Last Updated on November 26, 2025 by Bilal Hasdemir

Bowel death is a serious condition where the intestine cannot recover. It’s a medical emergency. Learn about bowel death, its main symptoms, causes, and available treatment options.
It usually happens when the intestine doesn’t get enough blood. This leads to tissue death. Knowing the causes and symptoms is key to quick treatment.
Problems like changes in bowel habits and blood in the stool are signs of trouble. They can lead to gangrenous colon or bowel infarction if not treated.
Key Takeaways
- Understanding bowel death is key to quick medical help.
- Not enough blood flow can cause tissue death, leading to bowel infarction.
- Symptoms include changes in bowel habits, blood in the stool, and abdominal pain.
- Quick treatment is vital to avoid serious issues.
- Liv Hospital offers top-notch, patient-centered care for gangrenous colon and bowel infarction.
What Is Bowel Death: Definition and Medical Significance

Bowel death is a serious medical issue where the intestines die off. It’s also called intestinal gangrene or gangrenous bowel. This happens when tissue decays and infections get severe, often needing surgery.
The Process of Intestinal Necrosis
Intestinal necrosis happens when the intestines don’t get enough blood. This can be due to many reasons l,,ike blocked blood vessels or inflammation. When the intestines die, they can let bacteria into the blood, leading to sepsis.
This condition can get worse fast, needing quick medical help. Early treatment is key to saving lives and improving health.
Prevalence and Mortality Statistics
Acute bowel infarction, linked to bowel death, affects up to 2 percent of people with sudden belly pain. Older people are more at risk due to blood vessel problems and other health issues.
Death rates from bowel death are high, showing the urgency of quick diagnosis and treatment. Knowing how common and deadly this condition is highlights the critical need for immediate medical care.
The Pathophysiology of Intestinal Gangrene
It’s important to understand how intestinal gangrene happens. This condition, also known as bowel infarction, occurs when the intestines don’t get enough blood. This leads to tissue death.
How Tissue Death Occurs in the Intestines
Tissue death in the intestines can happen for several reasons. These include vascular occlusion, infection, and inflammation. When blood flow is blocked, the tissue becomes ischemic. This causes cellular damage and eventually necrosis.
The process of intestinal necrosis is complex. It starts with a lack of blood flow, which means no oxygen or nutrients. This causes cellular injury. As it gets worse, inflammatory mediators and cellular pathways play a role in tissue deterioration.
Different Types of Bowel Infarction
Bowel infarction can be classified into different types. These depend on the cause and the extent of tissue damage. The main types include:
| Type | Description | Causes |
| Arterial Occlusion | Blockage of arterial blood flow to the intestines | Thrombosis, embolism |
| Venous Thrombosis | Clot formation in the veins draining blood from the intestines | Hypercoagulability, trauma |
| Non-occlusive Ischemia | Reduced blood flow without a physical blockage | Shock, heart failure |
Gangrenous intestine can develop due to vascular diseases, obstruction, or infections. Knowing these types helps doctors choose the right treatment.
Primary Causes of Bowel Death
Bowel death can happen due to several main reasons. It’s important to know and act on these causes quickly. This is key to managing and treating the condition effectively.
Vascular Occlusion and Ischemia
Vascular occlusion leads to ischemia, a major cause of bowel death. Ischemia happens when blood flow to the intestines stops or slows down. This is often because of blockages in arteries or veins. It’s vital to spot symptoms of gangrenous bowel like severe pain, fever, and quick worsening fast.
Doctors say ischemia can cause tissue death if not treated quickly. This shows why early action is so important.
Mechanical Obstruction
Mechanical obstruction is another main reason for bowel death. It happens when something blocks the intestines, stopping normal flow. This can be due to cancer treatment or the cancer itself.
Spotting it early is key to avoiding serious problems like bowel death.
Inflammatory Conditions
Inflammatory conditions like Crohn’s disease or ulcerative colitis can also cause bowel death. Long-term inflammation can harm the intestines, leading to necrosis.
Infectious Causes
Infections, such as severe peritonitis, can also lead to bowel death. These need quick medical care to avoid serious issues.
In summary, knowing the main causes of bowel death is vital for prevention and treatment. Spotting risk factors and symptoms early helps healthcare providers act fast. This can greatly reduce the risk of bowel death.
