Last Updated on November 27, 2025 by Bilal Hasdemir

When a heart attack occurs, prompt treatment is crucial to minimize damage to the heart muscle. At Liv Hospital, we prioritize restoring blood flow quickly to prevent lifelong complications. Our trusted protocols and patient-focused care deliver world-class outcomes with the latest heart attack treatment options.
Effective hospital protocols include a range of medications, interventions, and rehabilitation programs tailored to each patient’s needs. Our mission is to provide comprehensive care that addresses the unique requirements of international patients seeking advanced medical treatments.
Key Takeaways
- Prompt treatment is essential to minimize heart muscle damage during a heart attack.
- Liv Hospital’s protocols include medications, interventions, and rehabilitation programs.
- Our patient-focused care delivers world-class outcomes with the latest treatment options.
- We provide comprehensive support for international patients.
- Restoring blood flow quickly is a top priority in heart attack treatment.
Understanding Heart Attacks: What Happens to Your Heart
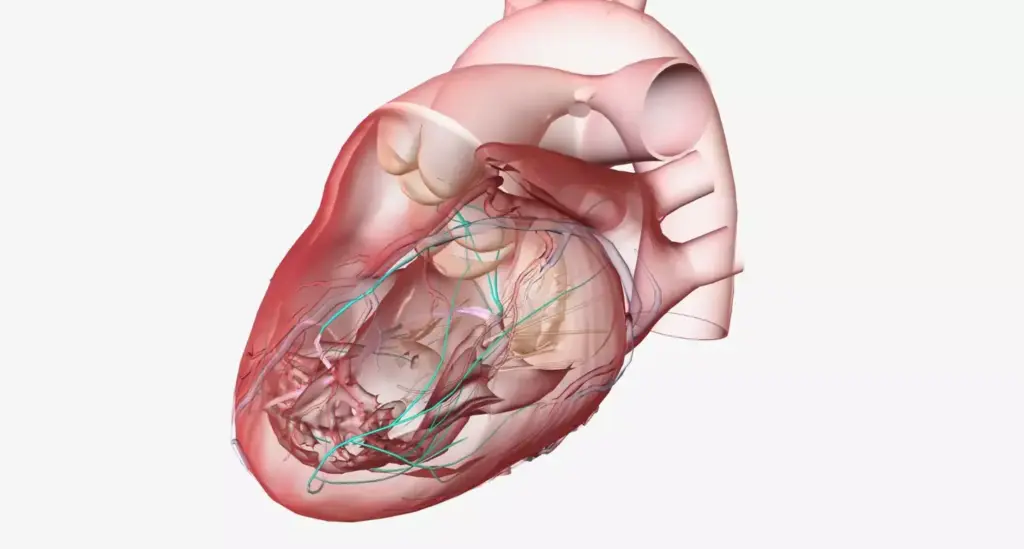
Understanding what happens during a heart attack is crucial for recognizing the symptoms and seeking timely medical intervention. A heart attack, medically known as myocardial infarction, occurs when the blood flow to a part of the heart is blocked, often by a blood clot, damaging or destroying the heart muscle.
The Physiology of a Myocardial Infarction
During a myocardial infarction, the blockage of a coronary artery restricts blood flow to the heart muscle, leading to tissue damage or death. This process involves complex physiological changes, including the release of various biochemical markers into the bloodstream, such as troponins, which are critical for diagnosing a heart attack.
The extent of the damage depends on the duration of the blockage and the area of the heart affected. Prompt medical treatment is essential to restore blood flow and minimize damage.
Types of Heart Attacks and Their Severity
Heart attacks are categorized based on the severity and location of the blockage. The most common type is a STEMI (ST-Elevation Myocardial Infarction), where a major coronary artery is completely blocked. Another type is NSTEMI (Non-ST-Elevation Myocardial Infarction), where the blockage is partial. Understanding these types helps in determining the appropriate treatment of a heart attack.
The severity of a heart attack can vary significantly among individuals, influenced by factors such as the presence of other health conditions and the promptness of medical care received.
Risk Factors and Warning Signs
Recognizing the risk factors and warning signs of a heart attack is vital for early intervention. Common risk factors include high blood pressure, high cholesterol, diabetes, smoking, and a family history of heart disease. Warning signs often include chest pain or discomfort, shortness of breath, nausea, and fatigue.
Being aware of these indicators can significantly impact the effectiveness of the heart attack treatment by ensuring that medical help is sought promptly.
