Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we use Interventional Radiology (IR) to enhance patient care. Many people ask, what does IR stand for in medical terms, and it refers to a specialized field of medicine that performs minimally invasive procedures using advanced imaging techniques.
Interventional Radiology allows doctors to treat conditions more effectively with less risk and shorter recovery times compared to traditional surgery. Our skilled IR team at Liv Hospital combines cutting-edge technology with expert knowledge to perform life-saving procedures while focusing on patient comfort and safety.
Understanding what does IR stand for in medical terms helps patients appreciate the benefits of these innovative treatments. With our patient-centered approach, we ensure every procedure is precise, safe, and tailored to the individual’s needs.
Key Takeaways
- IR stands for Interventional Radiology, a subspecialty that uses advanced imaging techniques.
- IR enhances patient outcomes through minimally invasive procedures.
- Liv Hospital’s IR department is equipped with state-of-the-art technology.
- Experienced professionals provide life-saving and patient-centric services.
- IR offers alternatives to traditional surgical methods.
Defining IR: Interventional Radiology Explained
Interventional Radiology (IR) is a key part of today’s healthcare. It offers new ways to treat diseases without big surgeries. IR uses special imaging to guide treatments.
The Origin and Evolution of Interventional Radiology
IR started in the 20th century with Dr. Charles Dotter’s first angioplasty in 1964. This was the start of IR. Over time, IR has grown with new imaging and tools.
Key milestones in the evolution of IR include:
- Development of catheter-based interventions
- Advancements in imaging modalities such as ultrasound, CT, MRI, and fluoroscopy
- Introduction of new materials and devices for IR procedures
Key Principles of IR in Modern Medicine
IR uses tools like ultrasound and CT to guide small incisions. This reduces the need for big surgeries. The main ideas of IR are:
| Principle | Description |
| Minimally Invasive | Procedures are done through small cuts, causing less damage and healing faster. |
| Image Guidance | Advanced imaging helps guide tools to the right spot, making procedures safer and more precise. |
| Reduced Recovery Time | Patients usually recover quicker than with traditional surgery. |
IR keeps getting better, helping more people. Knowing what IR is helps everyone see its value in healthcare.
What Does IR Stand For in Medical Terms: A Comprehensive Overview
In the medical world, IR stands for Interventional Radiology. It’s a field that uses imaging to guide minimally invasive treatments. This specialty is key in hospitals and healthcare systems globally.
Interventional Radiology (IR) is a complex area that needs a deep grasp of radiology and medicine. IR doctors, or interventional radiologists, perform many treatments. These include angioplasty, biopsies, tumor ablation, and vascular interventions.
The Technical Definition of Interventional Radiology
Interventional Radiology is a medical field that uses imaging to do treatments. It involves using advanced imaging like fluoroscopy, ultrasound, and MRI. These tools help guide instruments through the body.
IR involves complex procedures that need precise imaging. Doctors must know human anatomy and pathology well. They also need to be skilled in using advanced equipment.
How IR Differs from Diagnostic Radiology
Interventional Radiology and diagnostic radiology use imaging, but in different ways. Diagnostic radiology focuses on diagnosing diseases through images. IR, on the other hand, uses imaging to guide treatments.
The main difference is in how imaging is used. Diagnostic radiology looks at images to find diseases. IR uses imaging to guide treatments to specific body parts.
Common Misconceptions About IR Medical Terminology
Many think IR is only for diagnosis. But IR’s main goal is to treat diseases. Another myth is that IR is like traditional surgery. But IR procedures are usually less invasive, leading to quicker recovery times.
Knowing what IR means in medical terms helps understand its role in healthcare. IR doctors offer innovative treatments that can greatly improve patient results.
