Last Updated on November 27, 2025 by Bilal Hasdemir

Angina pectoris is a condition where you feel chest pain or discomfort. This happens because your heart doesn’t get enough oxygen-rich blood. It’s a sign of a bigger problem with your heart’s blood flow.
This condition often means there’s a heart issue. Knowing its symptoms, medical definition, and causes is key to treating it right. At Liv Hospital, we focus on our patients to diagnose and manage angina pectoris. We aim to give our patients the best care possible.
Key Takeaways
- Angina pectoris is a symptom of coronary artery disease.
- It is characterized by chest pain or discomfort due to reduced blood flow to the heart.
- Understanding its symptoms, medical definition, and causes is critical for proper diagnosis and treatment.
- Liv Hospital uses a patient-centered, multidisciplinary approach to diagnose and manage angina pectoris.
- Early diagnosis and treatment are vital for managing the condition and preventing further complications.
Understanding Angina Pectoris: A Complete Overview
Angina pectoris is a condition that causes chest pain or discomfort. It happens when the heart muscle doesn’t get enough oxygen-rich blood. This is a sign of coronary artery disease.
The Medical Definition of Angina Pectoris
Angina pectoris is a condition with episodes of chest pain or discomfort. It usually happens when you exert yourself or feel stressed. Resting or taking nitroglycerin can help relieve the pain.
The pain feels like a heavy or squeezing sensation. A medical expert says, “Angina pectoris is a symptom that warns of an imbalance between myocardial oxygen supply and demand.“
The term “angina pectoris” comes from Latin. “Angina” means “to choke” and “pectoris” means chest. So, it’s literally a choking sensation in the chest.
How Common Is Angina Pectoris?
Angina pectoris affects millions of people worldwide. It becomes more common with age and in those with heart disease risk factors. Every year, millions are diagnosed, showing the need for awareness and treatment.
As a health report states, “
Angina pectoris is a significant health issue globally, necessitating complete management strategies to lessen its impact on quality of life and mortality.
“
Types of Angina Pectoris
It’s important to know the different types of angina pectoris for proper treatment. Angina pectoris is chest pain or discomfort due to temporary heart muscle ischemia. It’s not just one thing but several types, each with its own traits and care needs.
Stable Angina: The Predictable Pattern
Stable angina is the most common type. It happens when you exert yourself or get stressed, and goes away with rest or medicine. The pain is usually the same every time you do the same thing. Stable angina shows you have coronary artery disease. To manage it, you need to change your lifestyle and might need medicine to lessen the pain.
Unstable Angina: A Medical Emergency
Unstable angina is more serious and can mean a heart attack is coming. It causes chest pain without warning, even when you’re not doing anything. This type of angina gets worse over time. It’s a medical emergency because it means you’re at high risk of a heart attack. You need to see a doctor right away to prevent a heart attack.
Variant (Prinzmetal’s) Angina
Variant angina, or Prinzmetal’s angina, is rare. It’s caused by a spasm in the coronary arteries. This spasm makes the arteries narrow, cutting off blood to the heart and causing pain. Unlike stable angina, it often happens when you’re resting. It can be triggered by stress, cold, or some medicines.
Microvascular Angina
Microvascular angina affects the heart’s small blood vessels. It causes chest pain that doesn’t follow the usual patterns. It’s hard to diagnose because tests don’t show big blockages. Treatment aims to manage symptoms and improve blood flow in these small vessels.
In summary, knowing the different types of angina pectoris is key to good care. Each type has its own signs and needs. Recognizing these differences helps in treating and improving patient outcomes.
Recognizing Angina Pectoris Symptoms
It’s key to spot angina pectoris symptoms early. Finding these signs can be tricky because they differ from person to person.
Classic Chest Pain Symptoms
The main sign of angina is chest pain or discomfort. People often say it feels like a squeeze, pressure, or heavy feeling in the chest. This pain usually happens when you’re active or stressed and goes away when you rest or take medicine.
Not everyone’s chest pain is the same. Some feel sharp pain, while others get a dull ache. Knowing these differences helps doctors diagnose angina pectoris correctly.
