Last Updated on December 1, 2025 by Bilal Hasdemir

Every year, over 15,000 stem cell transplants, also known as bone marrow transplants, are performed worldwide, offering hope to those with blood cancers and disorders.
A stem cell transplant is a complex process that replaces damaged or sick bone marrow with healthy cells, potentially saving lives but bringing significant changes to the body.
Understanding what happens after a stem cell transplant is crucial for patients and caregivers as the recovery process can be challenging, with possible complications and side effects.
Key Takeaways
- The bone marrow transplant process involves replacing damaged marrow with healthy functioning marrow.
- Patients undergo significant physical and medical changes after the transplant.
- Understanding the recovery process is key for patients and caregivers.
- The procedure can be life-saving for those with blood cancers and disorders.
- Potential complications and side effects can occur during recovery.
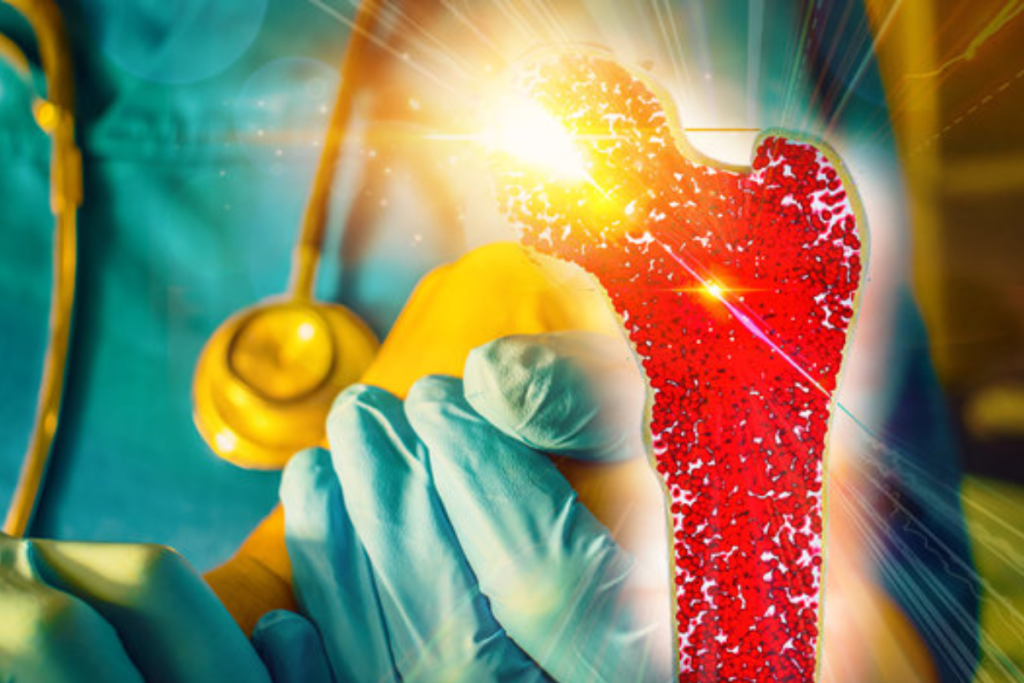
Understanding Bone Marrow and Its Function
Bone marrow is key to how our body makes blood and keeps our immune system strong. It’s the soft tissue inside bones like the hips and thighbones. This tissue makes blood cells.
The Role of Bone Marrow in Blood Production
Bone marrow is vital for making blood cells. It creates red blood cells that carry oxygen, white blood cells that fight infections, and platelets that help blood clot.
The process of making blood is complex. It involves many cell types in the bone marrow. Stem cells, the starting point for all blood cells, are here. They turn into different blood cell types.
How Bone Marrow Affects Immune System Function
The bone marrow is also key to the immune system. It’s where immune cells like B lymphocytes mature. These cells then fight off pathogens in the body.
A healthy bone marrow is vital for a strong immune response. Immunologists have found that without it, people are more at risk for infections and cancers. For example, skin cancer caused by HPV shows how important a good immune system is.
- Bone marrow produces immune cells.
- It supports the body’s defense against infections.
- A healthy bone marrow is essential for immune function.
