Last Updated on November 25, 2025 by Ugurkan Demir
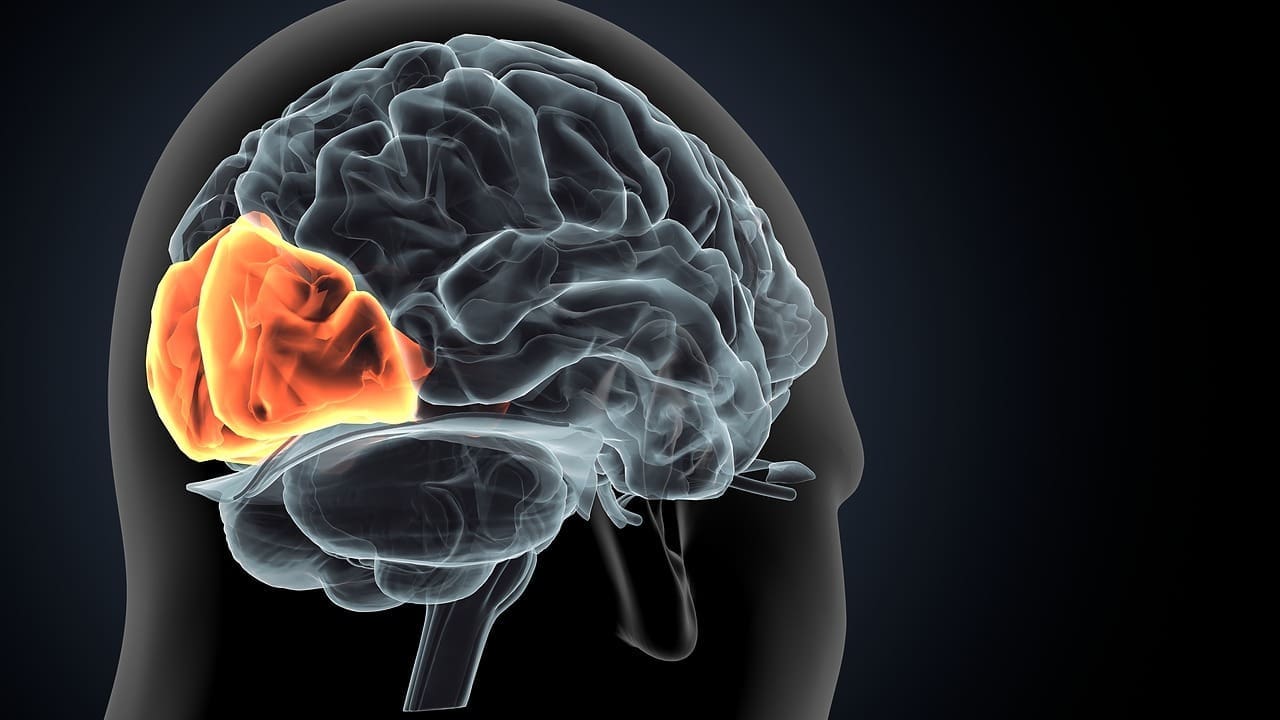
At Liv Hospital, we know how complex heart rhythm disorders like Paroxysmal Atrial Tachycardia (PAT) can be. PAT causes sudden, fast heart rates, usually starting in the atria. These rates can go up to 100-250 beats per minute. It’s a type of supraventricular tachycardia (SVT), but it starts in the atrial tissue, not like other types.
PAT can be triggered by stress, stimulants, or heart problems. Symptoms include heart palpitations, dizziness, and chest pain. Sometimes, people don’t even notice they have an episode. Doctors use ECGs to diagnose PAT, looking for a narrow QRS complex. Knowing about PAT is key to managing and treating it.
Key Takeaways
- PAT is a type of supraventricular tachycardia characterized by sudden rapid heart rate episodes.
- Triggers include stress, stimulants, and structural heart issues.
- Symptoms can vary, including palpitations, dizziness, and chest pain.
- Diagnosis is based on ECG findings.
- Effective management and treatment depend on understanding PAT.
What is Paroxysmal Atrial Tachycardia?
Understanding Paroxysmal Atrial Tachycardia (PAT) means looking into its definition, characteristics, and how it differs from other heart rhythm issues. We’ll see how PAT is defined and its main traits. Then, we’ll dive into the electrical pathways that make it unique.
Definition and Characteristics
Paroxysmal Atrial Tachycardia is a type of heart rhythm problem called supraventricular tachycardia (SVT). It starts in the atrial tissue. It’s marked by sudden, fast heart rates over 100 beats per minute, lasting from seconds to hours.
The term “paroxysmal” means these episodes start and stop suddenly. PAT is known for its episodic nature, with normal heart rhythm in between fast heart episodes. It’s different from other SVTs because it starts in the atrium, not the AV node.