Radiation of Pain to Other Body Parts
Pain from angina pectoris isn’t just in the chest. It can spread to the arms, neck, jaw, or ears. This happens because the nerves that serve the heart also cover these areas, making the pain seem to move.
Most often, pain goes to the left arm, but it can also hit the neck, jaw, or back. Sometimes, people feel pain in these spots without chest pain. This makes diagnosing angina more challenging.
Chest and Ear Pain Together: An Atypical Presentation
Angina pectoris can also show up as both chest and ear pain. This is less common but can be a big sign of heart disease, mainly in those at risk.
It’s important for doctors to know about this unusual symptom. This helps them make the right diagnosis and treatment plan.
The Meaning of Pectoris in Angina Pectoris
The term ‘pectoris’ in angina pectoris is more than a medical term. It shows the part of the body affected. To fully grasp angina pectoris, we must explore its etymology and medical terms related to ‘pectoris’.
Etymology and Medical Terminology
The word ‘pectoris’ comes from the Latin ‘pectus,’ meaning chest or breast. In medical terms, ‘pectoris’ means something related to or affecting the chest. “The term ‘angina pectoris’ literally means a condition with a tightening or squeezing sensation in the chest,” say medical experts. This etymological insight is key because it directly ties to the symptoms and nature of angina pectoris.
The use of ‘pectoris’ in angina pectoris points to the main concern—the chest. This is vital for both doctors and patients to grasp the condition’s symptoms and implications.
Common Misspellings and Variations
Despite its importance, ‘pectoris’ is often misspelled or varied. Common errors include ‘pextiors’ or similar variations. It’s important to remember that the correct spelling is ‘pectoris.’ Knowing this helps avoid confusion when talking about angina pectoris in medical or everyday contexts.
Some key points to remember about ‘pectoris’ include:
- The correct spelling is ‘pectoris,’ derived from Latin.
- It refers to conditions or sensations related to the chest.
- Common misspellings can lead to confusion and should be avoided.
In conclusion, grasping the meaning and etymology of ‘pectoris’ in angina pectoris offers valuable insights. By understanding the term’s origin and correct use, we can better understand angina pectoris and its effects on patients.
The Pathophysiology of Heart Angina Symptoms
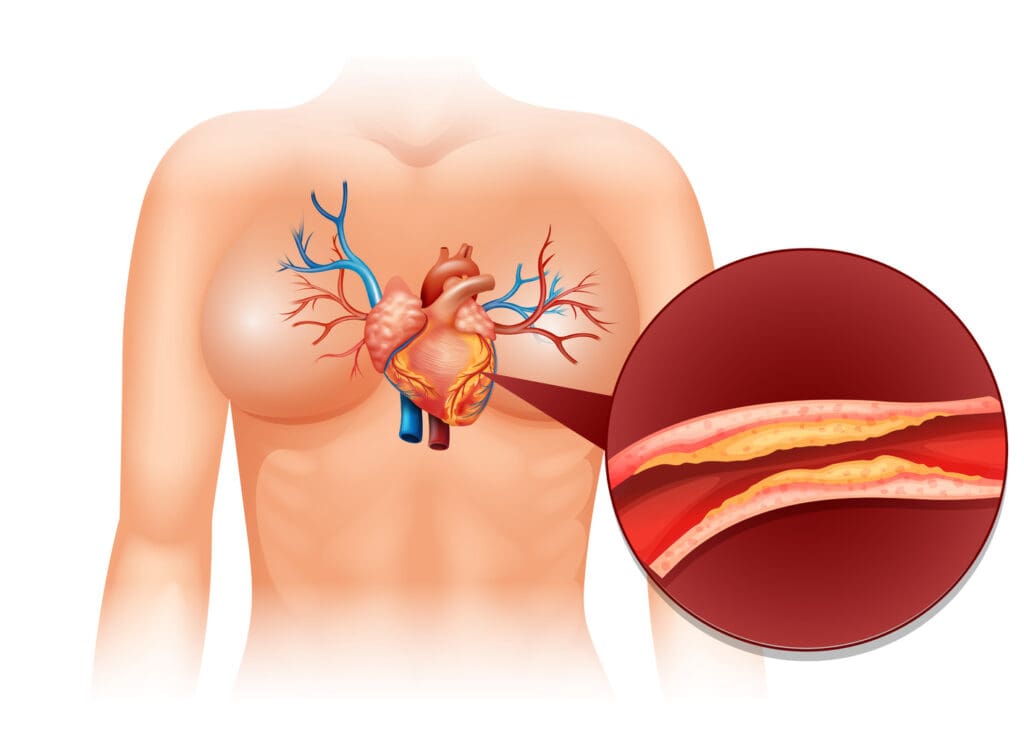
When the heart muscle doesn’t get enough oxygen-rich blood, it can cause angina pectoris. This is chest pain or discomfort. It happens when the heart’s oxygen needs don’t match the blood supply through the coronary arteries.