When Bone Marrow Replacement Becomes Necessary
In some cases, we need to replace bone marrow. This is because of diseases like leukemia and lymphoma. These conditions harm the bone marrow, making it hard to produce healthy blood cells.
Stem cell therapy can be a cure. It replaces damaged bone marrow with healthy cells. These can come from the patient themselves or a donor.
Medical Conditions Requiring a Stem Cell Transplant
Stem cell transplants are key for treating serious medical conditions. They are vital for patients with certain cancers and blood and immune system disorders.
Blood Cancers: Leukemia, Lymphoma, and Myeloma
Blood cancers are treated with stem cell transplants. Leukemia is a cancer of the blood and bone marrow. It makes abnormal white blood cells.
Lymphoma affects the lymphatic system, a key part of the immune system. It causes the uncontrolled growth of lymphocytes. Myeloma, or multiple myeloma, is a cancer of plasma cells in the bone marrow. It can cause anemia, bone pain, and infections.
A stem cell transplant can replace diseased bone marrow with healthy cells. Studies show it improves survival rates for these cancers.
Bone Marrow Failure Syndromes
Bone marrow failure syndromes, like aplastic anemia, happen when the bone marrow can’t make enough blood cells. This leads to severe anemia, infections, and bleeding disorders. A stem cell transplant can restore the bone marrow’s function.
The transplant replaces damaged marrow with healthy stem cells. This can cure the condition. A medical expert says, “A stem cell transplant can be a lifesaving procedure for patients with bone marrow failure syndromes.”
Immune Deficiency Disorders
Immune deficiency disorders, like severe combined immunodeficiency (SCID), weaken the body’s ability to fight infections. SCID lacks both B cells and T cells, making patients very sick. A stem cell transplant can rebuild the immune system by introducing healthy stem cells.
“A stem cell transplant cleared cancer in an immunocompromised woman, illustrating the potential of stem cell transplants in treating certain conditions.”
Stem cell transplants are vital for treating these conditions. They help restore health and improve survival rates.
Types of Bone Marrow Transplants
There are many types of bone marrow transplants, each with its own features and uses. The type chosen depends on the patient’s health, age, and if a good donor is available.
Autologous Transplants: Using Your Own Cells
An autologous transplant uses the patient’s own stem cells. It’s often for patients with certain cancers like multiple myeloma or lymphoma. First, the patient’s stem cells are harvested and stored. Then, they get high-dose chemotherapy and the stem cells are put back in.
Allogeneic Transplants: Using Donor Cells
An allogeneic transplant uses stem cells from a donor. This donor can be a sibling, an unrelated donor, or a cord blood unit. The transplant’s success depends on how well the donor’s and recipient’s HLA genes match.
| Transplant Type | Donor Source | HLA Matching Requirement |
| Autologous | Patient’s own cells | Not applicable |
| Allogeneic | Sibling or unrelated donor | High |
| Haploidentical | Family member (partial match) | Partial |
| Cord Blood | Cord blood unit | Moderate |
Haploidentical and Cord Blood Transplants
Haploidentical transplants use a family member who shares half of the HLA genes. This is useful when a fully matched donor isn’t available.
Cord blood transplants use stem cells from umbilical cord blood. This is an option when an adult donor isn’t available.
Choosing between these transplants depends on the patient’s condition, donor availability, and transplant needs.
Pre-Transplant Preparation of the Body
To boost the success of a bone marrow transplant, a detailed pre-transplant prep is key. This step is vital to get the patient’s body ready for the transplant.
Medical Evaluation and Testing Process
The prep starts with a detailed medical evaluation to check the patient’s health. Tests like blood work and imaging studies are done to make sure the patient is fit for the transplant.
These tests help doctors create a treatment plan that fits the patient’s needs. This reduces the risk of problems during and after the transplant.
Conditioning Regimens: Chemotherapy and Radiation
A big part of the prep is conditioning regimens, which often include chemotherapy and/or radiation. The goal is to weaken the immune system and kill off diseased cells. This makes room for the new stem cells to grow.
Whether to use chemotherapy, radiation, or both depends on the patient’s condition and the transplant type. The healthcare team decides this based on various factors.