The Electrical Pathway in PAT
The electrical pathway in PAT is due to abnormal activity in the atrial tissue. This can cause atrial tachycardia. Unlike other SVTs, PAT doesn’t involve the AV node.
To understand PAT’s electrical pathway, let’s compare it to normal heart rhythm:
| Characteristics | Normal Heart Rhythm | Paroxysmal Atrial Tachycardia |
| Origin of Electrical Activity | SA Node | Atrial Tissue |
| Heart Rate | 60-100 bpm | Typically >100 bpm |
| Episode Duration | Continuous | Episodic, variable duration |
| Involvement of AV Node | Normal conduction | Typically not involved |
This comparison shows the main differences between normal heart rhythm and PAT. It highlights PAT’s unique electrical pathway and episodic nature.
Paroxysmal Atrial Tachycardia vs. Other Arrhythmias
It’s important to know the differences between Paroxysmal Atrial Tachycardia (PAT) and other arrhythmias. PAT is a type of Supraventricular Tachycardia (SVT). But it has its own unique features that set it apart from other arrhythmias.
We will look at how PAT differs from other SVTs and ventricular tachycardias. This will help doctors and patients understand PAT’s specific traits. It will also show how it is diagnosed and treated differently.
PAT vs. Other Forms of Supraventricular Tachycardia
Supraventricular Tachycardia (SVT) includes various conditions with fast heart rates above the ventricles. PAT is a specific SVT, known for its intermittent nature and atrial origin.
- Origin: PAT starts in the atria, unlike other SVTs that may start in different places, like the AV node.
- Duration: PAT episodes are short and sudden, unlike other SVTs that can last longer.
- ECG Characteristics: PAT has a unique P-wave on an electrocardiogram (ECG). This helps doctors tell it apart from other SVTs.
Medical Expert, a cardiologist, says, “Knowing the difference between PAT and other SVTs is important. It affects how we treat and manage them.”
“Accurate diagnosis of PAT requires a thorough understanding of its unique characteristics and how they differ from other supraventricular tachycardias.”
Differences Between PAT and Ventricular Tachycardias
Ventricular tachycardias start in the ventricles and are more dangerous than SVTs like PAT. The main differences are:
- Origin: Ventricular tachycardias start in the ventricles, while PAT starts in the atria.
- Risk: Ventricular tachycardias carry a higher risk of cardiac arrest and sudden death than PAT.
- Treatment Approach: Ventricular tachycardias often need urgent and aggressive treatment, like immediate cardioversion or defibrillation. PAT may start with vagal maneuvers or medications.
In summary, PAT has its own set of characteristics that require a specific approach to diagnosis and treatment. Understanding these differences is key for healthcare providers to give the best care to PAT patients.
Primary Causes of Paroxysmal Atrial Tachycardia
To manage PAT well, knowing its causes is key. These can be structural heart abnormalities or non-cardiac triggers. Understanding these is vital for diagnosing and treating PAT.
Structural Heart Abnormalities
Structural heart issues are a big part of PAT. These can include:
- Atrial septal defects
- Mitral valve prolapse
- Wolff-Parkinson-White syndrome
- Other congenital heart defects
These problems can mess with the heart’s electrical paths, causing PAT. Early diagnosis and treatment of these conditions can help manage PAT symptoms.
Non-Cardiac Triggers
Non-cardiac factors can also start PAT episodes. These include:
- Stress and anxiety
- Drinking caffeine and nicotine
- Certain medications
- Hormonal changes
Handling these triggers can cut down on PAT episodes. Lifestyle changes and stress management are often suggested to patients.
By tackling both heart and non-heart causes of PAT, doctors can create treatment plans that fit each patient’s needs.
Identifying Common Symptoms of PAT Heart Arrhythmia
It’s key for both patients and doctors to know the signs of PAT heart arrhythmia. This condition shows itself in different ways, which helps in catching it early and treating it.
Physical Manifestations
The signs of PAT can be quite clear. People often feel their heart racing or pounding, known as palpitations. They might also feel dizzy, lightheaded, or have trouble breathing.
In some cases, chest pain or discomfort can occur. This is serious and needs quick medical help.
These symptoms happen because the heart rate suddenly goes up. This can make it hard for the heart to pump blood well. As a result, the body’s tissues and organs might not get enough oxygen and nutrients.
Asymptomatic Episodes
Some people with PAT might not feel any symptoms at all, even though the arrhythmia is happening. This makes finding the problem tricky. It might only be spotted during a check-up for something else or with heart monitoring devices.
