Last Updated on November 27, 2025 by Bilal Hasdemir
Aortic stenosis is a serious condition where the heart’s aortic valve narrows. At Liv Hospital, we know how important it is to act fast. We offer care that is based on the latest research and focuses on the patient.
Recent updates in medicine show the need for good treatment options for aortic stenosis. This includes new procedures like TAVR. For mild cases, watching them closely might be enough. But for severe, symptomatic cases, immediate action is needed to save lives. We aim to give top-notch healthcare and support to patients from around the world.
Key Takeaways
- Timely intervention is key for managing aortic stenosis well.
- Advanced treatments like TAVR are suggested for severe cases.
- Liv Hospital offers internationally recognized, patient-centered care.
- Effective management strategies range from monitoring to mechanical interventions.
- Comprehensive support is available for international patients.
Understanding Aortic Stenosis and Its Clinical Impact
It’s important to understand how aortic stenosis affects patients. This heart disease can cause serious problems if not treated right. Knowing this helps find the best treatment for each patient.
The Pathophysiology of Aortic Valve Narrowing
Aortic stenosis happens when the aortic valve gets narrower. This blocks blood flow from the left ventricle to the aorta. It can be caused by calcification, birth defects, or rheumatic fever.
As the valve gets smaller, the heart has to work harder. This can lead to the heart muscle thickening and eventually, heart failure.
The disease affects the valve, the aortic root, and the left ventricle. Valve calcification makes the valve stiffer and less mobile.
Grading Severity: Mild, Moderate, and Severe
The severity of aortic stenosis is graded by the valve area, mean gradient, and peak jet velocity. Mild aortic stenosis might not need treatment right away. But severe aortic stenosis needs quick action. Knowing the exact grade helps decide the best treatment.
- Mild: Valve area > 1.5 cm², mean gradient
- Moderate: Valve area 1.0-1.5 cm², mean gradient 20-40 mmHg
- Severe: Valve area 40 mmHg
Symptoms and Life-Threatening Complications
Symptoms include chest pain, shortness of breath, and fainting. If not treated, severe aortic stenosis can cause heart failure, arrhythmias, and sudden death. It’s vital to catch these symptoms early.
Managing aortic stenosis means treating the valve and other heart problems. Sometimes, medication for aortic stenosis helps manage symptoms and slow the disease.
Why Prompt Intervention Matters in Aortic Stenosis
Aortic stenosis can cause serious health problems if not treated early. It happens when the aortic valve gets narrower, blocking blood flow. This can be life-threatening.
Natural History and Disease Progression
Aortic stenosis starts off mild but can get worse over time. At first, people might not feel any symptoms. But as it gets more severe, they may start to feel chest pain, have trouble breathing, and even faint.
It’s important to watch how the disease progresses. Doctors use echocardiograms and check-ups to see how bad it is. This helps them know when it’s time for surgery.
Survival Statistics Without Treatment
Patients with severe aortic stenosis are at high risk of dying if not treated. Research shows that once symptoms appear, their survival time is only about 2-3 years without surgery.
This highlights the need for quick action. Early treatment can save lives and improve quality of life.
Recognizing When to Escalate from Monitoring to Intervention
Knowing when to switch from watching the disease to taking action is key. Doctors make this decision based on symptoms, how bad the valve is, and the patient’s health.