The Role of Coronary Arteries
The coronary arteries are key in getting blood to the heart muscle. Coronary artery disease happens when these arteries narrow or block due to plaque. This reduces blood flow to the heart, causing angina symptoms, often during activity or stress.
Oxygen Demand vs. Supply Imbalance
The heart needs more oxygen when we’re active or stressed. If the coronary arteries are diseased, they can’t provide enough oxygen. This leads to angina pectoris symptoms.
Factors that cause this imbalance include:
- Atherosclerosis: Plaque buildup in the coronary arteries, causing narrowing or blockage.
- Physical exertion: Activities that raise heart rate and blood pressure, increasing oxygen demand.
- Emotional stress: Stress can also raise heart rate and blood pressure, straining the heart.
Understanding angina pectoris is key to managing its symptoms and preventing complications. By tackling the root causes, like coronary artery disease, we can create better treatment plans. This improves life quality for those with angina.
Common Triggers of Angina Attacks
Certain things can cause angina attacks. Knowing what these are is important for managing the condition. Recognizing these triggers helps patients take steps to prevent them.
Physical Exertion and Exercise
Physical activity is a known trigger for angina attacks. Activities like running, cycling, or lifting heavy objects can cause symptoms. It’s not that exercise is bad; it’s about knowing your limits.
A stress test can help find out when symptoms happen. This info is key for a safe exercise plan. It balances activity with avoiding angina.
Emotional Stress and Anxiety
Emotional stress and anxiety can also trigger angina. High stress can raise heart rate and blood pressure. This can lead to angina if the heart needs more oxygen than it gets.
Methods like meditation, deep breathing, and yoga can help manage stress. Patients should try different methods to find what works for them.
Environmental Factors
Environmental factors can also trigger angina attacks. Cold weather can make blood vessels constrict, leading to angina. High altitudes can lower blood oxygen, causing symptoms in some.
Knowing these environmental triggers helps patients prevent attacks. For example, dressing warmly in cold or avoiding polluted areas can help.
Underlying Causes of Angina Pectoris
It’s important to know what causes angina pectoris to manage it well. Angina often shows that there’s a problem with the heart’s blood flow. This is a big deal for heart health.
Coronary Artery Disease: The Primary Culprit
Coronary artery disease is the main reason for angina pectoris. This happens when the heart’s blood supply gets cut off. This is because of plaque buildup in the arteries.
Managing coronary artery disease is key to avoiding angina. When the arteries narrow, the heart doesn’t get enough oxygen. This leads to the chest pain of angina.
Other Medical Conditions That Can Cause Angina
While coronary artery disease is the main cause, other conditions can also lead to angina. These include:
- Hypertrophic cardiomyopathy
- Severe anemia
- Hyperthyroidism
- Coronary artery spasm
These conditions can affect the heart or change how much oxygen it gets. This can cause angina symptoms.
| Condition | Description | Effect on Angina |
|---|---|---|
| Hypertrophic Cardiomyopathy | Thickening of the heart muscle | Increased oxygen demand |
| Severe Anemia | Low red blood cell count | Reduced oxygen supply |
| Hyperthyroidism | Excess thyroid hormone | Increased heart rate and oxygen demand |
Knowing the causes of angina is key to treating it. By tackling the root cause, we can help patients live better lives.