High-Risk Populations and Predisposing Factors
Knowing who is at high risk of bowel death is key to better treatment. Some groups face a higher chance of getting this serious condition.
Age-Related Risk Factors
Older adults are at a higher risk. This is because they might be less active, have vascular disease, or other health issues. Age-related decline in physical condition makes things worse.
Pre-existing Medical Conditions
People with diabetes, heart disease, or past surgeries are at risk. Chronic conditions make it harder to diagnose and treat.
Lifestyle and Environmental Factors
Smoking and not being active increase the risk. Also, how easy it is to get healthcare matters a lot.
- Smoking
- Sedentary lifestyle
- Poor dietary habits
Studies show that not catching bowel cancer early can lead to more deaths. For example, older adults and Black people in the U.S. face a higher risk of colon cancer. This can turn deadly if not treated quickly.
Recognizing Gangrenous Bowel Symptoms
It’s key to know the signs of gangrenous bowel to avoid serious issues. Gangrene in the bowel is rare but deadly. It needs quick medical care.
Early Warning Signs
The first signs of gangrenous bowel can be tricky to spot. Look out for severe abdominal pain that doesn’t match the physical check. Also, watch for vomiting. Some might feel abdominal tenderness and fever.
Advanced Symptoms of Bowel Gangrene
As gangrene gets worse, symptoms get more serious. Look for bloody stools, septic shock, and multi-organ failure. Spotting these signs early is vital.
Symptom Progression Timeline
The time it takes for symptoms to get worse can vary. It often happens fast, in hours or days. Knowing this helps doctors act quickly.
Spotting gangrenous bowel symptoms early can save lives. Knowing the signs helps people get help fast. This can stop serious problems.
Diagnostic Approaches for Gangrenous Intestine
Diagnosing gangrenous intestine involves several steps. These include clinical assessment, lab tests, and imaging. Quick diagnosis is key to treating the condition and saving lives.
Clinical Evaluation and Physical Examination
First, doctors do a thorough check-up. They look at your medical history and do a physical exam. They check for signs like severe pain, tenderness, and muscle tension in the abdomen. These signs can point to bowel problems.
Laboratory Tests and Biomarkers
Lab tests are important for diagnosis. Blood tests can show high white blood cell counts, which means infection or inflammation. Other tests can hint at tissue death. While no one test is sure, a mix can help doctors diagnose.
Imaging Techniques
Imaging is key to confirming the diagnosis. Computed Tomography (CT) scans are very helpful. They can show signs like bowel wall thickening and gas in the bowel wall. This means bowel gangrene. Other tools like ultrasound and X-rays might also be used, but they’re not as good for this.
By using all these methods, doctors can quickly and accurately diagnose. This is vital for starting the right treatment.
Emergency Medical Interventions for Infarcted Bowel
Emergency medical care is key in treating an infarcted bowel. It helps prevent more problems. Quick action is needed to keep the patient stable and fix the root cause.
Initial Stabilization Measures
The first thing to do is stabilize the patient. This means checking the patient’s overall condition. We look at vital signs and lab results to see how bad it is.
Fluid Resuscitation and Antibiotic Therapy
Fluid resuscitation is vital to keep blood flowing to important organs. Antibiotic therapy is started to fight off bacteria that might spread through the damaged bowel.
| Treatment Component | Description | Clinical Benefit |
| Fluid Resuscitation | Restoring circulating volume | Maintains perfusion of vital organs |
| Antibiotic Therapy | Covering bacterial translocation | Reduces risk of sepsis |
Pain Management Strategies
Managing pain is very important for patients with an infarcted bowel. We use opioid analgesics and other methods to keep them comfortable.