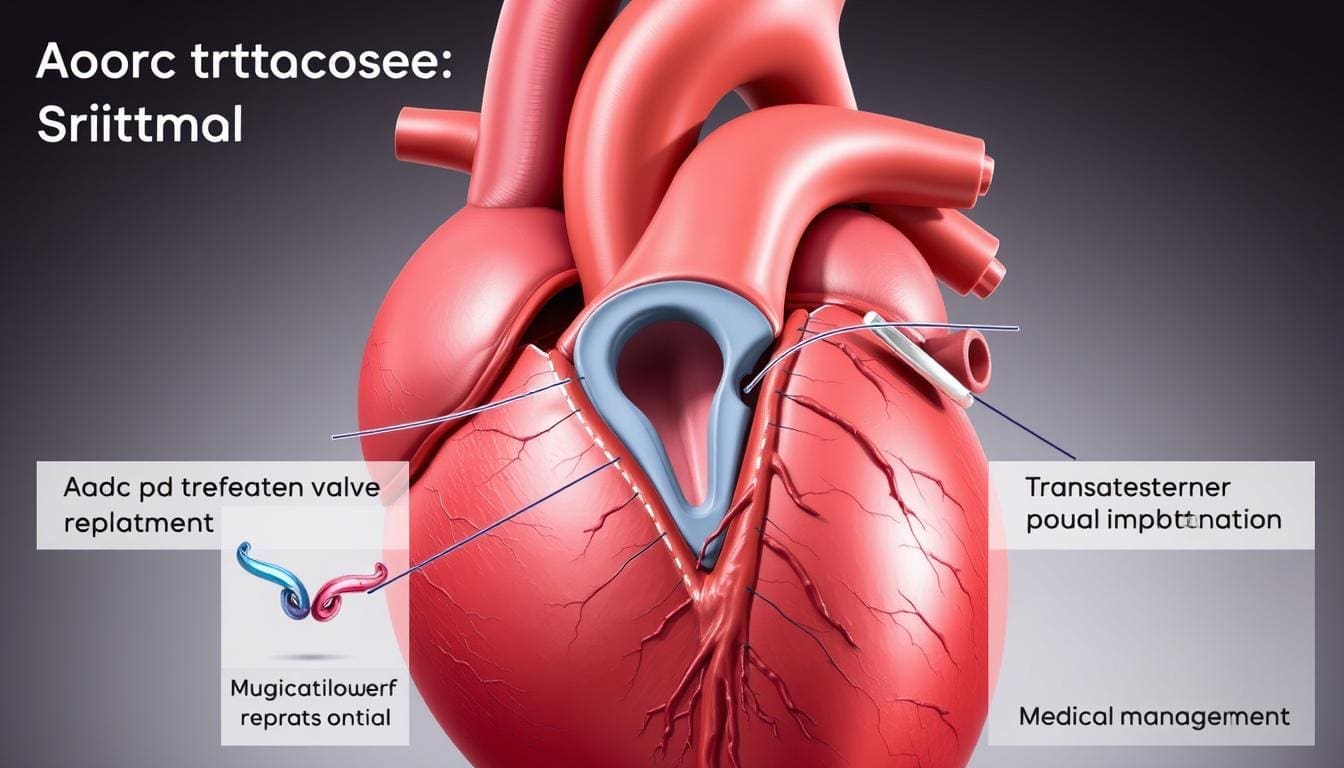
Surgical aortic valve replacement (SAVR) and transcatheter aortic valve replacement (TAVR) are two main treatments. The choice between them depends on the patient’s health, the valve’s shape, and what they prefer.
Understanding aortic stenosis, its effects without treatment, and when to act helps doctors give better care. This leads to better outcomes for patients.
Monitoring Strategy: Managing Mild Aortic Stenosis
Mild aortic stenosis needs regular checks to see how it’s changing. Many patients follow a watchful waiting plan. This balances the need for treatment with the risks of acting too soon.
Appropriate Candidates for Watchful Waiting
Those with mild aortic stenosis who don’t show symptoms are often watched closely. We keep an eye out for any signs of the disease getting worse or symptoms appearing.
Guidelines say regular echocardiograms are key for these patients. This test helps us see how bad the valve narrowing is and if it’s changing.