The Critical Golden Hour: Why Immediate Treatment Matters
The golden hour following a heart attack is a critical period that determines the effectiveness of treatment and patient survival. During this time, timely medical intervention can significantly improve outcomes by minimizing damage to the heart muscle.
Time-to-Treatment Impact on Survival Rates
The time elapsed between the onset of heart attack symptoms and the initiation of treatment is a crucial factor in determining patient survival rates. Studies have shown that early treatment can reduce mortality rates and improve long-term outcomes. We illustrate this with a table showing the impact of time-to-treatment on survival rates.
| Time to Treatment | Survival Rate |
|---|---|
| Within 1 hour | 90% |
| 1-2 hours | 80% |
| 2-3 hours | 70% |
| More than 3 hours | 50% |
As shown in the table, prompt medical attention within the first hour significantly enhances survival chances. This underscores the importance of recognizing symptoms early and activating emergency services promptly.
Recognizing Symptoms and Activating Emergency Services
Recognizing the symptoms of a heart attack is the first step towards timely treatment. Common symptoms include chest pain, shortness of breath, nausea, and fatigue. It’s crucial for individuals to be aware of these symptoms and to call emergency services immediately if they or someone else is experiencing them.
“Acting FASTER when you or someone else is having a heart attack can mean the difference between life and death.”
Upon recognizing symptoms, activating emergency services by calling the local emergency number is the recommended course of action. Emergency responders are trained to provide pre-hospital care and transport patients to appropriate medical facilities.
Pre-Hospital Care and Transport Considerations
Pre-hospital care plays a vital role in the initial management of heart attack patients. Emergency medical technicians (EMTs) and paramedics are trained to provide life-saving interventions, including administering medications and using defibrillators if necessary.
When transporting patients, considerations include the proximity to the nearest cardiac catheterization laboratory and the availability of advanced cardiac care. The goal is to minimize delays and ensure that patients receive appropriate treatment as quickly as possible.
By understanding the importance of the golden hour and the steps involved in immediate treatment, we can improve outcomes for heart attack patients. Prompt recognition of symptoms, swift activation of emergency services, and efficient pre-hospital care are all critical components of effective heart attack management.
How Can You Treat a Heart Attack: The Initial Emergency Response
Effective treatment for a heart attack begins with understanding the immediate steps taken during an emergency. When someone experiences a heart attack, the initial response is critical in determining the outcome.
First Medical Contact Assessment Protocol
The first medical contact is a crucial moment in treating a heart attack. Emergency medical services (EMS) personnel are trained to quickly assess the situation and provide initial care. The first medical contact assessment protocol involves evaluating the patient’s symptoms, medical history, and performing an electrocardiogram (ECG) to determine the severity of the heart attack.
We use the MONA protocol – Morphine, Oxygen, Nitroglycerin, and Aspirin – as part of the initial assessment and treatment. This protocol helps in alleviating pain, improving oxygenation, and reducing the workload on the heart.
Immediate Stabilization Techniques
Immediate stabilization techniques are vital in managing a heart attack. These include administering oxygen therapy to patients with low oxygen saturation, providing cardiac monitoring to track the heart’s activity, and giving aspirin to prevent further clotting.
- Administering oxygen therapy
- Providing cardiac monitoring
- Giving aspirin
- Using nitroglycerin for pain relief
Diagnostic Procedures in the Emergency Department
Upon arrival at the emergency department, a series of diagnostic procedures are conducted to assess the heart attack’s severity. These include:
| Diagnostic Procedure | Purpose |
|---|---|
| Electrocardiogram (ECG) | To assess the heart’s electrical activity |
| Blood Tests | To measure cardiac biomarkers like troponin |
| Imaging Tests (e.g., echocardiogram) | To evaluate heart function and structure |
These diagnostic procedures help healthcare providers determine the best course of treatment for the patient.
Protocol 1: Medication Therapy for Acute Myocardial Infarction
The management of acute myocardial infarction relies heavily on effective medication therapy. Medications play a crucial role in heart attack treatment, aiming to restore blood flow, reduce damage to the heart muscle, and prevent further complications.
Aspirin and Its Immediate Benefits
Aspirin is one of the first medications administered during a heart attack. It works by inhibiting platelet aggregation, thereby reducing clot formation. The immediate benefits of aspirin include its ability to prevent further clotting and reduce the risk of another heart attack. We recommend a chewable aspirin to enhance absorption.