Physical Changes During the Preparation Phase
Patients may see physical changes during the prep phase. These can include feeling tired, losing hair, nausea, and changes in appetite.
It’s important for patients to follow the healthcare team’s advice on handling these side effects. This ensures their comfort and safety during the prep.
The Stem Cell Transplant Procedure Explained
It’s important for patients to know about the stem cell transplant process. This detailed procedure includes several key steps. These steps go from getting ready for the transplant to the actual infusion of stem cells.
How Stem Cells Are Harvested from Donors
Donors give stem cells through a special process. First, stem cells are made to move into the blood. Then, apheresis separates these cells from other blood parts. The collected stem cells are then ready for the transplant.
The Transplantation Process Step by Step
The transplant process has several steps:
- Pre-transplant conditioning to prepare the patient’s body
- Infusion of the harvested stem cells
- Post-transplant care to monitor for complications
The conditioning regimen is key. It helps weaken the immune system, making room for the new stem cells.
What Happens in the Body During Infusion
When stem cells are infused, they go into the patient’s blood. This is like a blood transfusion and is done through a central line. The body’s reaction to these new cells can differ, so it’s closely watched.
Initial Cellular Responses to New Stem Cells
After infusion, the body starts to react to the new stem cells. The first response is the stem cells moving to the bone marrow. There, they start making new blood cells. This is key for the transplant’s success.
| Timeline | Cellular Response |
| 0-2 weeks | Stem cells begin to engraft in the bone marrow |
| 2-4 weeks | Production of new blood cells starts |
| 1-3 months | Immune system starts to recover |
Immediate Physical Effects After Transplantation
The time after a bone marrow transplant is very important. Patients experience significant physical changes, and understanding them is essential for effective recovery management.
Changes in Blood Counts and Composition
After a bone marrow transplant, blood counts change. Blood cell counts like white and red blood cells, and platelets, are watched closely. These counts being low means patients are more likely to get sick and bleed.
Getting blood counts back to normal takes time. White blood cells start to recover first, showing the immune system is getting back to work. Red blood cells and platelets take longer, sometimes needing transfusions until the bone marrow can make them.
| Blood Component | Normal Range | Post-Transplant Levels |
| White Blood Cells | 4,500 – 11,000 cells/μL | Initially low, then gradually increase |
| Red Blood Cells | 4.32 – 5.72 million cells/μL (men), 3.90 – 5.03 million cells/μL (women) | Often low, may require transfusions |
| Platelets | 150,000 – 450,000 platelets/μL | Initially low, recovery varies |
Immune System Suppression and Vulnerability
The immune system is very weak after a bone marrow transplant. Immunosuppressive medications are used to stop GVHD, making it even weaker.
To stay safe, patients are kept isolated and follow strict infection control. Watching for infection signs is key, and antibiotics might be given to prevent infections.
Common Physical Symptoms and Side Effects
After a bone marrow transplant, patients can feel tired, nauseous, and have diarrhea. These symptoms come from the treatment before the transplant.
It’s important to manage these symptoms to improve life quality during recovery. Drugs like antiemetics and pain relievers help with nausea and pain.
Medication Effects on the Body
The drugs given after transplant, like immunosuppressants, can affect the body a lot. Immunosuppressants can lead to infections and harm organs.
It’s vital to watch for side effects from these drugs. Changes to treatment might be needed to avoid bad effects. Patients should tell their doctor about any new symptoms or worries.
The Engraftment Process in the Body
The engraftment process is a key part of getting better after a bone marrow transplant. It’s when the body starts making blood cells again. New stem cells move into the bone marrow and start making healthy blood cells.
How New Cells Begin to Grow and Function
After a stem cell transplant, new cells go to the bone marrow. There, they grow and mature. This is important for making healthy blood cells like red and white blood cells, and platelets.
The new stem cells need to engraft in the bone marrow to start making these cells. This process can take weeks. During this time, the patient’s blood counts are watched closely.