Echocardiography and Clinical Follow-up Protocols
Echocardiograms are done at set times to check on the aortic stenosis. How often depends on how severe it is and if symptoms are present.
| Aortic Stenosis Severity | Echocardiography Frequency | Clinical Follow-up |
|---|---|---|
| Mild | Every 2-3 years | Annual clinical assessment |
| Moderate | Every 1-2 years | Bi-annual clinical assessment |
| Severe | Every 6-12 months | Frequent clinical assessment as needed |
A leading reseacher says, “Regular check-ups are key in managing aortic stenosis. This way, we can act quickly if needed.”
“The key to managing mild aortic stenosis is careful monitoring and a proactive approach to addressing any changes in the patient’s condition.”
Lifestyle Modifications and Activity Recommendations
Patients with mild aortic stenosis are also advised to make lifestyle changes. This includes eating well, staying active, and not smoking.
We suggest talking to your doctor to create a plan that fits you. With a good management plan, patients with mild aortic stenosis can live well and avoid serious problems.
Surgical Aortic Valve Replacement (SAVR): The Traditional Gold Standard
For decades, SAVR has been the top choice for treating severe aortic stenosis. This method involves open-heart surgery to replace the aortic valve with a prosthetic one. It greatly improves patient outcomes.
Open-Heart Surgical Techniques and Approaches
SAVR is done through a sternotomy, giving surgeons direct heart access. Cardiopulmonary bypass keeps blood flowing and oxygen levels up during surgery. The choice between mechanical or biological valves depends on patient age, lifestyle, and anticoagulation needs.
Surgeons use various techniques to reduce trauma and speed up recovery. For example, some choose minimally invasive SAVR. The surgery takes 3 to 4 hours, with the patient under general anesthesia.
Mechanical vs. Biological Valve Prostheses
Choosing between mechanical and biological valves is key. Mechanical valves are durable but need lifelong anticoagulation therapy to prevent clotting. Biological valves have a shorter lifespan but don’t need long-term blood thinners, making them better for older patients or those who can’t take blood thinners.
“The choice of valve prosthesis should be individualized based on patient characteristics and preferences.”
Recovery Timeline and Rehabilitation
Recovery from SAVR takes about 5 to 7 days in the hospital. Patients are closely watched for any issues. After surgery, physical therapy helps regain strength and mobility. Most can return to normal activities in 3 months, but strenuous activities may be limited longer.
- Right after surgery, care focuses on pain management and preventing complications.
- Moving around early helps prevent blood clots.
- Regular check-ups are important to monitor valve function and heart health.
Long-term Outcomes and Survival Benefits
Research shows SAVR greatly improves survival and quality of life for those with severe aortic stenosis. Long-term results depend on the valve type, patient health, and following post-operative care.
Recent data indicates SAVR offers great long-term survival benefits. Some studies show survival rates similar to the general population.
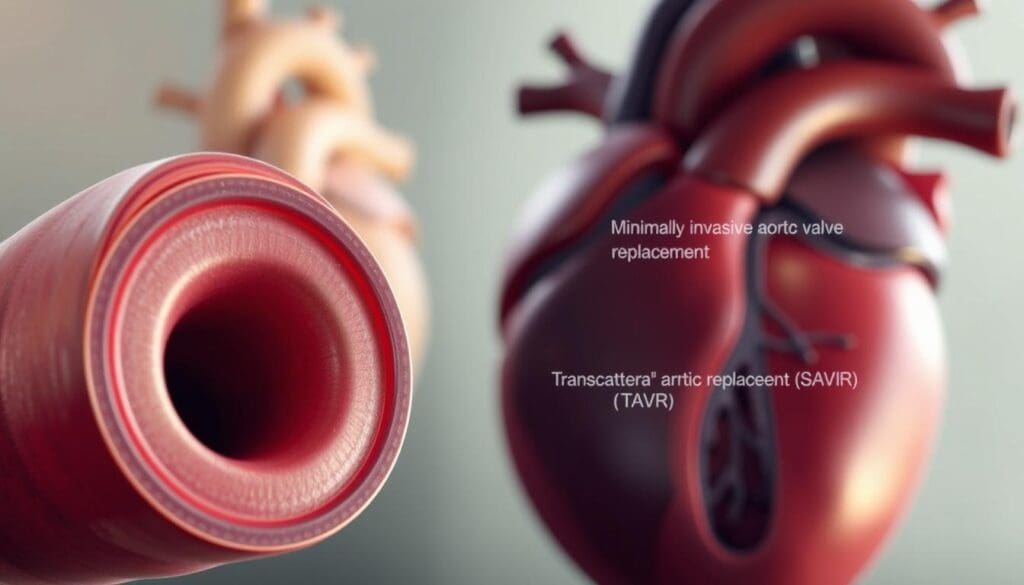
Transcatheter Aortic Valve Replacement (TAVR/TAVI): Minimally Invasive Revolution
TAVR has changed how we treat aortic stenosis. It’s a less invasive method that has made a big difference for patients with severe aortic stenosis.