The use of aspirin has been a cornerstone in heart attack treatment due to its:
- Antiplatelet effects
- Ability to reduce mortality when given early
- Wide availability and low cost
Thrombolytic (Clot-Busting) Medications
Thrombolytic medications, also known as clot-busting drugs, are used to dissolve the clot causing the heart attack. These medications are most effective when administered promptly after the onset of symptoms. We use thrombolytic therapy when primary percutaneous coronary intervention (PCI) is not readily available.
The benefits of thrombolytic medications include:
- Restoring blood flow in the occluded artery
- Reducing mortality and improving outcomes
- Being a viable alternative when PCI is not available
Anticoagulants and Antiplatelets
In addition to aspirin, other anticoagulants and antiplatelets are used to prevent further clot formation. These include medications like heparin, clopidogrel, and ticagrelor. The combination of these medications helps in reducing the risk of further cardiac events.
Anticoagulants and antiplatelets work by:
- Inhibiting the coagulation cascade
- Preventing platelet activation and aggregation
- Reducing the risk of re-infarction
Pain Management and Anxiety Control
Pain management is crucial during a heart attack, as it helps in reducing anxiety and the workload on the heart. We use medications like morphine to manage pain and anxiety. Effective pain management also helps in reducing the sympathetic drive, thus decreasing the heart’s oxygen demand.
The goals of pain management include:
- Reducing discomfort and anxiety
- Decreasing the heart rate and blood pressure
- Improving overall patient comfort and outcomes
By understanding and utilizing these medication therapies, we can significantly improve outcomes for patients suffering from acute myocardial infarction.
Protocol 2: Advanced Cardiac Medications
The use of advanced cardiac medications is a critical component of heart attack treatment protocols. These medications are designed to address various aspects of heart attack management, from protecting the heart muscle to stabilizing arterial plaques.
Beta Blockers: Protecting the Heart Muscle
Beta blockers are a cornerstone in the management of heart attack patients. They work by reducing the workload on the heart, thus lowering the demand for oxygen and minimizing damage to the heart muscle. By slowing the heart rate and reducing the force of contraction, beta blockers help in preserving the heart’s function during and after a heart attack.
ACE Inhibitors: Preserving Heart Function
ACE inhibitors are another crucial class of medications used in the treatment of heart attacks. They help in relaxing blood vessels, which improves blood flow and reduces the strain on the heart. This action not only aids in the immediate management of heart attack but also supports long-term heart health.
Statins: Stabilizing Arterial Plaques
Statins play a vital role in stabilizing arterial plaques, which are fatty deposits that can rupture and cause a heart attack. By lowering cholesterol levels, statins reduce the risk of further plaque buildup and rupture. The early initiation of statins has been shown to significantly improve outcomes in heart attack patients.
Timing and Administration of Medication Combinations
The timing and administration of these advanced cardiac medications are critical. Healthcare providers carefully consider the combination and dosage of these medications to maximize their benefits while minimizing potential side effects. The goal is to provide a comprehensive treatment plan that addresses the immediate needs of the patient while also considering long-term recovery and prevention of future heart-related events.
In conclusion, advanced cardiac medications, including beta blockers, ACE inhibitors, and statins, form a crucial part of heart attack treatment protocols. Their appropriate use, in terms of timing and combination, is vital for optimizing patient outcomes.
Protocol 3: Percutaneous Coronary Intervention (PCI)
The gold standard for treating STEMI, percutaneous coronary intervention (PCI), has become a cornerstone in heart attack treatment protocols worldwide. PCI is a lifesaving procedure that involves the use of a catheter to open blocked coronary arteries, thereby restoring blood flow to the heart muscle.
Primary PCI: The Gold Standard for STEMI
Primary PCI is the preferred treatment for patients with ST-elevation myocardial infarction (STEMI), a type of heart attack where a major coronary artery is completely blocked. We have seen significant improvements in patient outcomes when primary PCI is performed promptly.
Benefits of Primary PCI include reduced mortality rates, decreased risk of re-infarction, and improved left ventricular function. It’s a testament to the advancements in interventional cardiology that have made PCI a reliable and effective treatment for heart attacks.
Angioplasty and Stent Placement Procedures
During PCI, angioplasty is performed to widen the blocked artery. This involves inflating a balloon within the artery to push aside the plaque. Often, a stent is placed during the procedure to keep the artery open. We use advanced stent technologies, including drug-eluting stents, to minimize the risk of restenosis.