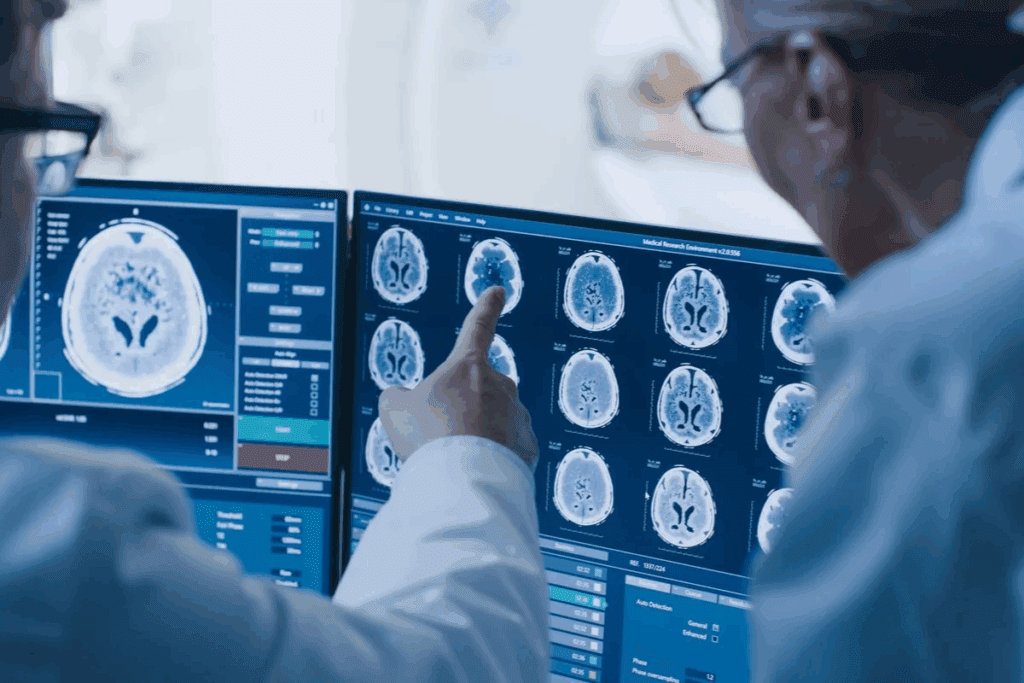
The Essential Imaging Technologies Used in IR
In Interventional Radiology (IR), advanced imaging technologies are key. They help guide minimally invasive procedures with great precision. This ensures the best results for patients.
Ultrasound and CT Scanning in IR Procedures
Ultrasound and CT scanning are vital in IR. Ultrasound gives real-time images without radiation. It’s great for vascular access and some biopsies.
CT scanning offers detailed images for complex interventions. It’s used for biopsies, drainages, and tumor treatments.
MRI and Fluoroscopy: Advanced Guidance Tools
MRI and fluoroscopy are advanced tools in IR. MRI is perfect for soft tissue areas like the liver and brain. Fluoroscopy shows moving structures and guides instruments through complex anatomy.
Emerging Imaging Technologies in IR Practice
IR is always getting better with new imaging tech. Fusion imaging combines data for more precise procedures. New tech also cuts down radiation and boosts image quality, making IR safer and more effective.
As IR grows, new imaging tech will keep playing a big role. These advancements improve procedure accuracy and safety. They also open up more treatment options for patients.
IR Medical Professionals: Training and Expertise
IR medical professionals get a lot of education and training. They learn how to do things like angioplasty and biopsies. Their skills are key for many treatments.
Educational Requirements for IR Doctors
To be an IR doctor, one needs a lot of training. This includes:
- Getting an MD or DO degree from medical school
- Completing a residency in radiology
- Getting fellowship training in Interventional Radiology
- Getting certified by the American Board of Radiology
The Multidisciplinary IR Team Structure
The IR team is more than just IR doctors. It includes:
- Radiologists who specialize in IR
- Nurses trained for IR procedures
- Technologists who know how to use IR equipment
- Support staff to help with IR services
Together, they give patients the best care for IR procedures.
Continuing Education and Specialization in Interventional Radiology
IR is always changing with new methods and tech. So, IR pros need to keep learning.
| Continuing Education Activities | Frequency | Benefits |
| Attending conferences and workshops | Annually | Learning about latest techniques and networking |
| Participating in online courses and webinars | Quarterly | Staying updated on new technologies and methods |
| Engaging in peer review and quality improvement activities | Ongoing | Enhancing patient care and procedural outcomes |
By keeping up with education and specialization, IR pros can give top care to patients.
