Every year, thousands of patients undergo a bone marrow transplant to save their lives. This vital treatment replaces the patient’s damaged or diseased bone marrow with healthy stem cells from either the patient or a compatible donor, offering hope for cancer, blood disorders, and immune system diseases.
This complex process needs careful planning and matching of donor and recipient. It also requires detailed care after the transplant. Knowing how BMT transplantation works is key for patients, caregivers, and doctors to help each other through this journey.
Key Takeaways
- A bone marrow transplant is a life-saving treatment for various medical conditions.
- The procedure involves replacing diseased marrow with healthy cells.
- Careful preparation and matching are critical for a successful transplant.
- Post-transplant care is essential for patient recovery.
- Understanding the BMT process is vital for patients and caregivers.
Understanding Bone Marrow and Its Function
Bone marrow is a key part of our bodies. It’s vital for our health. If it fails, we face serious health problems.
What is Bone Marrow?
Bone marrow is found in bones like the hips and thighbones. It makes blood cells, like red and white blood cells, and platelets. These cells carry oxygen, fight infections, and help blood clot.
The Role of Bone Marrow in the Body
Bone marrow does more than make blood cells. It’s also key to our immune system. “It helps develop immune cells like B and T cells, which fight infections.” It also stores stem cells for repair and growth.
When Bone Marrow Fails
When bone marrow fails, health issues arise. Problems like leukemia and aplastic anemia can occur. A bone marrow transplant may be needed to fix it.
Some people get transplants to replace their immune system. This shows how important bone marrow is for our health.
What is a Bone Marrow Transplant?
Bone marrow transplantation, also known as hematopoietic stem cell transplantation (HSCT), is a complex medical procedure. It involves replacing a patient’s bone marrow with healthy stem cells. This treatment is used for various life-threatening diseases, including certain types of cancer and blood disorders.
Definition and Basic Concept
A bone marrow transplant (BMT) is a medical procedure where damaged or diseased bone marrow is replaced. The term “BMT medical abbreviation” is commonly used in medical contexts to refer to this procedure. Understanding “bmt meaning medical” is key for patients and healthcare providers, as it’s a major treatment for many blood conditions.
When looking at “what is bmt in medical terms,” it’s important to know BMT involves the infusion of hematopoietic stem cells. These can come from the patient themselves (autologous transplant) or a donor (allogeneic transplant). The “bmt medical term” is often used the same as HSCT, showing the focus on stem cell transplantation.
History of Bone Marrow Transplantation
The history of bone marrow transplantation began in the mid-20th century, with the first successful transplant in 1968. Over the years, there have been big improvements in making the procedure safer and more effective. A pioneer in the field noted, “
The development of bone marrow transplantation has been a remarkable journey, transforming the treatment landscape for many hematological disorders.”
Common Terminology (BMT, HSCT)
In bone marrow transplantation, several terms are often used. BMT and HSCT are often used the same way, but HSCT is broader. It includes not just bone marrow but also peripheral blood and cord blood stem cell transplants. Knowing these terms is important for clear communication between healthcare providers and patients.
Medical Conditions Requiring Bone Marrow Transplant
Bone marrow transplants are needed when the bone marrow is damaged. They are a lifesaving option for people with certain serious diseases.
Leukemia and Lymphomas
Leukemia is a blood and bone marrow cancer. Lymphomas are cancers of the lymphatic system. Bone marrow transplants for leukemia can cure the disease by replacing bad cells with good ones.
Aplastic Anemia
Aplastic anemia means the bone marrow can’t make blood cells. A bone marrow transplant is the only cure for severe cases. It gives a new source of healthy stem cells.
Sickle Cell Disease
Sickle cell disease is a genetic disorder that affects hemoglobin. It can cause severe anemia and infections. BMT for sickle cell disease can cure it, mainly in young patients.
Other Conditions
Other conditions needing a bone marrow transplant include multiple myeloma and certain autoimmune diseases.
Understanding why someone would need a bone marrow transplant shows how serious these conditions are. Bone marrow transplants can replace damaged marrow with healthy cells. This offers hope for recovery and a better life.