Risk Factors for Developing Angina Pectoris
Angina pectoris can be caused by genetics, lifestyle, and environment. Knowing these factors helps in prevention and management.
Non-Modifiable Risk Factors
Some risk factors for angina pectoris can’t be changed. These include:
- Age: The risk of developing angina pectoris increases with age, after 45 for men and 55 for women.
- Family History: A family history of heart disease can increase an individual’s risk.
- Gender: Men are generally at higher risk of angina pectoris than women, though women’s risk increases after menopause.
Lifestyle-Related Risk Factors
Lifestyle choices greatly affect the risk of angina pectoris. Key factors include:
- Smoking: Tobacco use damages blood vessels, making them more prone to blockage.
- Physical Inactivity: Not being active can lead to heart disease.
- Obesity: Being overweight or obese increases the risk of heart disease and angina pectoris.
- Diet: A diet high in saturated fats, cholesterol, and sodium can harm the heart.
Medical Conditions That Increase Risk
Certain medical conditions can raise the risk of angina pectoris. These include:
| Medical Condition | Description |
|---|---|
| Hypertension | High blood pressure can damage coronary arteries, increasing the risk of angina. |
| High Cholesterol | Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in arteries. |
| Diabetes | Diabetes mellitus can damage blood vessels and nerves that control the heart. |
Understanding these risk factors helps individuals reduce their chance of getting angina pectoris. It also aids in managing the condition if it occurs.
Diagnosing and Differentiating Angina Pectoris
Diagnosing angina pectoris takes a detailed approach. This includes looking at the patient’s medical history, doing a physical exam, and running various tests. We’ll dive into these steps to see how doctors pinpoint this condition.
Medical History and Physical Examination
Getting a detailed medical history is key in diagnosing angina. We ask about the patient’s symptoms, like the type, how long it lasts, and what triggers it. A physical exam is also done to check for signs of heart disease or other issues.
We also check for risk factors like high blood pressure, high cholesterol, and diabetes. Looking for signs of heart failure or other heart problems is important too.
Diagnostic Tests and Procedures
Several tests help confirm angina pectoris and its severity. These include:
- Electrocardiogram (ECG): This test shows the heart’s electrical activity and can spot ischemia or past heart attacks.
- Stress Test: It watches the heart during exercise to find coronary artery disease.
- Coronary Angiography: Uses dye and X-rays to see the coronary arteries and find blockages.
- Cardiac Biomarkers: Blood tests check for enzymes and proteins released when the heart is damaged.
Which of the Following is Typical of Angina Pectoris?
Typical angina is chest pain or discomfort that comes on with exertion or stress. It goes away with rest or medicine. The pain feels like squeezing or pressure in the chest, sometimes in the arms, neck, or jaw too.
To tell angina apart from other issues, we look at a few things:
- Nature of Pain: Angina pain is usually dull, squeezing, or pressure-like.
- Triggers: It often starts with exertion or emotional stress.
- Relief: Rest or nitroglycerin usually helps.
- Duration: Angina episodes usually last a few minutes.
By knowing these signs and using medical history, physical exams, and tests, we can accurately diagnose and treat angina pectoris.
Treatment Approaches for Angina Pectoris
We treat angina pectoris with a detailed plan. This includes medicines, lifestyle changes, and surgery when needed. Our goal is to control symptoms, enhance life quality, and lower risk of serious issues.
Medications for Symptom Relief and Prevention
Medicines are key in managing angina. They help ease symptoms, prevent attacks, and boost heart health. Common drugs include:
- Nitrates: Relax blood vessels, improving heart blood flow.
- Beta-blockers: Lower the heart’s oxygen need.
- Calcium channel blockers: Relax blood vessels, reducing heart work.
