Last Updated on November 27, 2025 by Bilal Hasdemir
Chronic ischemic heart disease (SIHD) is a common condition where the heart doesn’t get enough blood. It affects millions globally. In the U.S., about 20 million people have it.
Managing SIHD well is key to avoiding serious problems and improving life quality. At Liv Hospital, we offer top-notch care based on the latest research and patient needs.
We know each patient with chronic IHD is different. Our treatment plans are made to fit each person’s needs. This ensures they get the best care and support every step of the way.
Key Takeaways
- Understanding the prevalence and impact of chronic ischemic heart disease.
- Importance of effective management and treatment strategies for SIHD.
- Overview of patient-centered care approaches at Liv Hospital.
- Role of latest medical research in guiding treatment protocols.
- Comprehensive support for international patients seeking advanced medical treatments.
Understanding Chronic Ischemic Heart Disease
Chronic ischemic heart disease is a serious condition. It involves the heart’s blood flow being reduced. We will look at what causes it and how it affects people.
Definition and Pathophysiology
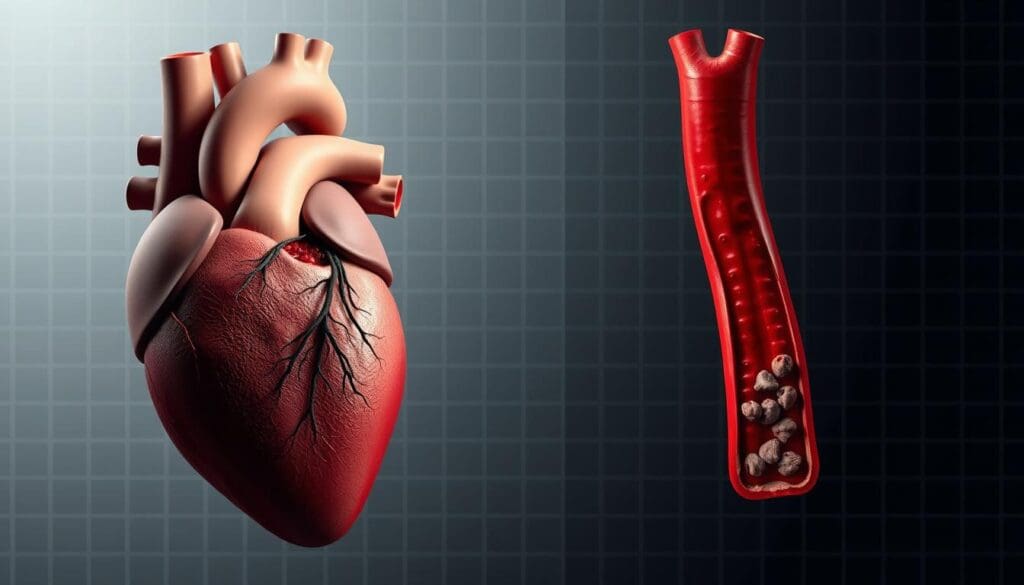
Also known as coronary artery disease, it happens when heart arteries get blocked. This blockage is due to a buildup of plaque. The plaque is made of fat, cholesterol, and other substances.
This buildup reduces blood flow to the heart. As a result, the heart muscle doesn’t get enough oxygen and nutrients. This is called ischemia.
The disease’s causes are complex. It involves artery blockage, inflammation, and other issues. Knowing these causes helps doctors find better treatments.
Stable Ischemic Heart Disease (SIHD) vs. Acute Coronary Syndrome (ACS)
It’s important to know the difference between stable ischemic heart disease (SIHD) and acute coronary syndrome (ACS). SIHD is a condition where symptoms come and go. They are usually triggered by stress or exertion and go away with rest or medicine.
On the other hand, ACS is a sudden and serious condition. It can be a heart attack or unstable angina. It needs immediate medical help.
Knowing the difference helps doctors decide how to treat each case. ACS needs quick action, while SIHD can be managed over time.