Door-to-Balloon Time Optimization
One of the critical factors in the success of PCI is the door-to-balloon time, which refers to the interval from the patient’s arrival at the hospital to the inflation of the balloon in the blocked artery. We strive to minimize this time to ensure the best possible outcomes for our patients.
Optimizing door-to-balloon time involves a coordinated effort from the emergency department, cardiology team, and catheterization laboratory staff. By streamlining our processes, we can significantly improve survival rates and reduce complications.
Recovery and Outcomes After PCI
After undergoing PCI, patients are closely monitored for any signs of complications. We have a comprehensive post-procedure care plan in place, which includes medication management, lifestyle counseling, and follow-up appointments to ensure a smooth recovery.
The outcomes after PCI are generally positive, with most patients experiencing significant improvements in their symptoms and quality of life. We continue to monitor our patients’ progress and adjust their treatment plans as necessary to achieve the best possible long-term outcomes.
Protocol 4: Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a critical surgical intervention for patients with complex coronary artery disease. This procedure involves bypassing blocked or partially blocked arteries with grafts, thereby restoring blood flow to the heart. We will outline the indications for CABG, the step-by-step procedure, post-surgical care, and the recovery process.
When Multiple Vessel Disease Requires Surgery
CABG is particularly recommended for patients with multiple vessel disease, where several coronary arteries are blocked. This condition often necessitates a more invasive approach than angioplasty or stenting. The decision to undergo CABG is typically made after a thorough evaluation, including coronary angiography and assessments of cardiac function.
According to a study published in the Journal of the American College of Cardiology, CABG has been shown to improve long-term survival in patients with complex multi-vessel coronary artery disease.
“CABG is associated with improved survival and reduced risk of major adverse cardiac events in patients with complex coronary artery disease.”
The CABG Procedure Step-by-Step
The CABG procedure involves several key steps:
- Preparation: The patient is prepared for surgery, which includes administering anesthesia and connecting the patient to a heart-lung machine.
- Graft Harvesting: Grafts are harvested from the patient’s leg (saphenous vein) or arm (radial artery), or taken from the internal thoracic artery.
- Bypass Grafting: The surgeon bypasses the blocked coronary arteries using the harvested grafts.
- Revascularization: The heart is revascularized, restoring blood flow to the affected areas.
Post-Surgical Care in the Cardiac ICU
After CABG, patients are closely monitored in the Cardiac Intensive Care Unit (CICU). Post-surgical care includes:
| Care Aspect | Description |
|---|---|
| Monitoring | Continuous monitoring of vital signs and cardiac function. |
| Pain Management | Effective pain management strategies are employed. |
| Respiratory Care | Support for breathing and respiratory function. |
Recovery Timeline and Rehabilitation Process
The recovery process after CABG involves several stages:
- Hospital Stay: Typically 5-7 days, during which the patient’s condition is stabilized.
- Early Recovery (0-6 weeks): Focus on wound healing and gradual increase in physical activity.
- Rehabilitation (6-12 weeks): Structured cardiac rehabilitation programs are initiated to improve cardiovascular health.
We emphasize the importance of adherence to the rehabilitation protocol to ensure optimal recovery and long-term health benefits. As part of the treatment options for heart attacks, CABG plays a vital role in managing complex coronary artery disease, improving survival rates, and enhancing the quality of life for patients.
Protocol 5: Advanced Monitoring and Critical Care
Advanced monitoring and critical care are crucial components of effective heart attack treatment. When a patient is admitted with a myocardial infarction, the care team springs into action, employing a range of strategies to monitor and manage their condition closely.
Continuous Cardiac Monitoring Systems
Continuous cardiac monitoring is a cornerstone of care in the acute phase of a heart attack. This involves the use of electrocardiogram (ECG) monitors to track the heart’s electrical activity in real-time. Continuous monitoring allows healthcare providers to quickly identify any changes in the patient’s condition, such as arrhythmias or signs of further ischemia. Modern monitoring systems are highly sophisticated, offering advanced algorithms to detect subtle changes that may not be apparent to the naked eye.
Hemodynamic Assessment and Management
Hemodynamic monitoring involves assessing the patient’s blood pressure, cardiac output, and other factors related to blood flow and circulation. This information is critical for managing the patient’s condition, as it helps clinicians to optimize fluid status, adjust medications, and make other necessary interventions. Hemodynamic assessment can be achieved through various methods, including invasive techniques like pulmonary artery catheters and non-invasive methods such as echocardiography.
