are more at risk. Knowing these patterns helps target prevention efforts.
| Demographic Factor | Risk Level | Reason |
| Gender | Higher in Women | Hormonal influences, like during pregnancy |
| Obesity | Higher Risk | Metabolic changes and more cholesterol in bile |
| Age | Increased risk in 40s | Age and lifestyle factors add up |
| Pregnancy | Higher Risk | Hormonal changes affect gallbladder function |
The table above highlights key demographic risk factors for cholecystitis. It shows why these factors are important in prevention and treatment.
Anatomy and Physiology of the Gallbladder
The gallbladder is a key organ that holds bile made by the liver. It plays a big part in digestion. It’s found under the liver, in the right upper part of the abdomen, and looks like a small pear.
Its main job is to store and make bile more concentrated. This concentrated bile then goes into the small intestine to help with fat digestion. Knowing how the gallbladder works helps us understand its role in digestion.
Anatomical Relationships
The gallbladder is connected to several important parts. It links to the liver through the cystic duct. This duct merges with the common hepatic duct to form the common bile duct. This duct then empties into the second part of the duodenum.
Because of its location under the liver, the gallbladder can get diseases like gallstones. Its close relationship with the duodenum and pancreas means gallbladder diseases can sometimes be mistaken for diseases in these organs.
Bile Production and Storage
The liver makes bile all the time and stores it in the gallbladder. The gallbladder makes the bile more concentrated by removing extra water and salts. This makes it better for breaking down fats.
When fatty foods reach the duodenum, a hormone called cholecystokinin is released. This hormone makes the gallbladder contract and release bile into the common bile duct. Then, it goes into the duodenum. This is key for breaking down and absorbing fats.
In short, the gallbladder’s role in storing and releasing bile is essential for fat digestion. Its connections with the liver, cystic duct, and duodenum highlight its importance in the digestive system.
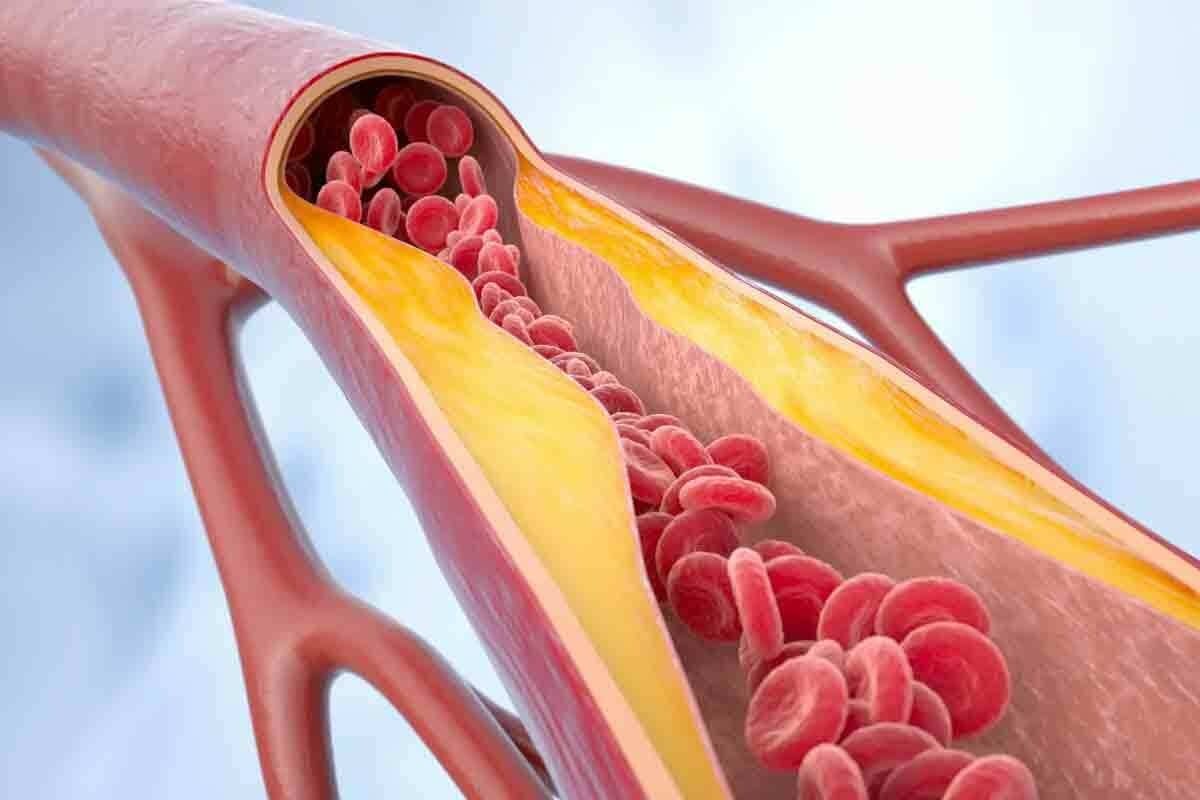
Pathophysiology of Acute Cholecystitis
To understand acute cholecystitis, we must look at how it starts. It often begins with a blockage in the cystic duct, usually by a gallstone. This blockage causes biliary colic and then inflammation.
