Last Updated on November 27, 2025 by Bilal Hasdemir

Understanding the meaning of MI in medical terms is crucial for anyone concerned about heart health. At Liv Hospital, we emphasize the importance of accurate medical terminology for effective patient care. MI stands for myocardial infarction, a condition where the heart muscle is damaged due to a lack of blood supply.
We recognize the significance of MI and its implications for patient care. With our advanced treatment standards and trusted approach, learning about MI could be the key to life-saving decisions for yourself or loved ones.
Key Takeaways
- MI stands for myocardial infarction, a serious heart condition.
- Myocardial infarction occurs when the heart muscle is damaged due to lack of blood supply.
- Understanding MI is vital for effective patient care and treatment.
- Liv Hospital provides world-class healthcare with advanced treatment standards.
- Accurate medical terminology is crucial for patient care and communication.
Understanding MI: Myocardial Infarction Defined
Myocardial Infarction, commonly referred to as MI, is a serious medical condition that affects millions worldwide. It is essential to understand what MI stands for in medical terms to grasp the severity of a heart attack and its implications on cardiovascular health.
The Medical Definition of MI
Myocardial Infarction is defined as the damage and death of heart muscle cells due to a blockage of a coronary artery, which supplies blood to the heart. This blockage can lead to a heart attack, commonly known as an MI. The medical community uses the term MI to describe this specific condition because it precisely indicates the infarction (death) of heart muscle tissue.
The Heart Attack Connection
The terms “Myocardial Infarction” and “heart attack” are often used interchangeably, but they essentially refer to the same condition. A heart attack occurs when the flow of blood to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies. Understanding the connection between MI and heart attacks is crucial for recognizing the warning signs and seeking timely medical intervention.
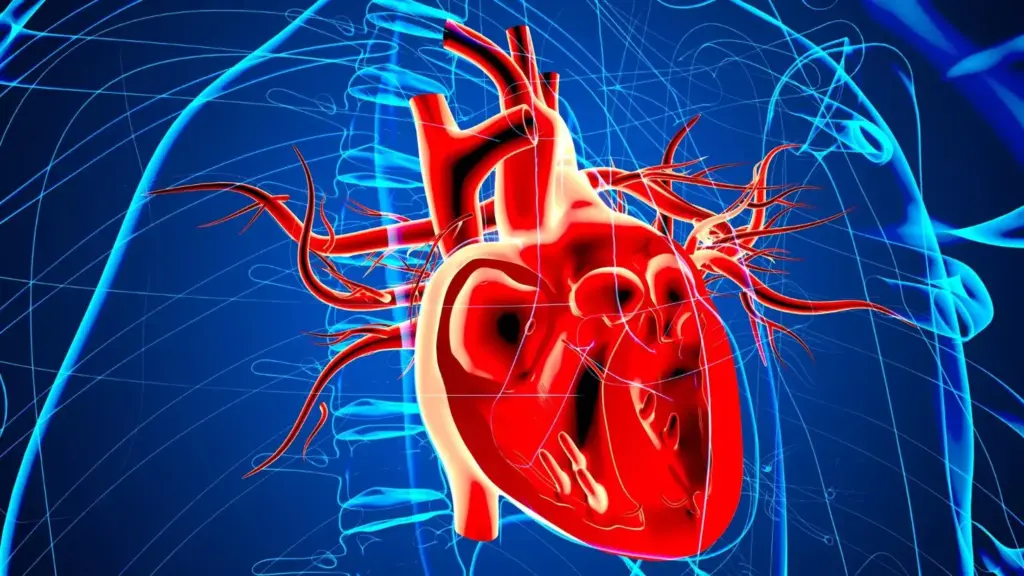
Cardiovascular System Basics
The cardiovascular system, comprising the heart and blood vessels, is responsible for transporting oxygen and nutrients to tissues and removing waste products. The heart, a muscular organ, pumps blood throughout the body. When an MI occurs, it disrupts this critical function, potentially leading to severe complications if not promptly treated. We will explore the intricacies of the cardiovascular system and how MI affects it in subsequent sections.
What Does MI Stand for in Medical Terms: Primary and Alternative Meanings

The abbreviation MI is widely used in medical practice, but its meaning can vary depending on the context. In this section, we will explore the primary and alternative meanings of MI in medical terms, providing clarity on its usage and significance.