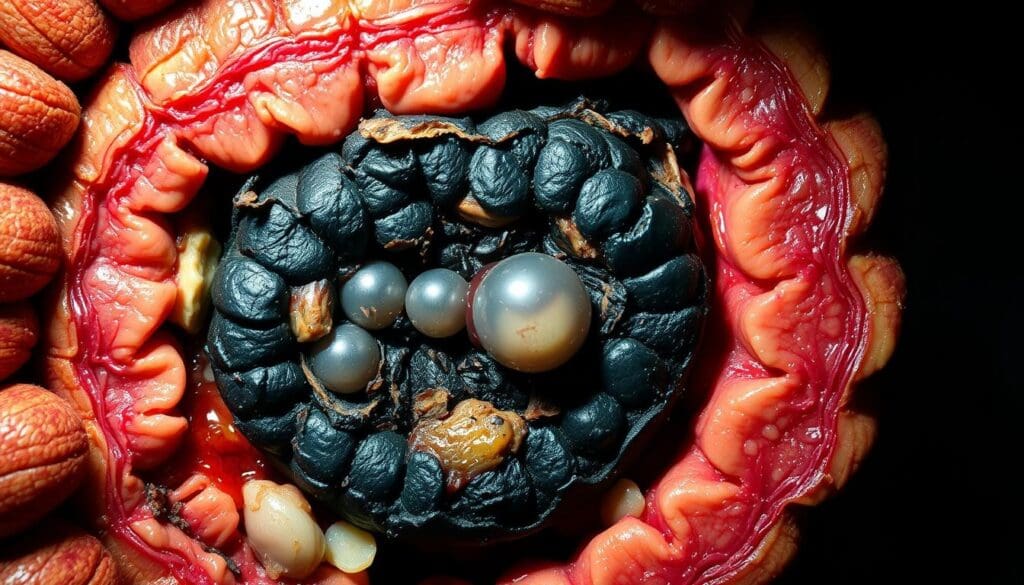
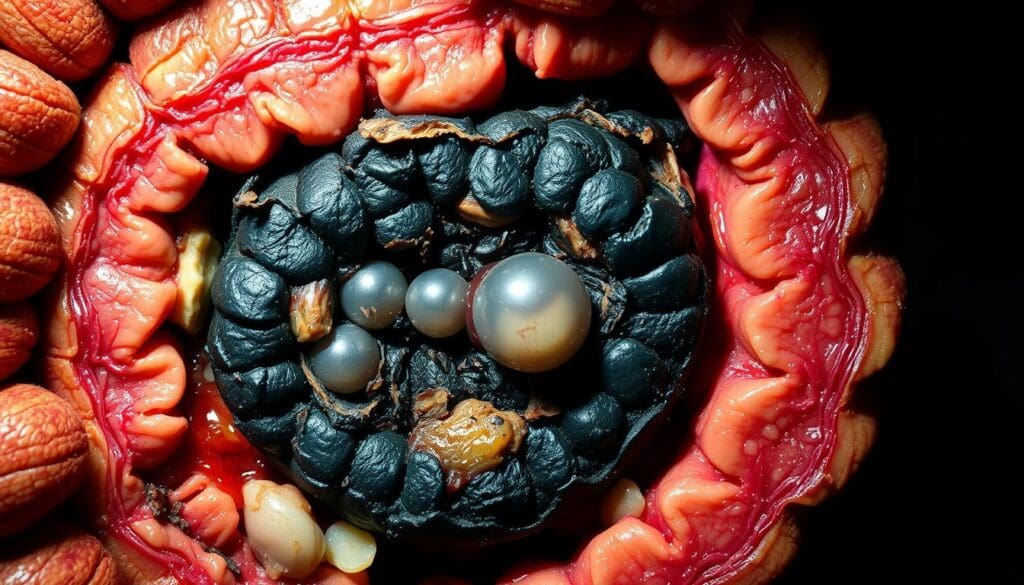
Surgical Treatment Options for Gangrene of the Bowel
Gangrene in the bowel needs surgery to remove dead tissue and fix the intestine. Surgery is key to treating gangrene of the bowel. Different methods are used, depending on the gangrene’s size and location.
Resection Procedures
Resection means cutting out the gangrenous part of the bowel. This stops gangrene from spreading. The surgeon then connects the healthy parts of the bowel, if it’s possible.
Revascularization Techniques
Revascularization helps blood flow back to the affected area. It might involve bypassing a blocked blood vessel or removing the blockage. This method tries to save as much intestine as possible and keep it working.
Ostomy Creation and Management
An ostomy might be needed if the gangrene is too big or if reconnecting the bowel is not possible. This creates an opening in the abdomen to collect feces in a bag. Taking care of an ostomy is important and requires patient education and support.