Obstructive Mechanisms
The blockage of the cystic duct is key in starting acute cholecystitis. This blockage can be from gallstones, sludge, or other things that stop bile flow. The gallbladder gets too full and the pressure inside can cause the wall to get inflamed and ischemic.
Chemical Inflammation Process
Chemical inflammation happens because of the buildup of harmful substances in the blocked gallbladder. These substances irritate the gallbladder, making the inflammation worse. This makes the disease get worse.
Bacterial Infection Role
At first, acute cholecystitis is not caused by bacteria. But, bacteria like Escherichia coli and Klebsiella can infect the bile later. This makes the inflammation even more severe.
Progression to Necrosis and Perforation
If not treated, acute cholecystitis can get worse. It can lead to gangrene, necrosis, and even perforation of the gallbladder. The high pressure and lack of blood can cause the gallbladder wall to die, leading to a serious infection in the belly.
Understanding how acute cholecystitis progresses is vital. It shows why quick diagnosis and treatment are so important. Knowing the causes helps doctors manage the disease better.
Etiology of Cholecystitis
Cholecystitis has many causes, including gallstones and other factors. Knowing these causes helps doctors diagnose and treat the condition.
Calculous Cholecystitis
Calculous cholecystitis is the most common type, making up 90-95% of cases. It happens when gallstones block the cystic duct, causing inflammation. This blockage leads to bile stasis and can cause bacterial infections.
Gallstones are a big risk for this type of cholecystitis. They form due to high cholesterol, bile stasis, and inflammation.
Acalculous Cholecystitis
Acalculous cholecystitis happens without gallstones, often in very sick patients. The exact causes are not fully understood but include bile stasis, ischemia, and infection. It’s very serious because it affects very ill patients.
Critical illness can lead to acalculous cholecystitis. This is due to fasting, total parenteral nutrition, and less gallbladder movement.
Other Causative Factors
Other things can also cause cholecystitis, like bacterial infection, chemical inflammation, and trauma. Sometimes, it’s caused by parasites or rare conditions.
In summary, cholecystitis has many causes. Knowing the differences between types and other factors is key to managing and treating it.
Clinical Presentation and Symptoms
Knowing the symptoms of cholecystitis is key for early treatment. Cholecystitis can cause a range of symptoms that affect a person’s life quality.
Cardinal Symptoms
The main symptoms of cholecystitis include severe pain in the upper right or center of the abdomen. This pain, called biliary colic, often starts after eating, and can be worse after fatty meals. It may also cause nausea and vomiting.