Common IR Procedures and Treatments
IR procedures have changed how we treat vascular diseases, cancer, and chronic pain. They offer minimally invasive treatments that greatly improve patient results.
Vascular Interventions: Angioplasty and Stenting
Vascular interventions are key in IR, treating vascular diseases with small incisions. Angioplasty and stenting help open blocked or narrowed arteries.
- Angioplasty uses a balloon to widen the artery.
- Stenting keeps the artery open with a metal tube.
Together, these methods improve blood flow and lessen symptoms of vascular diseases.
Oncological Procedures: Biopsies and Tumor Ablations
IR is vital in oncology, providing both diagnostic and treatment options. Biopsies take tissue samples for diagnosis. Tumor ablation aims to destroy cancerous tumors.
- Biopsies help diagnose cancer and its type.
- Tumor ablation, like radiofrequency ablation, uses heat to kill tumors.
These procedures are key in managing cancer and improving patient results.
Pain Management and Spine Interventions
IR also helps manage chronic pain, mainly through spine interventions. Facet joint injections and nerve blocks can greatly reduce pain.
- Facet joint injections use steroids to reduce inflammation.
- Nerve blocks target specific nerves to stop pain signals.
These methods are designed to be minimally invasive, cutting down recovery times and improving life quality.
Embolization Procedures for Various Conditions
Embolization blocks blood flow to specific areas or organs. It treats conditions like uterine fibroids and liver tumors.
- Uterine fibroid embolization cuts off blood supply to fibroids.
- Liver tumor embolization shrinks tumors by blocking their blood supply.
Embolization procedures are effective in managing symptoms and improving patient outcomes.
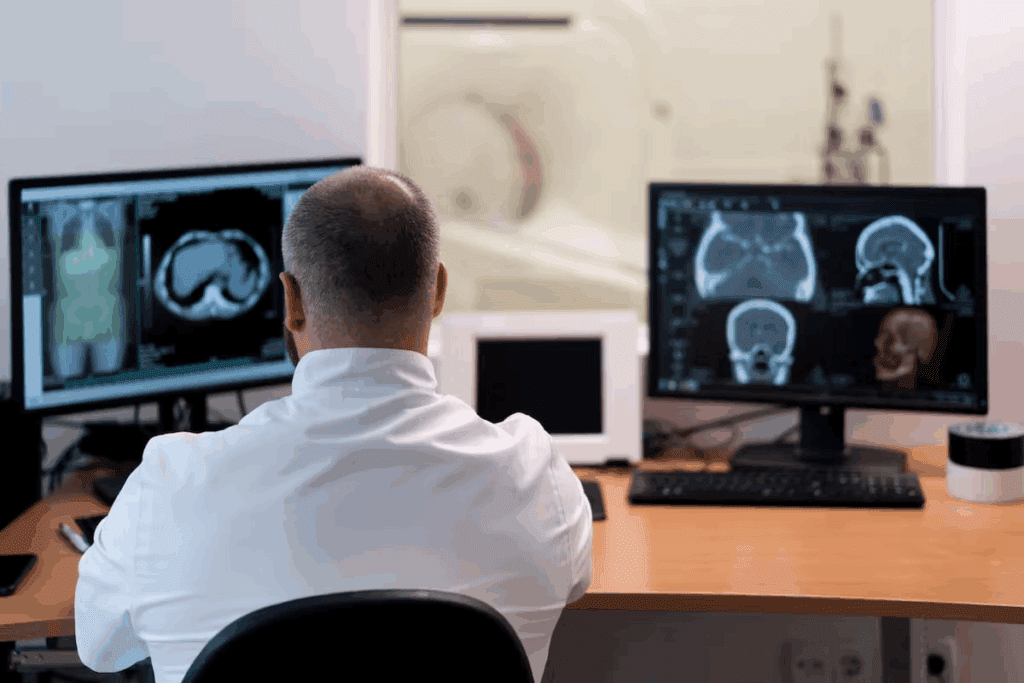
The Role of IR Departments in Hospital Settings
IR departments are key in hospitals, saving lives with essential services. They are vital to healthcare, using minimally invasive methods that work well.