Catheter-Based Procedure Techniques
TAVR uses a catheter to put a new valve in the heart. This method avoids open-heart surgery. It cuts down on recovery time and lowers the risk of problems.
We use special imaging to guide the catheter to the aortic valve. This ensures the new valve is placed correctly.
Key steps in the TAVR procedure include:
- Accessing the femoral artery
- Guiding the catheter to the heart
- Deploying the new valve
- Assessing valve function post-deployment
Comparative Advantages Over SAVR
TAVR is better than traditional Surgical Aortic Valve Replacement (SAVR) in many ways. It’s less invasive, causing less harm to the patient and leading to faster recovery. TAVR also lowers the risk of complications during surgery, which is a big plus for high-risk patients.
“TAVR has emerged as a viable alternative to SAVR, providing a less invasive option with similar results for many patients.” –
Expanding Indications: From High-Risk to Low-Risk Patients
At first, TAVR was only for patients at high or extreme risk for surgery. But now, studies show it’s safe and effective for lower-risk patients too. This means more people can benefit from TAVR.
Doctors are now treating patients earlier in their disease. This could lead to better long-term results. The data supports using TAVR for a wider range of patients, showing it can be as good as or better than SAVR.
Valve Durability and Long-term Results
There’s a big question about how long TAVR valves last. But, the latest data is promising. Modern TAVR devices seem to work well over time, helping patients feel better and live better lives.
Long-term outcomes after TAVR include:
| Outcome | 1-Year | 5-Year |
|---|---|---|
| Survival Rate | 85-90% | 60-70% |
| Valve Dysfunction | 10-15% |
As TAVR technology gets better, we’ll see even more improvements. Ongoing research and new device technology will be key in the future of treating aortic stenosis.
Balloon Aortic Valvuloplasty: Temporary Relief Option
Balloon aortic valvuloplasty is a non-surgical method for some aortic stenosis patients. It uses a balloon catheter to widen the narrowed aortic valve. This improves blood flow from the heart.
Procedure Details and Mechanism of Action
The procedure starts with a catheter inserted through a peripheral artery, usually the femoral artery. It’s guided to the heart. Then, a balloon is inflated at the aortic valve to widen it.
This action compresses the calcified leaflets, increasing the valve area. It reduces the blockage to blood flow. The goal is to improve blood flow and ease symptoms of severe aortic stenosis.
Limited Durability and High Restenosis Rates
Despite its benefits, balloon aortic valvuloplasty has limited durability and high restenosis rates in adults. Studies show symptoms often return within months to a year due to valve restenosis. This makes it less suitable as a long-term solution for most adults.
“The use of balloon aortic valvuloplasty as a standalone therapy is generally limited due to the high rate of restenosis and the need for repeat interventions.”
Role as Bridge Therapy in Critical Patients
In critical cases, balloon aortic valvuloplasty acts as a bridge therapy. It stabilizes patients who are too sick for immediate aortic valve replacement. It improves their condition, making them better candidates for more definitive treatments.