Prevalence and Impact in the United States
Chronic ischemic heart disease is a big problem in the United States. It affects millions of adults. It’s a leading cause of illness, death, and healthcare costs.
The risk of getting it goes up with age. It’s also more common in some groups because of factors like high blood pressure and diabetes.
A study shows managing risk factors is key to fighting this disease on cardiovascular health. Knowing how widespread it is helps in planning how to fight it.
Strategy 1: Complete Risk Check and Diagnosis
Managing chronic ischemic heart disease starts with a full risk check and diagnosis. We know that ischemic heart disease treatment works best when we understand each patient’s risk factors and symptoms.
Clinical Evaluation and Symptom Assessment
Diagnosing and assessing ischemic heart disease needs a detailed clinical evaluation. This includes a full medical history, physical check-up, and symptom review. We look for signs like angina, shortness of breath, and tiredness, which show how severe advanced ischemic heart disease is.
Diagnostic Testing and Imaging
Diagnostic tests are key to confirming the disease and its extent. We use tests like electrocardiograms (ECGs), stress tests, echocardiograms, and coronary angiography. These help us see the types of ischemic heart disease and how it affects the heart.
- ECGs spot patterns of ischemia or past heart attacks.
- Stress tests check how the heart works under stress.
- Echocardiograms show the heart’s structure and function.
- Coronary angiography shows the coronary arteries and finds blockages.
Risk Stratification for Treatment Planning
Risk stratification is vital for planning ihd treatment. We look at the patient’s risk factors, symptoms, and test results to group them. This helps us tailor the treatment to each patient’s needs.
| Risk Category | Characteristics | Treatment Approach |
|---|---|---|
| Low Risk | Few risk factors, mild symptoms | Lifestyle changes, medical therapy |
| Intermediate Risk | Moderate risk factors, manageable symptoms | More medical therapy, possible revascularization |
| High Risk | Many risk factors, severe symptoms | Strong medical therapy, revascularization |
By using a detailed risk assessment and diagnosis, we can create effective treatment plans. This approach improves outcomes for patients with chronic ischemic heart disease.
Strategy 2: Lifestyle Modifications for Chronic Ischemic Heart Disease
Managing chronic ischemic heart disease requires a multi-faceted approach. Lifestyle changes are a key part of this. By adopting healthier habits, people can lower their risk of complications and improve their life quality.
Dietary Approaches for Heart Health
Eating a heart-healthy diet is essential for managing chronic cardiac disease. We suggest eating lots of fruits, vegetables, whole grains, and lean proteins. It’s also important to cut down on saturated fats, trans fats, and cholesterol.
The Mediterranean diet is great for heart health. It focuses on olive oil, nuts, and fatty fish. Making smart food choices can help manage the condition and may reduce medication needs.
| Dietary Component | Recommended Foods | Foods to Limit |
|---|---|---|
| Fats | Olive oil, nuts, fatty fish | Saturated fats, trans fats |
| Proteins | Lean meats, fish, beans | Processed meats |
| Carbohydrates | Whole grains, fruits, vegetables | Refined grains, added sugars |
Physical Activity and Exercise Recommendations
Regular exercise is vital for managing chronic ischemic heart disease. Aim for at least 150 minutes of moderate-intensity aerobic exercise weekly. Or, do 75 minutes of vigorous-intensity aerobic exercise, or a mix of both. Also, include strength training exercises at least twice a week to boost heart health.
Before starting any new exercise, it’s important to talk to your healthcare provider. This is true, even if you have heart health concerns or other health issues.
Smoking Cessation and Alcohol Moderation
Quitting smoking is critical for those with chronic ischemic heart disease. Smoking can worsen the condition. Look into counseling and medication to find the best way to quit.
It’s also important to drink alcohol in moderation. Too much alcohol can harm heart health. Stick to moderate levels, up to one drink a day for women and up to two for men.