Myocardial Infarction as the Primary Meaning
Myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow to the heart is severely blocked, causing damage to the heart muscle due to lack of oxygen. This condition is a medical emergency requiring immediate attention. The term MI is predominantly used in cardiology to describe this specific condition.
Other Medical Uses of the MI Abbreviation
While myocardial infarction is the most common interpretation of MI, there are other medical uses of this abbreviation. For instance, in some contexts, MI can refer to mitral insufficiency or myocardial ischemia. Understanding the specific context in which MI is used is crucial for accurate interpretation.
Context-Dependent Interpretations in Clinical Settings
In clinical settings, the meaning of MI can shift based on the department or the specific condition being treated. For example, in cardiology, MI typically refers to myocardial infarction. However, in other departments, it might have different implications. Healthcare professionals must be aware of these variations to provide accurate care.
We recognize that clarity in medical terminology is essential for effective patient care and communication among healthcare providers. By understanding the various meanings of MI and their contexts, medical professionals can ensure they are providing the most accurate diagnoses and treatments.
The Pathophysiology of Myocardial Infarction
Coronary artery disease and atherosclerosis play significant roles in the development of myocardial infarction (MI). Understanding the pathophysiology of MI is crucial for grasping how this condition affects the heart and for developing effective treatment strategies.
Coronary Artery Disease and Atherosclerosis
Coronary artery disease is characterized by the narrowing or blockage of the coronary arteries due to atherosclerosis. Atherosclerosis is a condition where plaque builds up in the arterial walls, leading to their hardening and narrowing. This process restricts blood flow to the heart muscle, setting the stage for an MI.
The development of atherosclerosis involves the accumulation of lipids, inflammatory cells, and fibrous elements in the arterial walls. Over time, this can lead to the formation of atherosclerotic plaques, which are susceptible to rupture.
The Process of Plaque Rupture and Thrombosis
Plaque rupture is a critical event in the pathophysiology of MI. When an atherosclerotic plaque ruptures, it exposes highly thrombogenic material to the bloodstream, leading to the formation of a thrombus. This thrombus can occlude the coronary artery, completely blocking blood flow to a portion of the heart muscle.
The resulting ischemia (lack of oxygen) causes damage to the heart muscle cells, leading to cell death if the ischemia is prolonged. This is the essence of an MI, or heart attack.
Cellular Damage During an MI
During an MI, the lack of blood flow to the heart muscle leads to cellular damage and necrosis. The extent of the damage depends on several factors, including the duration of ischemia, the area of the heart affected, and the presence of collateral circulation.
Understanding the cellular damage during an MI is vital for appreciating the importance of prompt medical intervention. Early treatment can significantly reduce the extent of damage and improve outcomes for patients.
By recognizing the warning signs of an MI and understanding its pathophysiology, we can better manage and prevent this potentially life-threatening condition.
Types of Myocardial Infarction: STEMI vs. NSTEMI
When it comes to myocardial infarction, or MI, there are two main types that healthcare professionals focus on: STEMI and NSTEMI. Understanding the differences between these two conditions is crucial for providing appropriate care.
ST-Elevation Myocardial Infarction (STEMI)
A STEMI occurs when there is a complete blockage of a coronary artery, leading to significant damage to the heart muscle. This type of MI is characterized by ST-segment elevation on an electrocardiogram (ECG).
Key characteristics of STEMI include:
- Complete occlusion of a coronary artery
- ST-segment elevation on ECG
- High risk of significant heart muscle damage
Non-ST-Elevation Myocardial Infarction (NSTEMI)
NSTEMI, on the other hand, involves a partial blockage of a coronary artery. While it is still a serious condition, the damage to the heart muscle may be less extensive compared to STEMI.
NSTEMI is characterized by:
- Partial occlusion of a coronary artery
- Absence of ST-segment elevation on ECG
- Elevated cardiac biomarkers indicating heart damage
Clinical Differences and Treatment Approaches
The distinction between STEMI and NSTEMI is not just semantic; it has significant implications for treatment. While both conditions require immediate medical attention, the approach to care can differ.
| Characteristics | STEMI | NSTEMI |
|---|---|---|
| Coronary Artery Occlusion | Complete | Partial |
| ECG Findings | ST-segment elevation | No ST-segment elevation |
| Typical Treatment Approach | Immediate reperfusion therapy (e.g., PCI) | Initial stabilization, then consider invasive strategies |
We understand that navigating the complexities of myocardial infarction can be challenging. By recognizing the differences between STEMI and NSTEMI, healthcare providers can tailor their approach to meet the specific needs of each patient, ultimately improving outcomes.