Minimally Invasive Approaches
Minimally invasive surgery, like laparoscopy, is sometimes used for gangrenous bowel. These methods can make recovery faster and leave less scarring. But they depend on one case and the surgeon’s skills.
| Surgical Technique | Description | Benefits |
| Resection | Prevents the spread of gangrene | Prevents spread of gangrene |
| Revascularization | Restoration of blood flow | Salvages intestinal function |
| Ostomy Creation | Diverts fecal flow | Manages extensive gangrene |
| Minimally Invasive Surgery | Less invasive surgical techniques | Reduces recovery time |
Treating gangrene of the bowel with surgery is complex. It needs a plan that fits the patient’s situation and the gangrene’s size. Knowing the surgical options is key to good management and recovery.
Post-Surgical Care and Recovery Process
Good post-surgical care is key to avoiding problems after bowel gangrene surgery. The recovery journey has many important steps. Both healthcare teams and patients must pay close attention to these.
Immediate Post-Operative Management
Right after surgery, care focuses on keeping the patient stable and managing pain. This means watching vital signs and giving the right pain meds.
Long-term Recovery Considerations
Long-term recovery includes regular check-ups to see how healing is going. Patients also learn about lifestyle changes to avoid future issues.
Nutritional Support and Rehabilitation
Eating right is vital for getting better. A diet full of proteins, vitamins, and minerals is best.
| Care Aspect | Description | Importance |
| Immediate Post-Operative Management | Stabilizing the patient, pain management | High |
| Long-term Recovery Considerations | Follow-up appointments, lifestyle changes | High |
| Nutritional Support | Balanced diet for healing | Critical |
Complications and Long-Term Consequences of Gangrenous Colon
It’s important to know the complications of gangrenous colon to manage patients well. This serious condition causes tissue death in the colon. If not treated quickly, it can lead to serious health issues.
Short-Term Complications
Short-term issues include infection, sepsis, and organ failure. These problems can happen fast and need quick medical help. For example, an infection can quickly turn into sepsis, a dangerous condition.
Long-Term Health Implications
The long-term effects of gangrenous colon are serious. Patients might face chronic pain, malabsorption, and reduced bowel function. They could also deal with long-term mental health issues like anxiety and depression.
Quality of Life Considerations
Patients with gangrenous colon may see their quality of life drop. They might need ostomy care, have changes in bowel habits, and face long-term disabilities. These can make it hard for them to live normally again.
Prevention Strategies and Risk Reduction
Preventing bowel death starts with proactive steps. Managing health conditions and regular check-ups are key. By knowing the risks and taking action, you can lower your chance of getting this condition.
Managing Underlying Conditions
Controlling health issues is critical. Conditions like heart disease, diabetes, and high blood pressure need attention. Managing these can greatly lower the risk of bowel problems.
Lifestyle Modifications
A healthy lifestyle is essential. Eat foods high in fiber, exercise, don’t smoke, and drink less alcohol. These habits not only prevent bowel death but also boost your overall health.
Regular Medical Monitoring for High-Risk Patients
High-risk individuals need regular doctor visits. These check-ups help spot bowel problems early.
Conclusion: The Critical Importance of Early Intervention
Early intervention is key to better outcomes for patients with bowel death. Quick medical action can greatly lower death rates from gangrenous colon.
It’s vital to diagnose and treat early. Studies show early treatment of colon issues boosts survival chances. This highlights the need for quick action and awareness.
Knowing the causes, signs, and treatments for bowel death helps people get medical help fast. This could save lives. Doctors must also watch for high-risk patients and take steps to prevent problems.
In the end, early action is the best way to handle bowel death. It’s important for everyone to know the risks and act quickly.
FAQ
What is bowel death, and how does it occur?
Bowel death, also known as intestinal gangrene or bowel infarction, happens when the intestines don’t get enough blood. This can cause tissue to die. It can be caused by many things, like blocked blood vessels, mechanical blockages, inflammation, and infections.
What are the primary causes of bowel death?
The main causes of bowel death are blocked blood vessels and not enough blood flow, mechanical blockages, inflammation, and infections. These issues can lead to the intestines not getting enough blood, causing tissue death.
Who is at high risk for developing bowel death?
Older adults, people with heart disease, and those who have had bowel surgery or have inflammatory bowel disease are at higher risk. Smoking and a sedentary lifestyle can also increase the risk.
What are the symptoms of gangrenous bowel?