Types of Bone Marrow Transplants
Bone marrow transplants are divided into several types. These include autologous, allogeneic, haploidentical, and cord blood transplants. Knowing about these types helps find the best treatment for patients.
Autologous Transplants
Autologous bone marrow transplants use the patient’s own stem cells. They are often used for cancers like multiple myeloma or lymphoma. First, the patient’s stem cells are harvested and stored. Then, they get high-dose chemotherapy and the stem cells are reinfused.
Allogeneic Transplants
Allogeneic transplants use stem cells from a donor. This donor can be a sibling, parent, or someone unrelated. They are used for leukemia or blood disorders. The transplant’s success depends on how well the donor and recipient’s HLA match.
Haploidentical Transplants
Haploidentical transplants use a donor who is a half-match, often a family member. They are useful when a full match is not available.
Cord Blood Transplants
Cord blood transplants use stem cells from a newborn’s umbilical cord. They are used when no matched donor is available.
| Type of Transplant | Donor Source | Common Uses |
| Autologous | Patient’s own cells | Multiple myeloma, lymphoma |
| Allogeneic | Matched donor | Leukemia, blood disorders |
| Haploidentical | Half-matched family member | Various blood cancers |
| Cord Blood | Umbilical cord blood | Patients without a matched donor |
In conclusion, the choice of bone marrow transplant depends on several factors. These include the patient’s condition, donor availability, and the disease being treated.
Finding a Bone Marrow Donor
Finding the right bone marrow donor is key to a successful transplant. It starts with understanding the importance of Human Leukocyte Antigen (HLA) matching.
HLA Matching Process
HLA matching is vital to avoid graft-versus-host disease (GVHD). GVHD is a serious issue in bone marrow transplants. HLA typing helps find compatible donors.
Sibling and Family Donors
Siblings and family members are often the first choice for donation. They might share similar genes with the patient. But, not all family members are a match.
Unrelated Donor Registries
If a family member isn’t a match, donor registries are used. These registries have HLA typing for millions of donors worldwide.
Becoming a Bone Marrow Donor
People can register to be bone marrow donors. It involves giving a cheek swab or blood sample for HLA typing.
| Donor Type | HLA Matching Importance | Donation Process |
| Sibling/Family | High | Bone marrow or peripheral blood stem cell collection |
| Unrelated | High | Registered through a donor registry; may involve bone marrow or peripheral blood stem cell collection |
Being a bone marrow donor can save lives. Understanding HLA matching and the donation process helps make informed choices.
Pre-Transplant Evaluation and Preparation
The pre-transplant evaluation is a key step in the bone marrow transplant process. It checks if the patient is ready medically and mentally. This detailed check makes sure the patient is ready for the transplant and its challenges.
Medical Assessment
A detailed medical check is done to look at the patient’s health. It reviews their medical history and current health. It also checks for risks related to the transplant. Cardiac, pulmonary, and hepatic functions are checked to see if they can handle the transplant.
Psychological Preparation
Psychological preparation is also key, as the transplant can be emotionally tough. Patients get counseling to deal with stress and anxiety. This support is important for their mental health during recovery.
Central Venous Catheter Placement
A central venous catheter is put in for medication and transfusions. This is done under local anesthesia. It makes it safe and easy to give treatments.
The Bone Marrow Transplant Procedure Step by Step
A bone marrow transplant is a detailed process. It needs careful planning and execution. It includes several key stages, from the start to the end.
Conditioning Regimen (Chemotherapy/Radiation)
The first step is the conditioning regimen. This involves giving high-dose chemotherapy and/or radiation. It aims to kill the old bone marrow and weaken the immune system.
Stem Cell Collection Methods
Next, stem cells are collected. They can come from a donor or the patient’s own cells. The cells are taken from the bone marrow or the blood after mobilization.
The Day of Transplant
The transplant day is a big moment. The stem cells are prepared for infusion, like a blood transfusion.
What Happens During Infusion
During infusion, the stem cells are given through a catheter. It takes a few hours. Patients are watched closely for any bad reactions.