Timeline for Blood Cell Production
After a stem cell transplant, blood cell production follows a timeline. At first, blood counts are low because of the treatment. But as the new stem cells engraft, blood cell production starts again.
| Timeline | Blood Cell Production |
| 1-2 weeks | Initial signs of engraftment, with possible increases in white blood cell counts |
| 2-4 weeks | Gradual increase in red blood cell and platelet counts |
| 4-6 weeks | Blood counts typically return to near-normal levels |
Physical Signs of Successful Engraftment
When engraftment is successful, you might feel better. You might have more energy, fewer infections, and your blood counts will get back to normal. You might also feel hungrier and feel better overall as your body heals.
Monitoring these signs is key. It shows how well the engraftment process is going.
Monitoring Blood Counts During Engraftment
During engraftment, blood counts are checked often with blood tests. These tests help doctors see how well the engraftment is going. They can also adjust the patient’s care plan if needed.
How often blood tests are done can change. But they are usually done several times a week until blood counts are stable.
The Body’s Recovery in the First 30 Days
The first 30 days after a transplant are key for recovery. They mark important milestones in the body’s healing. The body starts to adjust to the new stem cells during this time.
Critical Physiological Milestones
In the first 30 days, several critical milestones show how recovery is going. Engraftment, when the new stem cells start making blood cells, is a big one. It’s important to check blood counts to see if engraftment is happening.
Another key point is when the immune system starts to get better. It might take longer than 30 days for it to fully recover. But the early days are vital for starting the immune system’s recovery.
Managing Acute Side Effects
Dealing with side effects early on is a big challenge. Side effects like fatigue, nausea, and mouth sores are common. To manage them, a mix of medicine, diet changes, and rest is needed.
Medications are key in fighting these side effects. Drugs for nausea and pain help reduce discomfort and prevent serious problems.
Nutritional Challenges and Solutions
After a bone marrow transplant, eating well can be tough. Patients might have trouble tasting food, feel sick to their stomach, and struggle to get enough calories and nutrients. Nutritional counseling and supplements can help.
- Eating a balanced diet with lots of proteins, vitamins, and minerals is important.
- Eating small meals often can help with nausea.
- Drinking plenty of water, focusing on fluids with electrolytes, is also key.
Hospital Discharge Considerations
When a patient is ready to go home, it’s called hospital discharge. Before leaving, they get advice on medication management, follow-up visits, and what to watch for. It’s important to have a support system at home and follow the healthcare team’s advice closely.
Potential Complications and Body Responses
It’s important to know the possible problems after a bone marrow transplant. These transplants can save lives but also have risks. Managing these risks is key for good care.
Infection Risks and Prevention Strategies
One big problem after a transplant is infections. The treatment before the transplant weakens the immune system. This makes patients more likely to get sick.
Prevention Strategies: To lower infection risks, patients get antibiotics and antivirals. They also need to wash hands a lot and stay away from sick people.
Graft-Versus-Host Disease: Causes and Manifestations

Graft-versus-host disease (GVHD) happens when the donor’s immune cells attack the recipient’s body. It can be acute or chronic, with different symptoms and times.
Causes and Risk Factors: GVHD is more common in allogeneic transplants. The match between donor and recipient, the stem cell source, and the treatment used affect the risk.
| GVHD Type | Timeline | Common Manifestations |
| Acute GVHD | Within 100 days post-transplant | Skin rash, liver dysfunction, gastrointestinal symptoms |
| Chronic GVHD | After 100 days post-transplant | Variable, can affect skin, mouth, eyes, liver, and other organs |
Organ System Complications
Bone marrow transplants can cause problems with different organs. These can be mild or severe, like liver or lung issues, and heart problems.
Management and Monitoring: It’s vital to watch and manage these problems closely. Regular checks on organ function and quick action when needed are important.
The Body’s Immune System Rebuilding
Rebuilding the immune system is key after a bone marrow transplant. It’s a complex process. The body regenerates immune cells like T cells, B cells, and natural killer cells.
Phases of Immune Reconstitution
Immune reconstitution happens in phases. First, the immune system is suppressed due to the conditioning regimen. Then, new immune cells start to form from the transplanted stem cells.
The first few months post-transplant are risky due to slow immune recovery. But, the immune function gets better over time. It can take up to a year or more for the immune system to fully recover.