Key symptoms to watch for:
- Severe abdominal pain
- Nausea and vomiting
- Fever
- Abdominal tenderness
Physical Examination Findings
A physical exam of someone with cholecystitis shows tenderness in the right upper abdomen. Sometimes, a doctor can feel a mass, which means the gallbladder is inflamed.
| Signs | Frequency | Clinical Implication |
| Right upper quadrant tenderness | Common | Indicates gallbladder inflammation |
| Fever | Common | Suggests infection |
| Palpable mass | Less common | May indicate a gallbladder empyema or gangrene |
Presentation in Special Populations
In some groups, like the elderly or pregnant women, cholecystitis symptoms can be different. Elderly people might not show typical fever or pain. Pregnant women could have more severe symptoms because of pregnancy changes.
It’s important to recognize the different ways cholecystitis can show up for timely and effective treatment.
Diagnostic Approach and Evaluation
Diagnosing cholecystitis involves a detailed process. It combines lab tests and imaging results. This approach is key to accurately diagnosing and treating the condition.
Laboratory Values in Cholecystitis
Laboratory tests are essential in diagnosing cholecystitis. They show an elevated white blood cell count, which means there’s inflammation or infection. They also show abnormal liver enzymes, which can point to bile duct problems or liver issues.
Other important lab values include high bilirubin and alkaline phosphatase levels. The white blood cell count is very telling, as a big increase often means severe inflammation. Liver enzymes like ALT and AST might also be high, but they’re not specific to cholecystitis.
Imaging Techniques
Imaging studies are vital for diagnosing cholecystitis. The main tool is abdominal ultrasound. It can spot gallstones, gallbladder inflammation, and other signs of cholecystitis. Ultrasound is safe, easy to get, and very good at finding gallstones.
The HIDA scan (Hepatobiliary Iminodiacetic Acid scan) is another useful tool. It checks the gallbladder and bile ducts’ function and structure. A HIDA scan can show if the gallbladder isn’t filling up, which is a sign of cystic duct blockage and acute cholecystitis.
Diagnostic Criteria and Scoring Systems
There are several ways to diagnose cholecystitis. These methods use clinical findings, lab results, and imaging to guess if someone has cholecystitis.
The Tokyo Guidelines are a well-known system. They help doctors diagnose and figure out how severe cholecystitis is. These guidelines mix symptoms, lab results, and imaging to sort patients and decide on treatment.
By using lab tests, imaging, and clinical checks, doctors can accurately diagnose cholecystitis. This helps them create the right treatment plan.
Differential Diagnosis for Cholecystitis
Cholecystitis can look like many other conditions, both in the stomach and outside it. It’s key to figure out what’s really going on to treat it right.
Gastrointestinal Conditions
Some stomach problems can feel a lot like cholecystitis. These include:
- Peptic ulcer disease
- Pancreatitis
- Gastritis
- Hiatal hernia
- Hepatitis
Each one needs its own treatment plan. So, knowing exactly what’s wrong is very important.
| Condition | Key Characteristics |
| Peptic Ulcer Disease | Characterized by ulceration in the stomach or duodenum, often presenting with epigastric pain. |
| Pancreatitis | Inflammation of the pancreas, which can cause severe abdominal pain radiating to the back. |
| Gastritis | Inflammation of the gastric mucosa, potentially causing dyspepsia and abdominal pain. |
Non-Gastrointestinal Conditions
Some problems outside the stomach can also feel like cholecystitis. For example, a heart attack can cause pain in the upper belly.
- Myocardial infarction
- Pneumonia
- Pleurisy
It’s vital to think about these when trying to figure out what’s wrong. This helps avoid mistakes in diagnosis.
Management of Acute Cholecystitis
Managing acute cholecystitis involves both initial medical treatment and sometimes surgery to remove the gallbladder. A quick and thorough approach is key to avoid complications and improve patient health.
Initial Medical Management
First, patients are usually admitted to the hospital for close monitoring and treatment. They are advised to fast to rest the gallbladder. Intravenous fluids help keep them hydrated.
Intravenous antibiotics are also given to fight off likely infections. Pain management is important, with medicines used to ease symptoms.
The choice of antibiotics depends on the disease’s severity and local resistance patterns. In severe cases, broad-spectrum antibiotics are used to cover a wide range of pathogens.
Surgical Interventions
Surgical intervention is often needed for a complete cure of acute cholecystitis. The preferred method is laparoscopic cholecystectomy. It has the benefits of less pain, shorter hospital stays, and quicker recovery compared to open surgery.