Detecting and Managing Complications
Despite the best care, complications can arise in patients with heart attacks. Advanced monitoring systems play a key role in detecting these complications early, when they are most manageable. Common complications include heart failure, arrhythmias, and mechanical problems such as ventricular septal defect. Prompt detection and intervention are crucial to prevent these complications from becoming life-threatening.
| Monitoring Parameter | Normal Range | Significance in Heart Attack |
|---|---|---|
| Heart Rate | 60-100 bpm | Tachycardia or bradycardia can indicate stress or ischemia |
| Blood Pressure | 90/60 – 120/80 mmHg | Hypotension may suggest cardiogenic shock |
| Cardiac Output | 4-8 L/min | Low output can indicate heart failure |
In conclusion, advanced monitoring and critical care are essential elements of heart attack treatment protocols. By leveraging continuous cardiac monitoring systems, hemodynamic assessment, and prompt detection of complications, healthcare providers can significantly improve patient outcomes. The integration of these strategies into a comprehensive care plan is vital for optimizing recovery and reducing the risk of long-term cardiac damage.
Protocol 6: Cardiac Rehabilitation Programs
The journey to recovery after a heart attack often involves a structured cardiac rehabilitation program. Cardiac rehabilitation is essential for recovery and long-term health, offering a comprehensive approach that includes various therapies to help patients regain their health and prevent future heart issues.
Structured Exercise and Physical Therapy
Structured exercise and physical therapy are cornerstone components of cardiac rehabilitation programs. These programs are tailored to the individual patient’s needs and capabilities, aiming to improve cardiovascular health, strength, and endurance.
Nutritional Counseling and Heart-Healthy Diet
Nutritional counseling is another vital aspect, educating patients on heart-healthy diets that can help manage risk factors such as high cholesterol, hypertension, and diabetes. We work with patients to develop personalized dietary plans that promote overall cardiovascular health.
Psychological Support and Stress Management
Psychological support and stress management are also critical components. We provide patients with the tools and support needed to manage stress and anxiety, which are common after experiencing a heart attack. This support can include counseling, stress management techniques, and support groups.
Measuring Progress and Adjusting Rehabilitation Plans
Throughout the cardiac rehabilitation program, we continuously measure patient progress and adjust the rehabilitation plans as necessary. This ensures that the program remains effective and tailored to the patient’s evolving needs.
| Component | Description | Outcome |
|---|---|---|
| Structured Exercise | Tailored exercise programs to improve cardiovascular health | Improved endurance and strength |
| Nutritional Counseling | Personalized dietary plans to manage risk factors | Better management of cholesterol, hypertension, and diabetes |
| Psychological Support | Counseling and stress management techniques | Reduced stress and anxiety |
Cardiac rehabilitation programs are a multifaceted approach to recovery after a heart attack, incorporating structured exercise, nutritional counseling, psychological support, and continuous assessment. By participating in these programs, patients can significantly improve their long-term health outcomes and reduce the risk of future cardiac events.
Protocol 7: Long-Term Management and Secondary Prevention
Long-term management strategies play a vital role in improving the outcomes for heart attack survivors. Effective management involves a multifaceted approach that includes medication regimens, lifestyle changes, and regular monitoring to prevent future cardiac events.
Medication Regimens for Ongoing Heart Health
Medications are a cornerstone in the long-term management of heart attack patients. We typically prescribe a combination of drugs to manage conditions such as high blood pressure, high cholesterol, and to prevent blood clots. Aspirin, beta-blockers, ACE inhibitors, and statins are commonly used to achieve these goals.
The specific medication regimen can vary based on the individual patient’s condition and medical history. For instance, patients with a history of heart failure may require additional medications to manage their condition effectively.
Lifestyle Modifications and Risk Factor Control
Lifestyle changes are crucial for heart attack survivors to reduce the risk of future cardiac events. We recommend adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins. Regular physical activity, such as walking or other aerobic exercises, is also essential.
Additionally, quitting smoking and limiting alcohol consumption are vital lifestyle modifications. We work closely with patients to develop a personalized plan that suits their needs and preferences.
Regular Follow-up and Monitoring Protocols
Regular follow-up appointments are essential for monitoring the patient’s progress and adjusting treatment plans as necessary. We use various diagnostic tests, including echocardiograms and stress tests, to assess heart function and identify potential issues early.