Symptoms of gangrenous bowel include abdominal pain, nausea, vomiting, and fever. More severe symptoms are severe abdominal tenderness, bloody stools, and signs of shock. It’s important to recognize these symptoms early for timely medical help.
How is gangrenous intestine diagnosed?
Diagnosing gangrenous intestine involves clinical evaluation, lab tests, and imaging. A healthcare provider will assess symptoms, perform a physical exam, and may order blood work, CT scans, or X-rays to confirm the diagnosis.
What are the treatment options for gangrene of the bowel?
Treatment for gangrene of the bowel includes emergency care like fluid resuscitation, antibiotics, and pain management. Surgery, like resection procedures, revascularization, and ostomy creation, may also be needed.
What is the recovery process like after surgery for bowel death?
Recovery after surgery for bowel death involves immediate care, long-term recovery, and nutritional support. Patients need to follow a specific care plan to ensure a smooth recovery and avoid complications.
Can bowel death be prevented?
While some risks for bowel death can’t be avoided, taking proactive steps can help. Managing health conditions, making lifestyle changes, and regular medical check-ups can reduce the risk or detect it early.
What are the complications and long-term consequences of gangrenous colon?
Complications of gangrenous colon include short-term issues like infection and organ failure, and long-term health problems like chronic digestive issues and reduced quality of life. Prompt treatment and care can help manage these consequences.
What is the importance of early intervention in managing bowel death?
Early intervention is key in managing bowel death. Timely medical action can greatly improve outcomes. Recognizing symptoms, quick diagnosis, and effective treatment can reduce complications and improve survival rates.
What is colonic infarction?
Colonic infarction occurs when colon tissue dies due to a lack of blood supply. It’s a type of bowel death and can be caused by blocked blood vessels and ischemia.
What are the symptoms of an infarcted bowel?
Symptoms of an infarcted bowel include severe abdominal pain, nausea, vomiting, and fever. It’s important to recognize these symptoms early for timely medical help.
Bowel death is a serious condition where the intestine cannot recover. It’s a medical emergency.
It usually happens when the intestine doesn’t get enough blood. This leads to tissue death. Knowing the causes and symptoms is key to quick treatment..
Problems like changes in bowel habits and blood in the stool are signs of trouble. They can lead to gangrenous colon or bowel infarction if not treated.
Key Takeaways
- Understanding bowel death is key to medical help.
- Not enough blood flow can cause tissue death, leading to bowel infarction.
- Symptoms include changes in bowel habits, blood in the stool, and abdominal pain.
- Quick treatment is vital to avoid serious issues.
- Liv Hospital offers top-notch, patient-centered care for gangrenous colon and bowel infarction.
What Is Bowel Death: Definition and Medical Significance

Bowel death is a serious medical issue where the intestines die off. It’s also called intestinal gangrene or gangrenous bowel. This happens when tissue decays and infections get severe, often needing surgery.
The Process of Intestinal Necrosis
Intestinal necrosis happens when the intestines don’t get enough blood. This can be due to many reasons, blocked blood vessels or inflammation. When the intestines die, they can let bacteria into the blood, leading to sepsis.
This condition can get worse fast, needing quick medical help. Early treatment is key to saving lives and improving health.
Prevalence and Mortality Statistics
Acute bowel infarction, linked to bowel death, affects up to 2 percent of people with sudden belly pain. Older people are more at risk due to blood vessel problems and other health issues.
Death rates from bowel death are high, showing the urgency of quick diagnosis and treatment. Knowing how common and deadly this condition is highlights the critical need for immediate medical care.
The Pathophysiology of Intestinal Gangrene
It’s important to understand how intestinal gangrene happens. This condition, also known as bowel infarction, occurs when the intestines don’t get enough blood. This leads to tissue death.
How Tissue Death Occurs in the Intestines
Tissue death in the intestines can happen for several reasons. These include vascular occlusion, infection, and inflammation. When blood flow is blocked, the tissue becomes ischemic. This causes cellular damage and eventually necrosis.
The process of intestinal necrosis is complex. It starts with a lack of blood flow, which means no oxygen or nutrients. This causes cellular injury. As it gets worse, inflammatory mediators and cellular pathways play a role in tissue deterioration.