Risk Factors and Prevention of Myocardial Infarction
The prevention of myocardial infarction (MI) relies heavily on understanding its risk factors and taking proactive measures. Myocardial infarction, commonly referred to as a heart attack, occurs when the flow of blood to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies. This is most often caused by a blockage in one or more of the coronary arteries due to plaque (a mix of fat, cholesterol, and other substances).
Modifiable Risk Factors
Several risk factors for MI can be modified through lifestyle changes or medical interventions. These include:
- Smoking: Smoking is a significant risk factor for MI as it damages the inner lining of blood vessels, making them more susceptible to blockage.
- High Blood Pressure: Hypertension can cause damage to the arteries, making them more prone to narrowing and blockage.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in arteries.
- Diabetes: Diabetes mellitus increases the risk of MI due to its effects on blood vessels and nerves that control the heart.
- Obesity and Physical Inactivity: Being overweight and lack of physical activity can contribute to other risk factors like high blood pressure, high cholesterol, and diabetes.
Managing these modifiable risk factors through lifestyle changes and, when necessary, medication can significantly reduce the risk of MI.
Non-Modifiable Risk Factors
While some risk factors cannot be changed, being aware of them can help in taking preventive measures. Non-modifiable risk factors include:
- Age: The risk of MI increases with age.
- Gender: Men are generally at higher risk of MI than women, although the risk for women increases after menopause.
- Family History: A family history of heart disease can increase an individual’s risk.
Primary and Secondary Prevention Strategies
Prevention strategies for MI can be categorized into primary and secondary prevention.
| Prevention Type | Description | Strategies |
|---|---|---|
| Primary Prevention | Aim to prevent the first occurrence of MI | Lifestyle modifications (diet, exercise, smoking cessation), managing risk factors (hypertension, diabetes) |
| Secondary Prevention | Focus on preventing another MI in individuals who have already experienced one | Medications (antiplatelets, beta-blockers, statins), cardiac rehabilitation, lifestyle changes |
Understanding what MI stands for in medical terms and its associated risk factors is crucial for both primary and secondary prevention. By managing modifiable risk factors and being aware of non-modifiable ones, individuals can significantly reduce their risk of experiencing a myocardial infarction.
Recognizing the Warning Signs of an MI
Recognizing the symptoms of an MI can significantly impact patient outcomes and survival rates. Myocardial infarction, commonly known as a heart attack, occurs when blood flow to the heart is severely blocked, causing damage to the heart muscle. We will outline the classic and atypical symptoms associated with MI and emphasize the importance of seeking immediate medical attention.
Classic Symptoms of a Heart Attack
The most common symptoms of a heart attack include chest pain or discomfort, often described as a feeling of pressure, tightness, or heaviness in the center or left side of the chest. This pain can radiate to the arms, back, neck, jaw, or stomach. Other classic symptoms include shortness of breath, cold sweats, nausea or vomiting, and lightheadedness or dizziness.
It’s crucial to understand that not everyone experiences all of these symptoms, and their severity can vary from person to person. Some individuals may have a mild heart attack with minimal symptoms, while others may have a more severe attack with multiple symptoms.
Atypical Presentations: Gender and Age Differences
Atypical symptoms of MI can occur and are more common in certain populations, such as women, older adults, and people with diabetes. Women, for instance, are more likely to experience atypical symptoms like sharp, stabbing pains rather than the classic pressure or heaviness. Older adults may present with confusion, fatigue, or weakness rather than chest pain.
Understanding these differences is vital for healthcare providers to make accurate diagnoses and provide appropriate care. It’s also essential for the general public to be aware of these variations to seek medical help promptly.
When to Seek Emergency Medical Attention
If you or someone else is experiencing symptoms of a heart attack, it’s critical to act quickly. Call emergency services or your local emergency number immediately. Do not attempt to drive to the hospital unless absolutely necessary.
While waiting for help to arrive, chew and swallow an aspirin if advised by your emergency operator or if you’re not allergic to aspirin. Aspirin can help prevent further clotting.
Prompt medical attention can significantly improve outcomes for individuals experiencing an MI. We encourage everyone to be aware of the warning signs and to take immediate action if they or someone they know is experiencing these symptoms.