Stress Management Techniques
Chronic stress can harm heart health. Managing stress is key to managing chronic ischemic heart disease. Try meditation, yoga, or deep breathing exercises to reduce stress.
Doing things that bring joy and relaxation can also help manage stress. Explore different stress-reduction techniques to find what works best for you.
By making these lifestyle changes, people with chronic ischemic heart disease can actively manage their condition. While can ischemic heart disease be cured is complex, these changes can greatly impact the disease’s progression and improve quality of life. Understanding that is chronic ischemia serious highlights the importance of these lifestyle modifications.
Strategy 3: Pharmacological Management with Lipid-Lowering Therapies
Managing chronic ischemic heart disease (IHD) well depends on medicine, like lipid-lowering therapies. These treatments are key in cutting down heart disease risks. They help lower cholesterol and make plaques more stable.
Statin Therapy: Mechanisms and Benefits
Statins are a big help in fighting chronic IHD. They do more than just lower cholesterol. They also fight inflammation and make blood vessels work better. Statin therapy greatly cuts down on heart attacks and strokes.
Statins work by blocking HMG-CoA reductase. This reduces cholesterol made in the liver and boosts LDL receptor numbers. This makes it easier to remove LDL from blood.
Non-Statin Lipid-Lowering Agents
Statins are the first choice, but non-statin lipid-lowering agents like ezetimibe and PCSK9 inhibitors are also useful. They can be used with statins or for those who can’t take statins. These drugs help lower LDL-C and meet each patient’s needs.
Ezetimibe stops cholesterol absorption in the small intestine. PCSK9 inhibitors block PCSK9 from binding to LDL receptors. This increases LDL clearance.
Monitoring and Managing Side Effects
It’s important to watch for side effects when starting or taking lipid-lowering therapy. Common statin side effects include muscle pain and liver enzyme increases. Regular monitoring of liver tests and creatine kinase is key to spotting problems early.
To handle side effects, you might adjust the statin dose or switch to a different one. Adding CoQ10 can help with muscle issues. For those who can’t take statins, other treatments are available.
Strategy 4: Antiplatelet and Antithrombotic Therapy
Antiplatelet and antithrombotic therapy are key in preventing heart problems in patients with chronic heart disease. We will explore how aspirin and P2Y12 inhibitors work. We will also look at when to use anticoagulants and how long to keep up with these treatments.
Aspirin and P2Y12 Inhibitors
Aspirin is a mainstay in treating chronic heart disease because it stops platelets from sticking together. It does this by blocking the COX-1 enzyme, which reduces thromboxane A2 and platelet aggregation. The usual dose for heart protection is 75 mg to 100 mg a day. P2Y12 inhibitors, like clopidogrel, prasugrel, and ticagrelor, block the P2Y12 receptor on platelets. This prevents ADP from making platelets stick together.
Choosing between aspirin and P2Y12 inhibitors depends on the patient’s risk, how well they tolerate the drug, and their specific situation. Dual antiplatelet therapy (DAPT), combining aspirin with a P2Y12 inhibitor, is often used for those with acute coronary syndrome or after PCI. It helps lower the risk of stent thrombosis and heart problems.
Anticoagulation in Special Circumstances
In some cases, patients need anticoagulants in addition to antiplatelet drugs. This is true for those with atrial fibrillation, mechanical heart valves, or a high risk of blood clots. Anticoagulants like warfarin, apixaban, rivaroxaban, and dabigatran help prevent blood clots in these patients. The right anticoagulant depends on the patient’s kidney function, risk of bleeding, and other health issues.
Duration and Combination Strategies
How long to use antiplatelet and antithrombotic therapy is very important. For patients with stents, DAPT is usually recommended for 6 to 12 months. The time may be longer or shorter based on the patient’s risk of heart problems versus bleeding. Patients at high risk of bleeding might have DAPT for a shorter time. Those at high risk of heart problems might need longer DAPT or anticoagulation therapy.