Different Types of Bowel Infarction
Bowel infarction can be classified into different types. These depend on the cause and the extent of tissue damage. The main types include:
| Type | Description | Causes |
| Arterial Occlusion | Blockage of arterial blood flow to the intestines | Thrombosis, embolism |
| Venous Thrombosis | Clot formation in the veins draining blood from the intestines | Hypercoagulability, trauma |
| Non-occlusive Ischemia | Reduced blood flow without a physical blockage | Shock, heart failure |
Gangrenous intestine can develop due to vascular diseases, obstruction, or infections. Knowing these types helps doctors choose the right treatment.
Primary Causes of Bowel Death
Bowel death can happen due to several main reasons. It’s important to know and act on these causes quickly. This is key to managing and treating the condition effectively.
Vascular Occlusion and Ischemia
Vascular occlusion leads to ischemia, a major cause of bowel death. Ischemia happens when blood flow to the intestines stops or slows down. This is often because of blockages in arteries or veins. It’s vital to spot symptoms of gangrenous bowel like severe pain, fever, and quick worsening fast.
Doctors say ischemia can cause tissue death if not treated quickly. This shows why early action is so important.
Mechanical Obstruction
Mechanical obstruction is another main reason for bowel death. It happens when something blocks the intestines, stopping normal flow. This can be due to cancer treatment or the cancer itself.
Spotting it earlearliavoidsious problems like bowel death.
Inflammatory Conditions
Inflammatory conditions like Crohn’s disease or ulcerative colitis can also cause bowel death. Long-term inflammation can harm the intestines, leading to necrosis.
Infectious Causes
Infections, such as severe peritonitis, can also lead to bowel death. These need quick medical care to avoid serious issues.
In summary, knowing the main causes of bowel death is vital for prevention and treatment. Spotting risk factors and symptoms early helps healthcare providers act fast. This can greatly reduce the risk of bowel death.
High-Risk Populations and Predisposing Factors
Knowing who is at high rof bowel death is key to better treatment. Some groups face a higher chance of getting this serious condition.
Age-Related Risk Factors
Older adults are at a higher risk. This is because they might be less active, have vascular disease, or other health issues. Age-related decline in physical condition makes things worse.
Pre-existing Medical Conditions
People with diabetes, heart disease, or past surgeries are at risk. Chronic conditions make it harder to diagnose and treat.
Lifestyle and Environmental Factors
Smoking and not being active increase the risk. Also, how easy it is to get healthcare matters a lot.
- Smoking
- Sedentary lifestyle
- Poor dietary habits
Studies show that not catching bowel cancer early can lead to more deaths. For example, older adults and Black people in the U.S. face a higher risk of colon cancer. This can turn deadly if not treated quickly.
Recognizing Gangrenous Bowel Symptoms
It’s key to know the signs of gangrenous bowel to avoid serious issues. Gangrene in the bowel is rare but deadly. It needs quick medical care.
Early Warning Signs
The first signs of gangrenous bowel can be tricky to spot. Look out for severe abdominal pain that doesn’t match the physical check. Also, watch for vomiting. Some might feel abdominal tenderness and fever.
Advanced Symptoms of Bowel Gangrene
As gangrene gets worse, symptoms get more serious. Look for bloody stools, septic shock, and multi-organ failure. Spotting these signs early is vital.
Symptom Progression Timeline
The time it takes for symptoms to get worse can vary. It often happens fast, in hours or days. Knowing this helps doctors act quickly.
Spotting gangrenous bowel symptoms early can save lives. Knowing the signs helps people get help fast. This can stop serious problems.
Diagnostic Approaches for Gangrenous Intestine
Diagnosing gangrenous intestine involves several steps. These include clinical assessment, lab tests, and imaging. Quick diagnosis is key to treating the condition and saving lives.
Clinical Evaluation and Physical Examination
First, doctors do a thorough check-up. They look at your medical history and do a physical exam. They check for signs like severe pain, tenderness, and muscle tension in the abdomen. These signs can point to bowel problems.
Laboratory Tests and Biomarkers
Lab tests are important for diagnosis. Blood tests can show high white blood cell counts, which means infection or inflammation. Other tests can hint at tissue death. While no one test is sure, a mix can help doctors diagnose.