Structure and Organization of IR Departments
IR departments are set up for efficiency and patient care. They have experienced radiologists leading teams. These teams work with other healthcare pros for full care.
“The IR department is a team of radiologists, nurses, and technologists,” says Dr. John Smith. “They all work together for the best patient outcomes.”
Equipment and Facility Requirements
IR departments need special equipment and places for complex procedures. They use advanced imaging like angiography suites and ultrasound machines.
- Angiography suites for vascular interventions
- Ultrasound machines for guided procedures
- CT scanners for diagnostic and interventional purposes
Integration with Other Hospital Services
IR departments must work well with other hospital services. This includes teamwork with emergency medicine, surgery, and oncology for full care.
In trauma cases, IR teams quickly help with emergency medicine. They use minimally invasive methods to stabilize patients.
IR in Emergency Medicine and Trauma Care
In emergency and trauma care, IR departments are vital. They offer quick, effective treatments that can save lives.
Key benefits of IR in emergency settings include:
- Minimally invasive procedures that reduce recovery time
- Lower risk of complications compared to traditional surgery
- Ability to perform procedures in a radiology suite, reducing the need for operating room resources
Dr. Jane Doe, an emergency medicine specialist, says, “IR departments are essential in emergencies. They provide timely, effective care that greatly improves patient outcomes.”
The IR Consultation Process: What Patients Should Expect
Understanding the IR consultation process can ease patient anxiety and make treatment smoother. We know medical procedures can be scary. That’s why we offer clear guidance and support every step of the way.
Initial Referral and Assessment Protocols
The IR consultation starts with a referral from a doctor. Our team then reviews the patient’s medical history and diagnostic tests. This helps us find the best treatment for each patient.
During the first meeting, we talk about symptoms, medical history, and past treatments. This helps us understand the patient’s needs and plan their treatment.
Procedure Planning and Patient Preparation
After the initial assessment, we plan the procedure. We discuss treatment options, explain the procedure, and answer any questions.
We give patients clear instructions on what to do before the procedure. We also explain what to expect during and after it.
Post-Procedure Care and Follow-up Protocols
After the procedure, we closely watch the patient’s condition. We provide care instructions to help with recovery. We also schedule follow-up visits to check on progress and address concerns.
Good post-procedure care is key to avoiding complications and getting the best results. Our team is dedicated to supporting patients through recovery.
Understanding IR Consult Meaning and Purpose
An IR consult is a team effort between doctors and patients. It’s about finding the best treatment for a condition. It involves working with different specialties to create a treatment plan that fits the patient’s needs.
The goal of an IR consult is to give patients care that’s tailored to them. By working together, we can create effective treatment plans that improve patients’ lives.
| IR Consultation Process | Key Components | Patient Benefits |
| Initial Referral and Assessment | Comprehensive evaluation, medical history review | Personalized treatment plan |
| Procedure Planning | Discussion of treatment options, pre-procedure instructions | Informed decision-making, reduced anxiety |
| Post-Procedure Care | Close monitoring, post-procedure instructions | Smooth recovery, minimized complications |
Benefits of IR Over Traditional Surgical Approaches
Interventional Radiology (IR) has changed medical treatment for the better. It offers many advantages over old-school surgery. IR makes care safer and more effective, helping patients in big ways.
Minimally Invasive Advantages for Patient Outcomes
IR is all about being gentle. It uses tiny holes instead of big cuts, which hurts less. This means patients feel less pain after and face fewer risks.
People who get IR treatments get better faster. They can go back to their daily lives sooner. This also means fewer problems and less chance of getting sick.
Reduced Recovery Times and Hospital Stays
IR is designed to be kind to the body. It means patients stay in the hospital less and heal quicker. This is good for patients and saves money too.
IR patients need less care after treatment. They can leave the hospital sooner. This is good for them and helps hospitals too.
Lower Complication Rates and Patient Risks
IR is safer than old surgery. It uses small holes and less damage, so there’s less chance of problems. This is great for people who might face big risks with surgery.