The timing of surgery depends on several factors. These include the disease’s severity, patient health, and the surgeon’s expertise. Early surgery, usually within 72 hours, is recommended to lower the risk of complications.
Post-Treatment Care and Follow-up
After surgery, patients need careful post-treatment care to manage any complications and ensure a smooth recovery. This includes watching for signs of infection, managing pain, and gradually returning to normal activities and diet.
Follow-up care is vital to check on the patient’s recovery and address any concerns or complications. It’s also a chance to discuss preventive measures and lifestyle changes to lower the risk of future gallbladder disease.
Complications of Acute Cholecystitis
Acute cholecystitis can lead to both immediate and long-term problems. Knowing about these issues is key to better care and outcomes for patients.
Immediate Complications
Right away, acute cholecystitis can cause serious and even deadly issues. Gangrene and perforation of the gallbladder are among the most severe. Gangrene happens when the gallbladder doesn’t get enough blood, often because of a blockage. Perforation can cause peritonitis, a dangerous inflammation of the lining around the organs.
Sepsis is another urgent problem, caused by infection spreading through the blood. It needs quick treatment with antibiotics and supportive care.
Long-term Complications
Even after treatment, long-term issues can arise. Recurrent cholecystitis is a big worry, mainly if gallstones are not fixed. People who had acute cholecystitis are more likely to get chronic cholecystitis, with ongoing inflammation and scarring.
Other long-term problems include gallbladder fistula, an abnormal connection, and biliary cirrhosis, caused by long-term blockage of bile ducts.
It’s vital to understand these long-term risks. This shows why a full management plan, including surgery when needed, is important. It helps prevent more problems and reduces risks.
Conclusion
Cholecystitis is a serious condition that needs quick diagnosis and treatment. Knowing the causes, symptoms, and how to diagnose it is key to managing it well.
Managing cholecystitis effectively means acting fast to avoid serious problems. Early medical care and surgery can greatly help patients.
In conclusion, treating cholecystitis well requires a full plan of action. By spotting symptoms and risk factors early, doctors can give better care. This helps lower the chance of serious problems now and later.
Managing cholecystitis also means working together. Doctors and surgeons need to team up to give the best care possible to patients.
FAQ
What is acute cholecystitis?
Acute cholecystitis is when the gallbladder gets inflamed. This usually happens when gallstones block the cystic duct.
What are the risk factors for developing cholecystitis?
Being female, obese, pregnant, or from certain ethnic groups increases your risk. Also, having gallstones or gallbladder disease before can raise your risk.
How is cholecystitis diagnosed?
Doctors use lab tests and imaging to diagnose cholecystitis. Tests include checking white blood cell count and liver enzymes. Imaging like ultrasound and HIDA scan are also used.
What is the difference between calculous and acalculous cholecystitis?
Calculous cholecystitis is caused by gallstones. Acalculous cholecystitis is caused by other factors like bacterial infection or lack of blood flow.
What are the symptoms of cholecystitis?
Symptoms include abdominal pain, fever, and nausea. The severity and type of cholecystitis can affect the symptoms.
How is acute cholecystitis managed?
First, doctors may use antibiotics and pain relief. Then, surgery like cholecystectomy is often needed.
What are the possible complications of acute cholecystitis?
Complications include gangrene, perforation, and sepsis. These can be serious and even life-threatening if not treated quickly.
What is the role of imaging in diagnosing cholecystitis?
Imaging like ultrasound and HIDA scan is key. They help see gallstones, inflammation, and other signs of gallbladder disease.
Can cholecystitis be treated without surgery?
Some cases might be managed without surgery. But, surgery is often needed to avoid complications and fix the problem.
What is the pathophysiology of acute cholecystitis?
Acute cholecystitis involves blockages, chemical inflammation, and bacterial infections. If not treated, it can lead to serious damage like necrosis and perforation.
References
- Pietrangelo, A. (2024). Managing weight loss after gallbladder removal. Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/317659