Using both antiplatelet and anticoagulant therapies together needs careful thought. We must weigh the benefits of preventing heart problems against the risk of bleeding. It’s important to monitor for bleeding complications closely.
Strategy 5: Symptom Control with Beta-Blockers and Anti-Anginal Medications
Managing symptoms is key for those with chronic ischemic heart disease. Beta-blockers are a big help in this area. We’ll look at how these drugs, along with others, ease symptoms and better patient care.
Beta-Blockers: Mechanisms and Selection
Beta-blockers are a mainstay in treating chronic ischemic heart disease. They cut down on heart oxygen need by lowering heart rate and strength. This is key in easing angina symptoms. When picking a beta-blocker, we consider patient health, side effects, and drug specifics.
Some beta-blockers also open up blood vessels, which can help more patients. We start with proven drugs like metoprolol or bisoprolol. Then, we adjust based on how well the patient does and how they react.
Calcium Channel Blockers and Nitrates
Besides beta-blockers, calcium channel blockers and nitrates help with angina. Calcium blockers widen blood vessels and lower blood pressure. Nitrates, like nitroglycerin, quickly ease angina by reducing blood flow to the heart.
Choosing between these drugs depends on the patient’s symptoms, heart rate, and blood pressure. For example, calcium blockers might be better for those who can’t take beta-blockers.
Newer Anti-Anginal Agents
New drugs like ranolazine also help manage symptoms. Ranolazine cuts down on sodium in heart cells, easing ischemia without affecting heart rate or blood pressure much.
These new drugs are great for those who keep feeling symptoms even with usual treatments. They can be used with beta-blockers or as a substitute if needed.
Managing Medication Side Effects
It’s important to handle side effects to keep patients on their meds. Beta-blockers can cause fatigue, dizziness, and cold hands and feet. Calcium blockers might lead to swelling in legs and constipation. Nitrates can cause headaches and low blood pressure.
We watch for these side effects closely and adjust treatments as needed. This might mean changing doses, switching to a different drug, or adding something to counteract side effects.
Strategy 6: Novel Therapeutic Approaches with SGLT-2 Inhibitors and GLP-1 Receptor Agonists
SGLT-2 inhibitors and GLP-1 receptor agonists offer more than just diabetes management. They also bring cardiovascular benefits to patients with chronic ischemic heart disease. These new treatments have shown great promise in managing the condition and improving patient outcomes.
Cardiovascular Benefits Beyond Glycemic Control
These drugs were first made to control type 2 diabetes. But they do more than that. SGLT-2 inhibitors help lower the risk of heart attacks and strokes. GLP-1 receptor agonists reduce heart-related deaths and problems.
Their benefits are many:
- Lower blood pressure
- Better lipid profiles
- Improved endothelial function
- Anti-inflammatory effects
These advantages help manage chronic ischemic heart disease. So, SGLT-2 inhibitors and GLP-1 receptor agonists are valuable in treatment plans.
Patient Selection and Monitoring
Choosing the right patients for these treatments is key. We look at:
- Presence of type 2 diabetes
- History of cardiovascular disease
- Renal function
- Potential side effects
Monitoring patients involves checking:
- Renal function
- Electrolyte levels
- Glycemic control
- Cardiovascular events
Regular checks help adjust treatments for the best results.
Integration with Traditional Therapies
Combining these new treatments with traditional ones needs a detailed plan. We look at the patient’s current medicines, like:
- Statins
- Beta-blockers
- Antiplatelet agents
- ACE inhibitors or ARBs
Together, these therapies can offer more heart benefits while avoiding bad interactions. A tailored treatment plan is key to maximizing benefits for patients with chronic ischemic heart disease.
By adding these new treatments to care plans, we can give better care to patients with chronic ischemic heart disease. This improves their heart health and quality of life.