After infusion, the stem cells go to the bone marrow. There, they start making new blood cells. The bone marrow transplant is a complex treatment. It gives hope to those with serious diseases. Knowing the steps helps patients and families understand the process better.
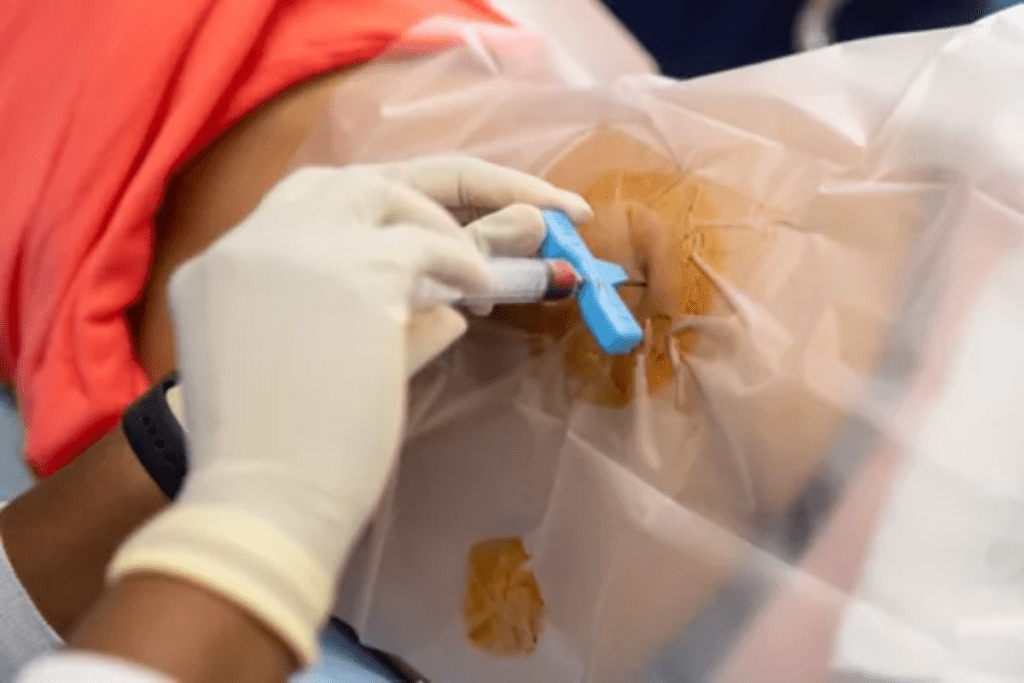
How is Bone Marrow Harvested from Donors
Harvesting bone marrow from donors is a complex process. It has changed over time. The goal is to take bone marrow or stem cells from a donor and give them to someone else. There are two main ways to do this: traditional bone marrow harvest and peripheral blood stem cell collection.
Traditional Bone Marrow Harvest
Traditional bone marrow harvest takes marrow from the donor’s hip bones. This is done under general anesthesia so the donor doesn’t feel pain. A needle and syringe are used to get the marrow, and how much depends on what the recipient needs.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is a gentler method. It makes the donor’s stem cells go into their blood. Then, these cells are collected using apheresis. This method doesn’t need surgery and is often preferred by donors because it’s less invasive.
Anesthesia and Procedure Details
For traditional bone marrow harvest, general anesthesia is used. This keeps the donor comfortable during the procedure. The team can get the needed bone marrow without causing pain or stress to the donor. The whole process usually takes a few hours, and the donor is watched closely before and after.
Choosing between traditional bone marrow harvest and peripheral blood stem cell collection depends on many things. These include the recipient’s health and the donor’s condition. Both methods have their benefits and are chosen based on the transplant’s specific needs.
Post-Transplant Hospital Care
The post-transplant period is critical, and hospital care plays a vital role in the patient’s recovery journey. After a bone marrow transplant, patients are closely monitored for any signs of complications. They receive care to support their recovery.
Isolation Procedures
To minimize the risk of infection, patients are often placed in isolation. They are in a single room with controlled air flow. This reduces exposure to pathogens. Visitors must wear protective gear, like masks and gowns, to further minimize the risk of introducing infections.