These silent episodes show why regular health checks and heart monitoring devices are important. They help catch PAT or other heart rhythm problems early.
| Symptom | Description | Frequency |
| Palpitations | Feeling like the heart is racing or pounding | Common |
| Dizziness/Lightheadedness | Feeling faint or unsteady | Common |
| Shortness of Breath | Difficulty breathing or feeling winded | Less Common |
| Chest Pain/Discomfort | Pain or discomfort in the chest area | Less Common |
Knowing about these symptoms and the chance of silent episodes helps a lot in managing PAT. Being aware of these signs means people can get help fast. This can stop bigger problems from happening.
Diagnostic Approaches for Paroxysmal Atrial Tachycardia
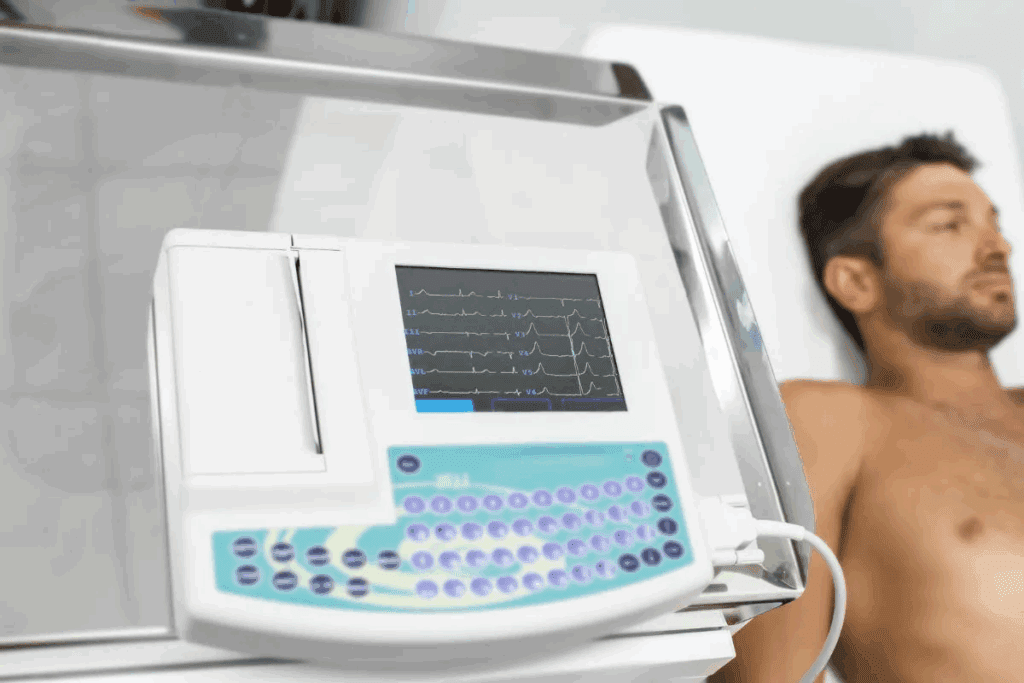
To find out if someone has PAT, doctors use several methods. These include the electrocardiogram (ECG) and other advanced tests. Getting the right diagnosis is key to treating PAT well.
Electrocardiogram (ECG) Findings
The ECG is a main tool for diagnosing PAT. It shows the heart’s electrical activity. ECG findings in PAT show a fast heart rate between 150-250 beats per minute. The P wave might be hard to see, and its shape can change based on where the abnormal rhythm starts.