Pediatric Applications vs. Adult Limitations
In adults, balloon aortic valvuloplasty has significant limitations. But, it’s more effective and commonly used in children. In kids, the procedure can be a good option due to the different nature of congenital aortic stenosis. It allows the valve to grow with the child. In adults, the calcific degeneration is harder to treat with valvuloplasty alone.
Aortic Stenosis Therapy: Medical Management Approaches
Medical management is key in treating aortic stenosis, alongside surgery. It helps manage symptoms, treat related heart issues, and change risk factors.
Limitations of Medication in Reversing Valve Narrowing
Medicines can’t widen a narrowed aortic valve. So, medical care focuses on easing symptoms and slowing the disease’s growth.
Current Medical Management Strategies:
- Symptom management
- Heart failure medication
- Addressing cardiovascular comorbidities
- Risk factor modification
Symptom Management and Heart Failure Medications
Managing symptoms like chest pain and shortness of breath is vital. Beta-blockers and ACE inhibitors help by easing the heart’s work.
Diuretics help with fluid buildup and heart failure symptoms. Sometimes, medications that slow the heart or lower blood pressure are used.
Addressing Cardiovascular Comorbidities
Aortic stenosis often comes with other heart issues like high blood pressure and coronary disease. Treating these is important for overall health.
| Comorbidity | Management Strategy |
|---|---|
| Hypertension | Antihypertensive medications, lifestyle modifications |
| Coronary Artery Disease | Antiplatelet therapy, statins, lifestyle changes |
| Atrial Fibrillation | Anticoagulation therapy, rate control medications |
Risk Factor Modification Strategies
Changing risk factors is a big part of managing aortic stenosis. This includes diet, exercise, quitting smoking, and managing diabetes and high cholesterol.
With a full medical management plan, we can improve life quality for those with aortic stenosis. It may also slow the disease’s progress.
Experimental and Emerging Treatments on the Horizon
New treatments for aortic stenosis are being developed, giving hope for better care. These new methods could lead to better health outcomes for patients. Several promising therapies are being explored.
PCSK9 Inhibitors and Lipid-Lowering Therapies
PCSK9 inhibitors are showing great promise in lowering LDL cholesterol. This is important because high LDL cholesterol can worsen aortic stenosis. By blocking PCSK9, these treatments could slow the disease’s progression.
We are watching the results of clinical trials closely. This will help us understand how effective PCSK9 inhibitors are in treating aortic stenosis.
Lipoprotein(a) Reduction Approaches
Lipoprotein(a), or Lp(a), is linked to heart disease, including aortic stenosis. New treatments aim to lower Lp(a) levels. This could help prevent the disease from getting worse.
Calcium Metabolism Targeting Agents
Calcium buildup is a big part of aortic stenosis. New agents are being tested to control this buildup. They might slow or stop valve calcification, which could be a new way to manage the disease.
Current Clinical Trials and Research Status
Many clinical trials are looking at these new treatments for aortic stenosis. We are deeply involved in studying these therapies. This will help us understand their role in managing the disease.
As we get more data, we’ll know more about the future of treating aortic stenosis.
We are dedicated to leading in the field of aortic stenosis treatments. By exploring new therapies, we aim to give our patients the best care. This will help improve outcomes for those with aortic stenosis.
Post-Intervention Care: Lifelong Management Essentials
The journey doesn’t end with the treatment of aortic stenosis. Instead, it moves into ongoing care and monitoring. Effective post-intervention care is key for long-term success and patient health.
Structured Cardiology Follow-up Protocols
Regular visits with a cardiologist are vital. They help monitor the patient’s condition and the prosthetic valve’s function. These visits include echocardiography to check heart health.
We recommend sticking to the follow-up schedule. This helps catch any issues early.
Healthcare providers watch for complications like valve dysfunction and heart failure. They can adjust the treatment plan as needed.