Diagnosing an MI: Medical Tests and Procedures
The diagnosis of myocardial infarction (MI) is multifaceted, involving several key medical tests and procedures. When a patient presents with symptoms suggestive of a heart attack, healthcare providers employ a range of diagnostic tools to confirm the diagnosis and guide treatment.
Electrocardiogram (ECG) Changes
One of the initial steps in diagnosing MI is performing an electrocardiogram (ECG). This test records the electrical activity of the heart, providing crucial information about the heart’s rhythm and potential damage to the heart muscle. ECG changes can indicate the presence of an MI, with specific patterns such as ST-segment elevation being characteristic of certain types of myocardial infarction.
ST-segment elevation on an ECG is a hallmark of STEMI (ST-Elevation Myocardial Infarction), a type of MI where a major coronary artery is completely blocked. Other ECG changes, such as Q-waves and T-wave inversion, can also provide evidence of myocardial damage.
Cardiac Biomarkers: Troponin and Beyond
In addition to ECG, cardiac biomarkers play a critical role in diagnosing MI. Troponin is a protein found in cardiac muscle cells, and its release into the bloodstream is a sensitive indicator of heart damage. Elevated troponin levels are a key diagnostic criterion for MI. Other biomarkers, such as creatine kinase-MB (CK-MB), may also be measured to support the diagnosis.
The measurement of these biomarkers, particularly troponin, has become a cornerstone in the diagnosis of MI, offering high sensitivity and specificity for myocardial injury.
Imaging Studies for Confirming MI
While ECG and cardiac biomarkers are primary diagnostic tools, imaging studies can provide additional information to confirm the diagnosis and assess the extent of cardiac damage. Techniques such as echocardiography and cardiac magnetic resonance imaging (MRI) can visualize the heart’s structure and function, helping to identify areas of damaged myocardium.
These imaging modalities are particularly useful in cases where the diagnosis remains uncertain after initial testing or when assessing the long-term impact of an MI on cardiac function.
Acute Management of Myocardial Infarction
The acute management of myocardial infarction (MI) is a critical aspect of cardiovascular care that requires immediate and effective intervention. When a patient presents with symptoms of MI, timely medical response is crucial to minimize cardiac damage and improve survival rates.
Emergency Interventions
Upon diagnosis of MI, several emergency interventions are initiated. These include:
- Administering aspirin to prevent further clotting
- Providing oxygen therapy to increase oxygen supply to the heart
- Using nitroglycerin to relieve chest pain and reduce the heart’s workload
- Activating the cardiac catheterization laboratory for potential reperfusion
Reperfusion Strategies
Reperfusion strategies are critical in restoring blood flow to the affected area of the heart. The primary methods include:
- Primary percutaneous coronary intervention (PCI): A mechanical intervention to open the blocked artery
- Fibrinolytic therapy: Using medications to dissolve the clot when PCI is not readily available
Both methods have their indications and are chosen based on the patient’s condition and the available medical facilities.
Medications in the Acute Phase
In addition to emergency interventions and reperfusion strategies, various medications play a crucial role in the acute management of MI. These include:
- Antiplatelet agents like clopidogrel to prevent new clot formation
- Anticoagulants such as heparin to prevent clot extension
- Beta-blockers to reduce the heart rate and myocardial oxygen demand
- ACE inhibitors or ARBs to reduce blood pressure and decrease the strain on the heart
These medications, along with lifestyle modifications, form the cornerstone of MI management in the acute phase, aiming to reduce morbidity and mortality.
Long-term Treatment and Rehabilitation After MI
After experiencing a myocardial infarction (MI), patients enter a critical phase of recovery that requires comprehensive long-term treatment and rehabilitation. This phase is crucial for improving survival rates, reducing the risk of further cardiovascular events, and enhancing the patient’s quality of life. We will outline the key components of long-term care for MI patients, including medication regimens, cardiac rehabilitation programs, and necessary lifestyle modifications.
Medication Regimens Post-MI
Medication plays a vital role in the long-term management of MI patients. The primary goals of pharmacotherapy are to reduce the risk of further MIs, manage symptoms, and improve survival. Commonly prescribed medications include:
- Antiplatelet agents to prevent blood clots
- Beta-blockers to reduce heart rate and blood pressure
- ACE inhibitors or ARBs to manage blood pressure and reduce strain on the heart
- Statins to lower cholesterol levels
Adherence to these medication regimens is crucial for optimal outcomes. We emphasize the importance of patient education and regular follow-up with healthcare providers to ensure compliance and adjust treatments as necessary.