Vaccination Schedule After Transplant
After a bone marrow transplant, a specific vaccination schedule is needed. This includes vaccines for diseases like influenza, pneumococcus, and tetanus.
| Vaccine | Recommended Timing | Doses |
| Influenza | 6-12 months post-transplant | 1 dose annually |
| Pneumococcal | 3-6 months post-transplant | 3-4 doses |
| Tetanus | 6-12 months post-transplant | 3 doses |
Graft-versus-Leukemia Effect
The graft-versus-leukemia (GVL) effect is when donor immune cells fight the recipient’s leukemia cells. This can help control or eliminate the leukemia.
The GVL effect is a major reason why allogeneic bone marrow transplants can cure certain types of leukemia.
Long-term Immune Function and Protection
Long-term immune function after a bone marrow transplant varies. It depends on the transplant type, graft-versus-host disease, and the patient’s age.
Regular follow-up care is vital. It helps monitor immune function and prevent infections and complications.
Long-Term Effects on the Body Systems
A bone marrow transplant can have lasting effects on a person’s health. Survivors face challenges that impact their well-being after recovery.
Potential Late Complications by Organ System
Organ systems can be affected long-term, leading to complications. These include:
- Lung problems, including chronic graft-versus-host disease (GVHD) affecting the lungs
- Cardiovascular issues, such as hypertension and heart disease
- Liver dysfunction, potentially related to GVHD or infections
- Kidney damage, which may be a result of medications or disease
Secondary Cancers Risk and Monitoring
Secondary cancers are a significant risk after a bone marrow transplant. This risk comes from the conditioning regimen and the transplant process. Regular monitoring is key for early detection.
Monitoring strategies include:
- Regular follow-up appointments with healthcare providers
- Screening tests as recommended by guidelines for secondary cancer detection
Fertility and Hormonal Changes
Fertility can be impacted by the conditioning regimen, leading to infertility or premature menopause. Hormonal changes may also occur, requiring hormone replacement therapy in some cases.
“The impact of bone marrow transplantation on fertility and hormonal balance highlights the need for thorough care.” – Expert in Hematology
Cardiovascular and Metabolic Effects
Cardiovascular and metabolic changes are common long-term effects. These include an increased risk of cardiovascular disease and metabolic syndrome. Lifestyle changes and medical management are essential to manage these risks.
Lifestyle adjustments may include:
- Dietary changes to manage weight and improve cardiovascular health
- Regular physical activity to enhance overall well-being
Monitoring and Follow-up Care After Stem Cell Transplant
Monitoring and follow-up care are key after a stem cell transplant. Patients need close watch to ensure a smooth recovery. This helps catch any complications early on.
Routine Testing and Evaluation Schedule
Regular check-ups and tests are essential. They help track the patient’s progress and spot any issues early. The schedule depends on the patient’s condition and transplant details.
- Regular blood tests to monitor blood cell counts and detect any signs of infection or graft-versus-host disease (GVHD).
- Periodic bone marrow biopsies to assess the health of the bone marrow and the presence of any residual disease.
- Imaging studies, such as X-rays, CT scans, or PET scans, to evaluate the overall health of the body and detect any abnormalities.
A study in the Journal of Clinical Oncology shows regular care boosts outcomes. It helps catch and manage complications early.
“The importance of follow-up care cannot be overstated. It is during these visits that we can identify and address issues before they worsen, improving recovery chances.” –
Signs That Require Medical Attention
Patients and caregivers must know when to seek help. Look out for fever, chills, shortness of breath, severe fatigue, and GVHD signs like skin rash or jaundice.
| Symptom | Possible Cause | Action |
| Fever | Infection | Seek immediate medical attention |
| Skin Rash | Graft-Versus-Host Disease (GVHD) | Contact healthcare provider |
| Severe Fatigue | Anemia or other complications | Discuss with healthcare team |
Long-term Survivorship Care
Long-term care focuses on managing late effects. This includes watching for secondary cancers, chronic GVHD, and long-term side effects.
Preventive Health Measures are also key. This includes vaccinations, lifestyle changes, and screenings for late complications.
Preventive Health Measures
Preventive steps are vital for long-term health. Stay current with vaccinations, eat well, exercise, and get regular screenings for late effects.
- Follow the recommended vaccination schedule to protect against infections.