Monitoring for Engraftment
Monitoring for engraftment is a critical aspect of post-transplant care. This involves regular blood tests to check for signs that the new stem cells are producing blood cells. Successful engraftment is indicated by rising blood cell counts, which is a positive sign of recovery.
Managing Immediate Complications
Immediate complications can arise after a bone marrow transplant, including infections, bleeding, and graft-versus-host disease (GVHD). Managing these complications involves a combination of medications, including antibiotics, antivirals, and immunosuppressants. The healthcare team closely monitors the patient’s condition and adjusts treatment as necessary.
| Complication | Management Strategy |
| Infections | Antibiotics, antivirals, and supportive care |
| Bleeding | Platelet transfusions and clotting factor replacement |
| GVHD | Immunosuppressive medications |
Hospital Stay Duration
The length of hospital stay after a bone marrow transplant can vary. It depends on the patient’s condition and the specifics of their treatment. On average, patients can expect to stay in the hospital for several weeks. During this time, the healthcare team provides around-the-clock care to manage complications and support recovery.
“The care received during the post-transplant period is critical for the success of the bone marrow transplant. It requires a coordinated effort from the healthcare team to manage complications and support the patient’s recovery.”
Expert in BMT

Recovery After Bone Marrow Transplant
Recovering from a bone marrow transplant takes time, patience, and medical care. It’s a journey with many stages, each important for your health. You’ll need a strong support system to get through it.
The First 100 Days
The first 100 days are very important. Doctors watch for signs of new blood cells, infections, and other issues. Engraftment, when new blood cells start, is a big milestone.
Patients often feel tired, weak, and have other side effects. It’s key to manage these and prevent infections. Doctors use prophylactic medications to stop infections and graft-versus-host disease (GVHD).
Immune System Reconstitution
Rebuilding your immune system is a big part of recovery. This can take months to a year or more. Patients are at risk for infections and need ongoing medical care.
- Regular follow-up appointments with healthcare providers
- Monitoring for signs of infection or GVHD
- Adherence to prescribed medications
Medications and Follow-up Care
Follow-up care is key to managing recovery. This includes taking medicines as directed, going to appointments, and watching for complications.
Every person’s recovery from a bone marrow transplant is different. With the right care, support, and medical help, many can fully recover and live a normal life again.
Potential Complications and Side Effects
It’s important to know about the risks of bone marrow transplants. This procedure can cure serious diseases but comes with big risks. Knowing these risks helps in caring for patients better.
Graft-Versus-Host Disease (GVHD) is a big problem after an allogeneic bone marrow transplant. GVHD happens when the donor’s immune cells see the recipient’s body as foreign and attack it. This can harm the skin, liver, and gut.
Graft-Versus-Host Disease (GVHD)
GVHD is a major cause of sickness and death after a transplant. Doctors use medicines to prevent and treat it. The chance of getting GVHD depends on how well the donor and recipient match, the type of stem cells, and the treatment given.
Infections and Immune Suppression
People getting bone marrow transplants are more likely to get infections. This is because the treatments weaken the immune system. They can get infections like bacteria, viruses (like CMV), and fungi.
Long-term Side Effects
People who survive bone marrow transplants might face long-term problems. These can include damage to organs, new cancers, and hormonal issues. The risk of these problems depends on the treatment, GVHD, and the patient’s age at the time of the transplant.
| Complication | Description | Management |
| GVHD | Immune reaction against host tissues | Immunosuppressive drugs |
| Infections | Bacterial, viral, fungal infections due to immunosuppression | Prophylactic antimicrobials, monitoring |
| Long-term Side Effects | Organ damage, secondary cancers, hormonal imbalances | Long-term follow-up, management of chronic conditions |
Handling complications and side effects is key in bone marrow transplant care. Knowing these risks helps prepare and follow up better. This improves patient results.
Advances in Bone Marrow Transplantation
Recent years have brought big changes to bone marrow transplantation. These changes have made the procedure safer and more effective. Now, more people can get this life-saving treatment.