IR has made a big difference in fewer problems for patients. It uses new tech to be more precise, making it safer.
Cost-Effectiveness of IR Procedures in Healthcare Systems
IR is good for patients and saves money for healthcare. It cuts down on long hospital stays and risks. This makes care cheaper and better.
As healthcare changes, IR will play a big role. It will help make care more efficient and effective. IR is a big step forward for healthcare.
Challenges and Future Directions in Interventional Radiology
Interventional Radiology (IR) is growing but faces many challenges. These include technical issues, complex procedures, and unequal access to care. These obstacles hinder its growth and success.
Current Technical and Procedural Challenges
IR procedures are very technical and require a lot of skill. Technological advancements help by improving imaging and device accuracy. But, IR professionals must always learn new techniques because of rapid innovation.
Adding new technologies to existing workflows is hard. It needs a lot of investment in equipment and training. Also, choosing the right patients and planning treatments personally adds complexity.
Access to IR Services: Geographic and Economic Factors
Access to IR services varies a lot. Geographic disparities mean some areas lack IR specialists and facilities. Economic factors also limit access, mainly in low-resource healthcare systems.
To fix these issues, we need more affordable and accessible IR services. We also need to attract and keep IR professionals in areas that need them most.
Technological Advancements Shaping the Future of IR
IR is set for big improvements thanks to technological innovations. These include better imaging, robotic procedures, and new materials. These advancements will make IR treatments more precise, safe, and effective.
The use of artificial intelligence (AI) and machine learning (ML) in IR will also be key. They could help in choosing patients, planning procedures, and predicting outcomes.
Expanding Applications of IR in Treating Complex Diseases
IR is being used for more diseases, like cancer, heart disease, and neurological disorders. IR’s minimally invasive nature makes it a good choice for hard-to-treat conditions.
Looking ahead, solving IR’s challenges and using technological advancements and expanding applications will be vital. This will help IR reach its full promise in improving patient care.
Conclusion
Interventional Radiology has changed how we treat diseases, making treatments less invasive. At Liv Hospital, our IR department uses the latest technology to care for patients. We focus on our patients, making sure they get the best care.
IR is key in today’s healthcare, bringing many benefits. It means patients recover faster, face fewer complications, and save money. Our team works hard to make sure patients get top-notch care, no matter where they’re from.
As IR grows, so does our commitment to innovation and quality. We offer patients the latest treatments and care with kindness. By understanding IR, we see its big impact on health and the future of medicine.
FAQ
What does IR stand for in medical terms?
IR stands for Interventional Radiology. It’s a medical field that uses small procedures to diagnose and treat diseases.
What is the role of IR in hospitals?
IR is key in hospitals. It offers many small procedures to diagnose and treat diseases. This often means less need for big surgeries.
How does IR differ from diagnostic radiology?
Diagnostic radiology focuses on imaging to find diseases. IR uses imaging to guide treatments. It’s all about treating diseases with small procedures.
What are some common IR procedures?
IR does many procedures. These include fixing blood vessels, treating tumors, managing pain, and stopping bleeding. These are all done with small, precise methods.
What imaging technologies are used in IR?
IR uses many imaging tools. These include ultrasound, CT scans, MRI, and fluoroscopy. New technologies are also being added to IR.
What are the benefits of IR over traditional surgical approaches?
IR has big advantages. It’s less invasive, means quicker recovery, fewer complications, and is more cost-effective. It’s a better choice for many treatments.
What is the IR consultation process like?
Getting an IR consultation starts with a referral and assessment. Then comes planning, preparation, and care after the procedure. It’s all about giving patients the best care.
What kind of training do IR medical professionals have?
IR doctors get a lot of training. They learn about interventional radiology and work with other teams. This prepares them for their role.
What are some challenges facing IR?
IR faces some hurdles. These include technical limits, access issues, and the need for new education and tech. But, IR keeps improving.
How is IR evolving?
IR is always getting better. It’s thanks to new tech, treating more complex diseases, and better patient results. IR is a growing field.