Anticoagulation Management for Mechanical Valves
Patients with mechanical valves need lifelong anticoagulation therapy. This prevents valve thrombosis and thromboembolic events. It’s important to follow the prescribed regimen and have regular blood tests.
- Anticoagulation medications, such as warfarin, need to be taken as directed.
- Regular INR (International Normalized Ratio) monitoring is critical.
- Dietary adjustments may be necessary to maintain stable anticoagulation levels.
Endocarditis Prevention and Dental Considerations
Patients with prosthetic heart valves are at higher risk of infective endocarditis. We stress the importance of good oral hygiene and regular dental check-ups. Antibiotic prophylaxis before certain dental procedures may be recommended.
“The prevention of infective endocarditis is a critical aspect of post-intervention care for patients with prosthetic heart valves. Good oral hygiene practices and appropriate antibiotic prophylaxis are key components of this preventive strategy.”
Monitoring for Prosthetic Valve Complications
Prosthetic valves are designed to be durable but can face complications. We educate patients on signs and symptoms of issues like valve dysfunction and leakage. They should seek immediate medical attention if they notice any concerning symptoms.
By following these lifelong management essentials, patients can enjoy a better quality of life. Our team is committed to providing support throughout this journey.
Conclusion: Optimizing Outcomes in Aortic Stenosis Management
Managing aortic stenosis well needs a full plan. This includes acting fast, choosing the right treatment, and caring for patients over time. New ways to treat aortic stenosis, like TAVR and medical care, have made a big difference for patients.
We talked about different ways to treat aortic stenosis. This includes open-heart surgery and new treatments. It’s not just about picking a treatment. It’s also about following up with patients and managing other heart problems.
By using a wide range of strategies, we can make patients’ lives better. As new treatments come along, it’s important to keep learning and updating our care plans. This way, we can give patients with aortic stenosis the best care possible.
FAQ
What is aortic stenosis, and how is it diagnosed?
Aortic stenosis is a serious heart condition. It happens when the aortic valve gets narrower. Doctors use echocardiography and clinical checks to see how bad it is.
What are the treatment options for aortic stenosis?
Treatment depends on how bad the stenosis is. For mild cases, doctors might just watch and wait. For severe cases, they might do surgery or use a catheter to replace the valve.
How is mild aortic stenosis managed?
Mild cases are watched closely. Doctors use echocardiography and check in regularly. They also suggest lifestyle changes and what activities are safe.
What is the difference between SAVR and TAVR?
SAVR is open-heart surgery to replace the valve. TAVR is a less invasive procedure using a catheter. TAVR is safer for those at high risk for surgery.
Can medications cure aortic stenosis?
No, medicines can’t fix the valve narrowing. But, they help manage symptoms and other heart problems.
What is balloon aortic valvuloplasty, and when is it used?
This procedure uses a balloon to widen the valve. It’s used for urgent cases or when surgery isn’t an option right away.
What are the emerging treatments for aortic stenosis?
New treatments include PCSK9 inhibitors and ways to lower lipoprotein(a). These are being studied to help manage aortic stenosis.
What is involved in post-intervention care for aortic stenosis?
After treatment, care is lifelong. This includes regular cardiology visits, managing blood thinners, and watching for valve problems.
How can I manage my lifestyle with aortic stenosis?
Eating well, exercising, and not smoking are key. The right activities depend on how severe the stenosis is.
What are the benefits of timely intervention in aortic stenosis?
Early treatment can greatly improve life and survival chances. Knowing when to act is very important.
References
American Heart Association (AHA): Managing Aortic Stenosis Symptoms
PubMed (NCBI): Aortic Stenosis Progression (Specific PubMed ID)
AHA Journals (Circulation Research): Molecular Mechanisms in Aortic Stenosis (Specific DOI)
AHA Journals (Circulation): Specific Article on Cardiovascular Disease (Specific DOI)