Strategy 7: Revascularization Strategies for Moderate to Severe Ischemia
Revascularization strategies are key for managing heart disease with moderate to severe ischemia. They help restore blood flow to the heart. This reduces symptoms and improves life quality.
Percutaneous Coronary Intervention (PCI)
Percutaneous Coronary Intervention (PCI) is a non-surgical way to open blocked heart arteries. PCI is very helpful for those with significant ischemia. It improves blood flow and lessens symptoms.
A study in Nature shows PCI benefits for chronic heart disease, mainly for those with moderate to severe ischemia.
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a surgery that bypasses blocked arteries with grafts. CABG is recommended for complex disease or when PCI doesn’t work.
| Procedure | Benefits | Risks |
|---|---|---|
| PCI | Minimally invasive, quick recovery | Risk of bleeding, stroke |
| CABG | Long-term benefits, suitable for complex disease | Surgical risks, longer recovery |
Decision-Making: Medical Therapy vs. Revascularization
Choosing between medical therapy and revascularization depends on several factors. These include ischemia severity, symptoms, and overall health. A heart team approach is used to make decisions.
Post-Procedure Management
After revascularization, patients need careful management. This includes monitoring for bleeding or thrombosis, managing medications, and promoting lifestyle changes.
Managing Chronic Ischemic Heart Failure: A Progressive Complication
Managing chronic ischemic heart failure needs a detailed plan to better patient outcomes and life quality. Heart failure is a serious step up from chronic ischemic heart disease. It calls for a change in how we treat it.
Recognizing the Transition to Heart Failure
It’s key to spot when heart disease turns into heart failure early. Signs like harder breathing, feeling very tired, and swelling in the legs mean heart failure might be coming. We watch for these signs closely and adjust treatment plans as needed.
Key indicators of heart failure progression include:
- Increased dyspnea on exertion
- Orthopnea or paroxysmal nocturnal dyspnea
- Elevated jugular venous pressure
- Peripheral edema
Guideline-Directed Medical Therapy for Ischemic Heart Failure
Guideline-directed medical therapy (GDMT) is key for managing ischemic heart failure. We follow guidelines that suggest a mix of medicines to help patients live longer and go to the hospital less.
GDMT typically includes:
- Angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor-neprilysin inhibitors (ARNI)
- Beta-blockers
- Mineralocorticoid receptor antagonists (MRA)
- Sodium-glucose cotransporter-2 inhibitors (SGLT2i) in appropriate patients
“The use of GDMT has been shown to significantly improve outcomes in patients with heart failure, reducing morbidity and mortality.”
Advanced Therapies for Refractory Cases
For those who keep feeling bad even with the best GDMT, we look at advanced treatments. These treatments aim to make the heart work better and improve life quality.
| Therapy | Description | Indications |
|---|---|---|
| Cardiac Resynchronization Therapy (CRT) | Device that coordinates heart contractions | Symptomatic patients with LBBB and LVEF ≤35% |
| Implantable Cardioverter-Defibrillator (ICD) | Device that prevents sudden cardiac death | Patients with LVEF ≤35% and high risk of ventricular arrhythmias |
Quality of Life Considerations
Boosting quality of life is a big part of managing chronic ischemic heart failure. We focus on managing symptoms, educating patients, and supporting them to improve their overall well-being.
Strategies to improve quality of life include:
- Personalized exercise programs
- Dietary counseling
- Psychological support
- Advanced care planning
Conclusion: Living with Chronic Ischemic Heart Disease
Managing chronic ischemic heart disease (IHD) is key to better health and life quality. We’ve shared a detailed plan that includes lifestyle changes, medicines, and procedures to fix blocked arteries. Each patient needs a unique plan to manage their disease well.
By making healthy lifestyle choices, taking medicines as directed, and getting procedures when needed, patients can lower their risk of serious problems. Managing chronic heart disease is a continuous effort. It needs regular check-ups and changes to the treatment plan as needed.