- Antiplatelet drugs: Stop blood clots.
| Medication Type | Primary Use | Benefits |
|---|---|---|
| Nitrates | Relieve angina symptoms | Quick relief, improves blood flow |
| Beta-blockers | Prevent angina episodes | Reduces heart rate, lowers blood pressure |
| Calcium channel blockers | Manage symptoms, lower blood pressure | Relaxes blood vessels, reduces heart workload |
Surgical and Interventional Procedures
For some, surgery or interventional methods are needed. These include:
- Angioplasty and stenting: Opens blocked arteries, keeps them open.
- Coronary artery bypass grafting (CABG): Creates a bypass around blocked arteries.
These methods are used when medicines alone can’t manage symptoms or when arteries are severely blocked.
Lifestyle Modifications as Treatment
Lifestyle changes are vital in managing angina. They help reduce symptoms, improve health, and lower heart disease risk. Key changes include:
- Dietary changes: Eat heart-healthy foods like fruits, veggies, and whole grains.
- Regular exercise: Do physical activity as advised by a doctor.
- Smoking cessation: Quit smoking to lower heart risk.
- Stress management: Use stress-reducing methods like meditation or yoga.
Combining these treatments helps people with angina manage their condition and improve their life quality.
Conclusion: Living with and Managing Angina Pectoris
Understanding and managing angina pectoris is key for patients to live active lives. It involves recognizing symptoms, following treatment plans, and making lifestyle changes. This approach helps manage the condition effectively.
Living with angina means knowing the condition well and its triggers. By using medications, making lifestyle changes, and sometimes surgery, patients can greatly improve their life quality. This approach helps manage the condition well.
Managing angina pectoris well can lower the risk of serious problems and improve health. We work with patients to create treatment plans that meet their specific needs. This helps them manage their condition better.
By being proactive in managing angina, people can reduce its impact on their daily lives. Our aim is to offer top-notch healthcare and support to international patients. We want to help them manage their condition and live happy, fulfilling lives.
FAQ
What is angina pectoris?
Angina pectoris is a condition where the heart doesn’t get enough blood. This leads to chest pain, often a sign of heart disease.
What are the symptoms of angina pectoris?
Symptoms include chest pain and discomfort. Pain can also spread to other parts of the body or the ear.
What is the medical definition of angina pectoris?
It’s when the heart muscle doesn’t get enough oxygen and nutrients. This usually happens because of heart disease.
What are the different types of angina pectoris?
There are several types, including stable and unstable angina. Variant and microvascular angina are also recognized.
What triggers angina attacks?
Physical exertion, emotional stress, and environmental factors can trigger attacks. They cause an imbalance in heart oxygen supply.
What is the meaning of ‘pectoris’ in angina pectoris?
‘Pectoris’ means chest. In angina pectoris, it refers to the chest pain or discomfort.
How is angina pectoris diagnosed?
Doctors use a medical history, physical exam, and tests to diagnose. These tests check for heart disease.
What are the risk factors for developing angina pectoris?
Risk factors include non-modifiable factors and lifestyle choices like smoking. Medical conditions like high blood pressure and diabetes also increase risk.
How is angina pectoris treated?
Treatment includes medications and procedures to improve blood flow. Lifestyle changes are also important to manage risk factors.
Can angina pectoris be managed effectively?
Yes, with the right treatment and lifestyle changes, people can manage angina pectoris. This improves their quality of life.
What is the role of coronary arteries in angina pectoris?
Coronary arteries supply blood to the heart. When they narrow or block, it can cause angina pectoris.
Is chest and ear pain together a typical symptom of angina pectoris?
Chest and ear pain together is not common. But it can be a symptom of angina pectoris. It shows the importance of recognizing different symptoms.
References
Urmc Rochester. Angina. https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=85&ContentID=P00194
National Heart, Lung, and Blood Institute (NHLBI). Angina symptoms. https://www.nhlbi.nih.gov/health/angina-symptoms
American Heart Association. Stable angina (angina pectoris). https://www.heart.org/en/health-topics/heart-attack/angina-chest-pain/angina-pectoris-stable-angina