Imaging Techniques
Imaging is key to confirming the diagnosis. Computed Tomography (CT) scans are very helpful. They can show signs like bowel wall thickening and gas in the bowel wall. This means bowel gangrene. Other tools like ultrasound and X-rays might also be used, but they’re not as good for this.
By using all these methods, doctors can quickly and accurately diagnose. This is vital for starting the right treatment.
Emergency Medical Interventions for Infarcted Bowel
Emergency medical care is key in trtreatingannfarcted bowel. It helps prevent more problems. Quick action is needed to keep the patient stable and fix the root cause.
Initial Stabilization Measures
The first thing to do is stabilize the patient. This means checking the patient’s overall condition. We look at vital signs and lab results to see how bad it is.
Fluid Resuscitation and Antibiotic Therapy
Fluid resuscitation is vital to keep blood flowing to important organs. Antibiotic therapy is started to fight off bacteria that might spread through the damaged bowel.
| Treatment Component | Description | Clinical Benefit |
| Fluid Resuscitation | Restoring circulating volume | Maintains perfusion of vital organs |
| Antibiotic Therapy | Covering bacterial translocation | Reduces risk of sepsis |
Pain Management Strategies
Managing pain is very important for patients with an infarcted bowel. We use opioid analgesics and other methods to keep them comfortable.
Surgical Treatment Options for Gangrene of the Bowel
Gangrene in the bowel needs surgery to remove dead tissue and fix the intestine. Surgery is key to treating gangrene of the bowel. Different methods are used, depending on the gangrene’s size and location.
Resection Procedures
Resection means cutting out the gangrenous part of the bowel. This stops gangrene from spreading. The surgeon then connects the healthy parts of the bowel, if it’s possible.
Revascularization Techniques
Revascularization helps blood flow back to the affected area. It might involve bypassing a blocked blood vessel or removing the blockage. This method tries to save as much intestine as possible and keep it working.
Ostomy Creation and Management
An ostomy might be needed if the gangrene is too big or if reconnecting the bowel is not possible. This creates an opening in the abdomen to collect feces in a bag. Taking care of an ostomy is important and requires patient education and support.
Minimally Invasive Approaches
Minimally invasive surgery, like laparoscopy, is sometimes used for gangrenous bowel. These methods can make recovery faster and leave less scarring. But they depend on the case and the surgeon’s skills.
| Surgical Technique | Description | Benefits |
| Resection | Prevents the spread of gangrene | Prevents spread of gangrene |
| Revascularization | Restoration of blood flow | Salvages intestinal function |
| Ostomy Creation | Diverts fecal flow | Manages extensive gangrene |
| Minimally Invasive Surgery | Less invasive surgical techniques | Reduces recovery time |
Treating gangrene of the bowel with surgery is complex. It needs a plan that fits the patient’s situation and the gangrene’s size. Knowing the surgical options is key to good management and recovery.
Post-Surgical Care and Recovery Process
Good post-surgical care is key to avoiding problems after bowel gangrene surgery. The recovery journey has many important steps. Both healthcare teams and patients must pay close attention to these.
Immediate Post-Operative Management
Right after surgery, care focuses on keeping the patient stable and managing pain. This means watching vital signs and giving the right pain meds.
Long-term Recovery Considerations
Long-term recovery includes regular check-ups to see how healing is going. Patients also learn about lifestyle changes to avoid future issues.
Nutritional Support and Rehabilitation
Eating right is vital for getting better. A diet full of proteins, vitamins, and minerals is best.
| Care Aspect | Description | Importance |
| Immediate Post-Operative Management | Stabilizing the patient, pain management | High |
| Long-term Recovery Considerations | Follow-up appointments, lifestyle changes | High |
| Nutritional Support | Balanced diet for healing | Critical |
Complications and Long-Term Consequences of Gangrenous Colon
It’s important to know the complications of gangrenous colon to manage patients well. This serious condition causes tissue death in the colon. If not treated quickly, it can lead to serious health issues.
Short-Term Complications
Short-term issues include infection, sepsis, and organ failure. These problems can happen fast and need quick medical help. For example, an infection can quickly turn into sepsis, a dangerous condition.
Long-Term Health Implications
The long-term effects of gangrenous colon are serious. Patients might face chronic pain, malabsorption, and reduced bowel function. They could also deal with long-term mental health issues like anxiety and depression.