We aim to give patients the tools and support they need to manage their disease well. This way, they can live active and meaningful lives. With the right approach, people with chronic ischemic heart disease can achieve great health outcomes and a better quality of life.
FAQ
What is chronic ischemic heart disease?
Chronic ischemic heart disease, also known as stable ischemic heart disease (SIHD), is a condition. It happens when blood flow to the heart is reduced. This is due to coronary artery disease, leading to symptoms like angina.
How does chronic ischemic heart disease differ from acute coronary syndrome?
Chronic ischemic heart disease is a stable condition with predictable symptoms. On the other hand, acute coronary syndrome is an acute event like a heart attack. It often needs immediate medical attention.
What are the key strategies for managing chronic ischemic heart disease?
Managing chronic ischemic heart disease involves several key strategies. These include a thorough risk assessment and diagnosis. Lifestyle changes, like diet and exercise, are also important.
Pharmacological management with lipid-lowering therapies is key. Antiplatelet and antithrombotic therapy help control symptoms. Revascularization strategies are used for moderate to severe ischemia.
What lifestyle modifications are recommended for managing chronic ischemic heart disease?
Lifestyle modifications are essential. These include dietary changes for heart health and regular physical activity. Quitting smoking and managing stress are also important.Moderation in alcohol consumption is recommended.
What is the role of lipid-lowering therapies in managing chronic ischemic heart disease?
Lipid-lowering therapies, like statins and non-statin agents, are vital. They help reduce the risk of cardiovascular events. They lower cholesterol levels and manage other lipid-related risk factors.
How is antiplatelet and antithrombotic therapy used in chronic ischemic heart disease management?
Antiplatelet therapy, such as aspirin and P2Y12 inhibitors, prevents blood clots. Anticoagulation therapy may be used in special cases. It further reduces the risk of thrombotic events.
What are the benefits of SGLT-2 inhibitors and GLP-1 receptor agonists in chronic ischemic heart disease?
SGLT-2 inhibitors and GLP-1 receptor agonists offer benefits beyond controlling blood sugar. They reduce the risk of major cardiovascular events. They may also improve heart failure outcomes.
When is revascularization considered for chronic ischemic heart disease?
Revascularization strategies, like PCI or CABG, are considered for those with moderate to severe ischemia. They are for patients who remain symptomatic despite optimal medical therapy.
How is chronic ischemic heart failure managed?
Managing chronic ischemic heart failure involves recognizing the transition to heart failure. It includes implementing guideline-directed medical therapy. Advanced therapies are considered for refractory cases.Quality of life considerations are also important.
Can ischemic heart disease be cured?
Ischemic heart disease cannot be “cured” in the traditional sense. But, effective management can significantly improve symptoms. It reduces the risk of complications and enhances quality of life.
Is chronic ischemia serious?
Yes, chronic ischemia is serious. It can lead to significant morbidity, including angina, heart failure, and increased risk of myocardial infarction.
What are the types of ischemic heart disease?
Ischemic heart disease includes various conditions. These include stable ischemic heart disease (SIHD), acute coronary syndrome (ACS), and chronic ischemic heart failure. Each has distinct characteristics and management strategies.
Reference:
- “2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease” – Circulation.
- https://www.ncbi.nlm.nih.gov/pubmed/37471501 (ncbi.nlm.nih.gov) (PubMed)
- “2024 ESC Guidelines for the management of chronic coronary syndromes” – European Heart Journal. https://academic.oup.com/eurheartj/article/45/36/3415/7743115 (academic.oup.com) (OUP Academic)
- “Chronic Ischemic Heart Disease: Selection of Treatment Modality” – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507703/ (ncbi.nlm.nih.gov) (NCBI)
“What has changed in the management of chronic ischaemic heart disease” – European Heart Journal Supplements. https://academic.oup.com/eurheartjsupp/article/27/Supplement_3/iii83/8114513 (academic.oup.com) (OUP Academic)