- Maintain a healthy diet and stay hydrated to support overall health.
- Engage in regular physical activity to improve strength and well-being.
By following a detailed care plan, transplant recipients can improve their recovery and long-term health.
Quality of Life After Bone Marrow Transplant
After a bone marrow transplant, patients worry about their quality of life. This includes physical, emotional, and social health. Survivors face many challenges that affect their well-being.
Psychological Adaptation and Coping
Recovering from a bone marrow transplant is tough on the mind. Patients deal with anxiety, depression, and PTSD. Finding ways to cope is key.
- Counseling and Therapy: Professional help can teach patients to handle their feelings.
- Support Groups: Being part of a support group helps patients feel connected and understood.
- Family and Friends: Loved ones are essential for emotional support and help.
Return to Normal Activities and Work
Going back to normal life and work is a big step. But, it’s hard because patients have to deal with their physical limits. They want to live their lives as usual.
- Start doing more things slowly to avoid getting too tired.
- Talk to employers about what they need to make coming back to work easier.
- Take care of yourself by resting, eating well, and managing stress.
Understanding the challenges of life after a bone marrow transplant helps patients cope better. With the right strategies, they can recover more confidently.
Conclusion
Knowing how the body reacts to a bone marrow transplant is key for patients. The recovery is complex, from the start of engraftment to long-term effects on the body.
A successful stem cell transplant needs careful planning, precise medical care, and follow-up. Patients should watch out for complications like graft-versus-host disease and infections. This ensures quick action if needed.
As the immune system rebuilds, vaccinations and health checks are important. The transplant’s long-term effects can affect fertility, heart health, and cancer risk.
By understanding these aspects and working with healthcare, patients can face recovery’s challenges. This helps them live better after a bone marrow or stem cell transplant.
FAQ
What is a bone marrow transplant?
A bone marrow transplant replaces a patient’s bone marrow with healthy stem cells. It treats blood-related diseases like leukemia and lymphoma.
How are stem cells harvested for a transplant?
Stem cells are taken from bone marrow, blood, or umbilical cord blood. A medical procedure collects these cells from the donor or the patient.
What is the difference between autologous and allogeneic transplants?
Autologous transplants use the patient’s own stem cells. Allogeneic transplants use a donor’s stem cells. The choice depends on the condition and donor availability.
What is the conditioning regimen for a bone marrow transplant?
The conditioning regimen uses chemotherapy and/or radiation. It destroys the bone marrow and suppresses the immune system. This prepares the body for new stem cells.
How long does it take for the new stem cells to engraft?
Engraftment takes several weeks. During this time, new stem cells start producing blood cells. The exact time varies by individual.
What are the possible complications after a bone marrow transplant?
Complications include infections, graft-versus-host disease, and organ damage. Close monitoring and follow-up care are key to managing these risks.
How does the immune system rebuild after a bone marrow transplant?
The immune system rebuilds over time. Different parts recover at different rates. Vaccinations help restore immune function.
What are the long-term effects of a bone marrow transplant?
Long-term effects include secondary cancers and fertility issues. Hormonal and cardiovascular changes are also possible. Regular follow-up care is essential.
How can patients manage their quality of life after a bone marrow transplant?
Patients can adapt to their new life. They can cope with psychological challenges and gradually return to normal activities.
What is the importance of follow-up care after a stem cell transplant?
Follow-up care is vital for monitoring recovery and managing complications. Regular testing ensures the best outcomes.
Is a stem cell transplant painful?
The transplant procedure itself is not painful, thanks to sedation or anesthesia. But, patients may feel discomfort or pain during recovery.
How long does a bone marrow transplant take?
The hospital stay for a bone marrow transplant varies. It can be several weeks to a few months. Recovery can take months to a year or more.
Can bone marrow grow back after a transplant?
Yes, new stem cells can grow and produce healthy blood cells. This replaces the patient’s original bone marrow.
What is the graft-versus-leukemia effect?
The graft-versus-leukemia effect is when donor stem cells fight any remaining leukemia cells. This helps prevent cancer from coming back.
References
- Tichelli, A., et al. (2021). Long-term effects of hematopoietic stem cell transplantation. British Journal of Hematology, 192(6), 1018-1033.