These follow-up visits also provide an opportunity to address any concerns or questions the patient may have, ensuring they remain engaged in their care.
Evidence-Based Guidelines for Secondary Prevention
Our approach to secondary prevention is guided by the latest evidence-based guidelines. We adhere to recommendations from reputable organizations such as the American Heart Association and the American College of Cardiology.
These guidelines help us tailor our treatment strategies to the individual needs of each patient, ensuring they receive the most effective care possible.
Conclusion: The Integrated Approach to Heart Attack Treatment
We have explored various heart attack treatment options, from initial emergency response to long-term management and secondary prevention. Effective treatment for heart attacks requires a comprehensive and coordinated care approach, incorporating multiple protocols and interventions.
Heart attack treatment in hospital involves a range of strategies, including medication therapy, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG). By integrating these approaches, healthcare providers can significantly improve patient outcomes and quality of life.
Our discussion highlights the importance of a multidisciplinary team in delivering high-quality care. From the initial assessment to post-discharge rehabilitation, we work together to ensure that patients receive the best possible treatment for heart attacks.
By adopting an integrated approach to heart attack treatment, we can reduce morbidity and mortality, enabling patients to recover and lead active lives. This comprehensive strategy is crucial in providing world-class healthcare with complete support for international patients.
FAQ
What is the importance of prompt heart attack treatment in a hospital setting?
Prompt heart attack treatment in a hospital setting is crucial as it significantly improves patient outcomes by minimizing damage to the heart muscle. Timely interventions, such as medication therapy and percutaneous coronary intervention (PCI), can greatly enhance survival rates and reduce the risk of complications.
What are the different types of heart attacks and their severity?
There are several types of heart attacks, including ST-Elevation Myocardial Infarction (STEMI), Non-ST Elevation Myocardial Infarction (NSTEMI), and unstable angina. The severity of a heart attack depends on the extent of damage to the heart muscle and the promptness of treatment.
What are the risk factors and warning signs of a heart attack?
Common risk factors for heart attacks include high blood pressure, high cholesterol, diabetes, smoking, and family history. Warning signs may include chest pain or discomfort, shortness of breath, nausea, fatigue, and pain or discomfort in the arms, back, neck, jaw, or stomach.
How does immediate treatment impact survival rates during a heart attack?
Immediate treatment during a heart attack significantly improves survival rates by restoring blood flow to the heart muscle, reducing damage, and preventing further complications. The critical golden hour following a heart attack is crucial, and timely medical attention can greatly enhance patient outcomes.
What is the role of percutaneous coronary intervention (PCI) in heart attack treatment?
PCI is a minimally invasive procedure used to open blocked coronary arteries and restore blood flow to the heart muscle. It is considered the gold standard for STEMI and is often used in conjunction with medication therapy to improve patient outcomes.
What medications are used to treat acute myocardial infarction?
Medications used to treat acute myocardial infarction include aspirin, thrombolytic medications, anticoagulants, antiplatelets, beta blockers, ACE inhibitors, and statins. These medications help to restore blood flow, reduce pain, and prevent further complications.
What is cardiac rehabilitation, and how does it support heart attack recovery?
Cardiac rehabilitation is a comprehensive program that includes structured exercise, physical therapy, nutritional counseling, psychological support, and stress management. It is designed to help patients recover from heart attacks, improve their overall health, and reduce the risk of future cardiac events.
What lifestyle modifications can help prevent future heart attacks?
Lifestyle modifications that can help prevent future heart attacks include maintaining a healthy diet, exercising regularly, quitting smoking, managing stress, and controlling risk factors such as high blood pressure and high cholesterol.
How can patients manage their condition after a heart attack?
Patients can manage their condition after a heart attack by adhering to their medication regimen, attending regular follow-up appointments, making lifestyle modifications, and participating in cardiac rehabilitation programs.
What is the importance of long-term management and secondary prevention after a heart attack?
Long-term management and secondary prevention are crucial after a heart attack to prevent future cardiac events and improve patient outcomes. This includes ongoing medication therapy, lifestyle modifications, and regular monitoring to control risk factors and detect any potential complications.
References:
• NHLBI, NIH. (n.d.). Heart attack – Treatment. https://www.nhlbi.nih.gov/health/heart-attack/treatment
• NHS. (n.d.). Treatments for heart attack. https://www.nhs.uk/conditions/heart-attack/treatment/