Quality of Life Considerations
Patients with gangrenous colon may see their quality of life drop. They might need ostomy care, have changes in bowel habits, and face long-term disabilities. These can make it hard for them to live normally again.
Prevention Strategies and Risk Reduction
Preventing bowel death starts with proactive steps. Managing health conditions and regular check-ups are key. By knowing the risks and taking action, you can lower your chance of getting this condition.
Managing Underlying Conditions
Controlling health issues is critical. Conditions like heart disease, diabetes, and high blood pressure need attention. Managing these can greatly lower the risk of bowel problems.
Lifestyle Modifications
A healthy lifestyle is essential. Eat foods high in fiber, exercise, don’t smoke, and drink less alcohol. These habits not only prevent bowel death but also boost your overall health.
Regular Medical Monitoring for High-Risk Patients
High-risk individuals need regular doctor visits. These check-ups help spot bowel problems early.
Conclusion: The Critical Importance of Early Intervention
Early intervention is key to better outcomes for patients with bowel death. Quick medical action can greatly lower death rates from gangrenous colon.
It’s vital to diagnose and treat early. Studies show early treatment of colon issues boosts survival chances. This highlights the need for quick action and awareness.
Knowing the causes, signs, and treatments for bowel death helps people get medical help fast. This could save lives. Doctors must also watch for high-risk patients and take steps to prevent problems.
In the end, early action is the best way to handle bowel death. It’s important for everyone to know the risks and act quickly.
FAQ
What is bowel death, and how does it occur?
Bowel death, also known as intestinal gangrene or bowel infarction, happens when the intestines don’t get enough blood. This can cause tissue to die. It can be caused by many things, like blocked blood vessels, mechanical blockages, inflammation, and infections.
What are the primary causes of bowel death?
The main causes of bowel death are blocked blood vessels and not enough blood flow, mechanical blockages, inflammation, and infections. These issues can lead to the intestines not getting enough blood, causing tissue death.
Who is at high risk for developing bowel death?
Older adults, people with heart disease, and those who have had bowel surgery or have inflammatory bowel disease are at higher risk. Smoking and a sedentary lifestyle can also increase the risk.
What are the symptoms of gangrenous bowel?
Symptoms of gangrenous bowel include abdominal pain, nausea, vomiting, and fever. More severe symptoms are severe abdominal tenderness, bloody stools, and signs of shock. It’s important to recognize these symptoms early for timely medical help.
How is gangrenous intestine diagnosed?
Diagnosing gangrenous intestine involves clinical evaluation, lab tests, and imaging. A healthcare provider will assess symptoms, perform a physical exam, and may order blood work, CT scans, or X-rays to confirm the diagnosis.
What are the treatment options for gangrene of the bowel?
Treatment for gangrene of the bowel includes emergency care like fluid resuscitation, antibiotics, and pain management. Surgery, like resection procedures, revascularization, and ostomy creation, may also be needed.
What is the recovery process like after surgery for bowel death?
Recovery after surgery for bowel death involves immediate care, long-term recovery, and nutritional support. Patients need to follow a specific care plan to ensure a smooth recovery and avoid complications.
Can bowel death be prevented?
While some risks for bowel death can’t be avoided, taking proactive steps can help. Managing health conditions, making lifestyle changes, and regular medical check-ups can reduce the risk or detect it early.
What are the complications and long-term consequences of gangrenous colon?
Complications of gangrenous colon include short-term issues like infection and organ failure, and long-term health problems like chronic digestive issues and reduced quality of life. Prompt treatment and care can help manage these consequences.
What is the importance of early intervention in managing bowel death?
Early intervention is key in managing bowel death. Timely medical action can greatly improve outcomes. Recognizing symptoms, quick diagnosis, and effective treatment can reduce complications and improve survival rates.
What is colonic infarction?
Colonic infarction occurs when colon tissue dies due to a lack of blood supply. It’s a type of bowel death and can be caused by blocked blood vessels and ischemia.
What are the symptoms of an infarcted bowel?
Symptoms of an infarcted bowel include severe abdominal pain, nausea, vomiting, and fever. It’s important to recognize these symptoms early for timely medical help.
References
- Dahmiwal, T., et al. (2024). Dietary considerations in cholecystectomy. Journal of Gastrointestinal Surgery, 28(5), 345-350. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11200314/