Cardiac Rehabilitation Programs
Cardiac rehabilitation is a comprehensive program that includes exercise training, education on heart-healthy living, and counseling to reduce stress. These programs are designed to help patients recover from MI, improve their cardiovascular health, and reduce the risk of future heart problems.
| Components of Cardiac Rehabilitation | Benefits |
|---|---|
| Exercise Training | Improves cardiovascular fitness, reduces symptoms |
| Education on Heart-Healthy Living | Empowers patients to make lifestyle changes |
| Counseling and Stress Reduction | Enhances mental well-being, reduces stress |
Participation in cardiac rehabilitation programs has been shown to significantly improve outcomes for MI patients, including reduced mortality and improved quality of life.
Lifestyle Modifications for Recovery
Lifestyle changes are a critical component of long-term recovery after MI. We recommend that patients adopt a heart-healthy lifestyle, including:
- A balanced diet low in saturated fats, cholesterol, and sodium
- Regular physical activity tailored to the patient’s abilities and health status
- Smoking cessation and avoidance of secondhand smoke
- Stress management techniques such as meditation or yoga
Psychological Impact and Support
The psychological impact of MI should not be underestimated. Patients may experience anxiety, depression, or fear related to their condition. We emphasize the importance of providing emotional support through counseling, support groups, and family involvement. Addressing the psychological aspects of recovery is crucial for overall well-being and successful long-term management.
Conclusion: The Critical Importance of Understanding MI
Understanding what MI stands for in medical terms is crucial for both healthcare providers and patients. Myocardial Infarction, commonly known as a heart attack, requires prompt and effective management to prevent serious complications. We have explored the various aspects of MI, from its definition and types to diagnosis and treatment options.
Recognizing the warning signs of an MI and seeking immediate medical attention can significantly improve patient outcomes. As a healthcare provider committed to delivering world-class care, we emphasize the importance of education and awareness about MI. By understanding what MI means in medical terms, patients can take proactive steps to reduce their risk factors and receive timely treatment if needed.
Our mission is to provide comprehensive healthcare services that cater to the needs of international patients. We strive to deliver care that is not only medically excellent but also compassionate and supportive. By understanding MI and its implications, we can work together to improve patient care and outcomes.
FAQ
What does MI stand for in medical terms?
MI stands for myocardial infarction, commonly known as a heart attack, where the heart muscle is damaged due to a lack of blood supply.
What is the difference between STEMI and NSTEMI?
STEMI (ST-Elevation Myocardial Infarction) and NSTEMI (Non-ST-Elevation Myocardial Infarction) are two types of myocardial infarctions. STEMI is characterized by a complete blockage of a coronary artery, indicated by ST-segment elevation on an electrocardiogram (ECG), while NSTEMI involves a partial blockage, without ST-segment elevation.
What are the risk factors for myocardial infarction?
Risk factors for MI include modifiable factors such as high blood pressure, high cholesterol, smoking, and diabetes, as well as non-modifiable factors like age, family history, and genetic predisposition.
How is myocardial infarction diagnosed?
Diagnosis of MI involves a combination of clinical presentation, electrocardiogram (ECG) changes, cardiac biomarkers like troponin, and imaging studies to confirm the extent of cardiac damage.
What are the symptoms of a myocardial infarction?
Symptoms of MI can include chest pain or discomfort, shortness of breath, nausea, fatigue, and pain or discomfort in one or both arms, the back, neck, jaw, or stomach. Symptoms can vary by gender and age.
What is the immediate treatment for myocardial infarction?
Immediate treatment for MI involves emergency interventions like calling emergency services, reperfusion strategies such as thrombolysis or percutaneous coronary intervention (PCI), and medications like aspirin, beta-blockers, and anticoagulants.
What lifestyle changes are recommended after a myocardial infarction?
After an MI, recommended lifestyle changes include adopting a healthy diet, increasing physical activity, quitting smoking, managing stress, and adhering to prescribed medication regimens.
What is cardiac rehabilitation, and why is it important?
Cardiac rehabilitation is a comprehensive program that includes exercise training, education on heart-healthy living, and counseling to reduce stress and help patients recover from MI, improving their overall cardiovascular health.
Can myocardial infarction be prevented?
Yes, MI can be prevented or its risk reduced through primary prevention strategies like managing modifiable risk factors and secondary prevention measures such as medication adherence and lifestyle modifications in individuals with a history of cardiovascular disease.