Reduced-Intensity Conditioning
Reduced-intensity conditioning (RIC) is a big step forward. It lets older or weaker patients get transplants. These patients can’t handle the usual strong treatments.
RIC uses lower doses of chemotherapy and radiation. This makes the transplant process safer and less harsh.
Gene Therapy Applications
Gene therapy is a new and exciting field. It changes genes to treat or prevent diseases.
In bone marrow transplants, gene therapy could fix genetic problems. It does this by changing the patient’s stem cells before they are put back in.
CAR-T Cell Therapy
CAR-T cell therapy is a type of immunotherapy. It uses the patient’s T cells, which are made to fight cancer cells.
| Therapy Type | Description | Benefits |
| CAR-T Cell Therapy | T cells engineered to target cancer cells | Effective against certain leukemias and lymphomas |
| Gene Therapy | Genetic modification to treat diseases | Potential cure for genetic disorders |
Future Directions
The future of bone marrow transplantation looks bright. Researchers are working on new treatments and technologies. This includes better conditioning regimens, gene editing, and cellular therapies.
Conclusion
Bone marrow transplant (BMT) is a key treatment for serious blood and immune system diseases. It’s a complex procedure that can save lives. Knowing about it is important.
The success of a transplant depends on many things. These include the type of transplant, how well the donor and patient match, and the patient’s health. Thanks to new research, more people are surviving and recovering well from BMT.
Recovering from a bone marrow transplant takes time and careful care. Patients must follow a strict treatment plan and make lifestyle changes. This helps ensure a good outcome. As BMT research grows, so does the hope for better treatments and support.
Learning about bone marrow transplantation helps patients and doctors work together. This teamwork can lead to better results and a better life for those with these diseases.
FAQ
What is a bone marrow transplant?
A bone marrow transplant, also known as hematopoietic stem cell transplantation (HSCT), is a medical procedure. It replaces a patient’s bone marrow with healthy stem cells. These stem cells can come from the patient or a donor.
What is bone marrow, and what does it do?
Bone marrow is the spongy tissue inside some bones. It makes blood cells, like red and white blood cells, and platelets. It’s key to the immune system and health.
Why is a bone marrow transplant necessary?
A bone marrow transplant is needed for patients with certain cancers, blood disorders, and immune diseases. This includes leukemia, lymphomas, aplastic anemia, and sickle cell disease.
What are the different types of bone marrow transplants?
There are several types of bone marrow transplants. These include autologous transplants (using the patient’s own stem cells), allogeneic transplants (using donor cells), haploidentical transplants (using a partially matched donor), and cord blood transplants (using stem cells from umbilical cord blood).
How is a bone marrow donor found?
A bone marrow donor is found through Human Leukocyte Antigen (HLA) matching. This tests the patient’s and donor’s tissue type for compatibility. Donors can be siblings, family members, or unrelated individuals in donor registries.
What is the bone marrow transplant process like?
The bone marrow transplant process has several steps. It includes a conditioning regimen (chemotherapy and/or radiation), stem cell collection, and infusion of the stem cells into the patient’s bloodstream.
How is bone marrow harvested from donors?
Bone marrow can be harvested from donors in two ways. It can be extracted from the donor’s hip bones under anesthesia or collected from the bloodstream after stimulating stem cells.
What are the possible complications and side effects of a bone marrow transplant?
Possible complications and side effects include graft-versus-host disease (GVHD), infections, and long-term side effects. These can include organ damage, secondary cancers, and hormonal imbalances.
How long does it take to recover from a bone marrow transplant?
Recovery from a bone marrow transplant can take months to a year or more. The first 100 days are critical. Patients need ongoing medications and follow-up care to manage complications and ensure a successful transplant.
What are the latest advancements in bone marrow transplantation?
The latest advancements include reduced-intensity conditioning, gene therapy applications, and CAR-T cell therapy. These offer new hope to patients undergoing this complex treatment.
References
- National Marrow Donor Program/Be The Match. (n.d.). Bone Marrow Transplant Process. Retrieved September 25, 2025, fromhttps://bethematch.org/transplant-basics/understanding-the-transplant-process/