When PAT happens, the ECG shows a sudden start and stop of the fast heart rate. Some key ECG signs include:
- A fast, regular heart rate
- Narrow QRS complexes unless there’s an unusual electrical path
- P waves that might be hidden in the T wave or seen with an odd axis
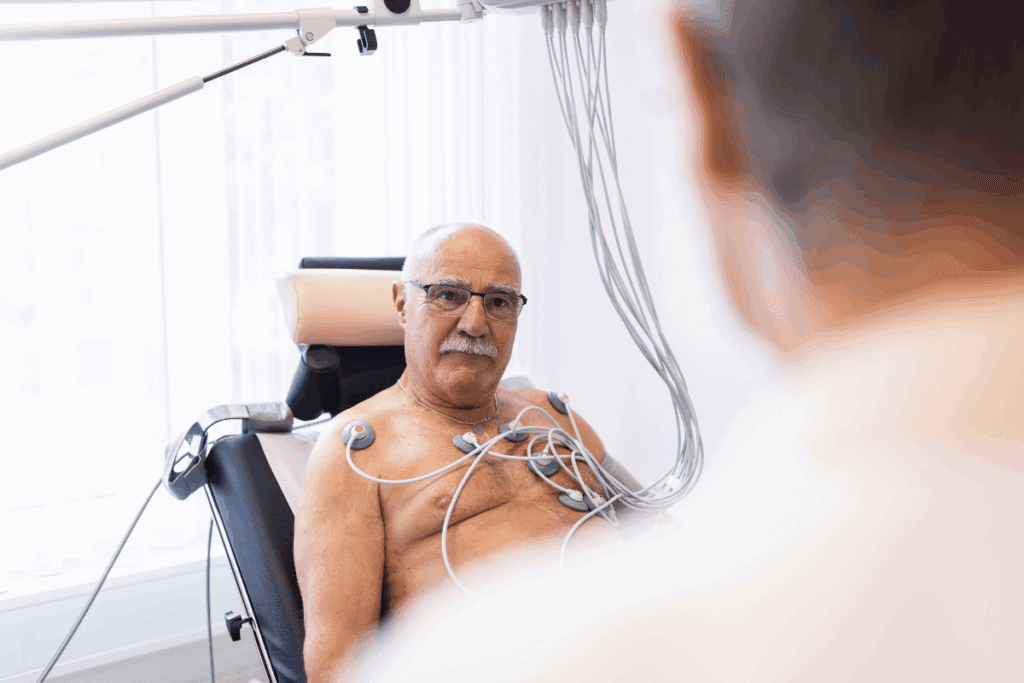
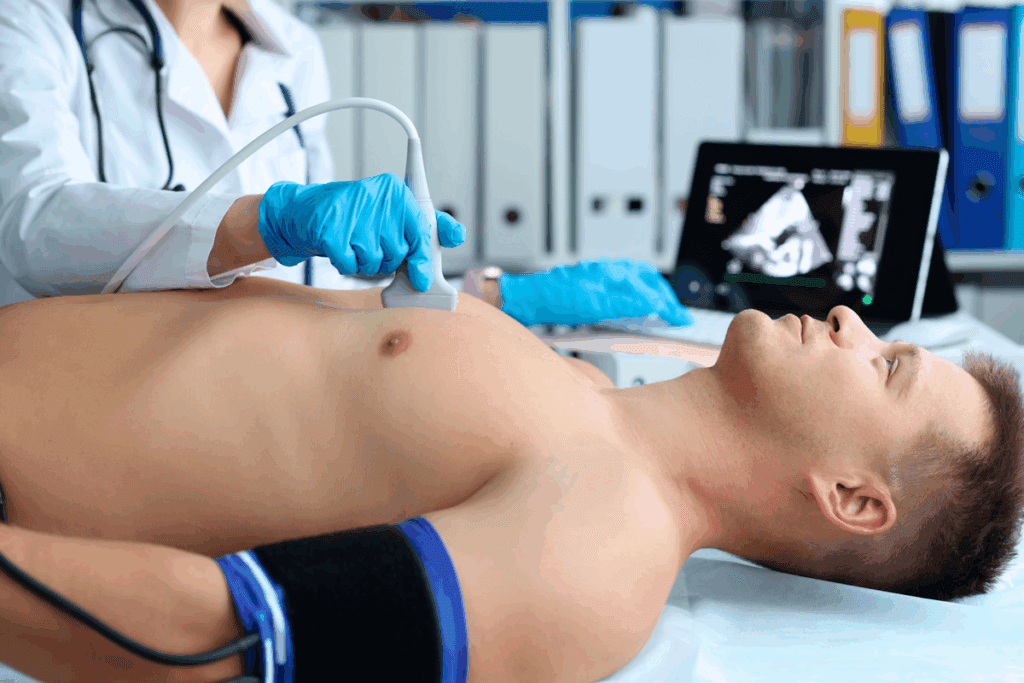
Advanced Diagnostic Methods
Even with ECG, doctors might use more tests to check PAT and what causes it. These include:
- Holter monitoring or event monitoring to catch PAT episodes over time
- Electrophysiological studies (EPS) to look at the heart’s electrical paths and find the tachycardia source
- Echocardiography to check the heart’s shape and how well it works
These extra tests help doctors create a treatment plan that fits each person’s needs. This way, they can manage PAT more effectively.
Risk Factors That Increase Susceptibility to PAT
Paroxysmal Atrial Tachycardia (PAT) can happen to anyone. But some people are more likely to get it. Knowing what increases the risk can help prevent or manage PAT.
Demographic Factors
Some things can make you more likely to get PAT. These include:
- Age: PAT can happen at any age, but it’s more common after 40.
- Family History: If your family has PAT or other heart issues, you might get it too.
- Gender: Some studies say women might get PAT more often than men, but it’s not clear.
These factors can tell you if you’re at higher risk for PAT.
| Demographic Factor | Influence on PAT Risk |
| Age > 40 | Increased risk |
| Family History of PAT | Increased risk |
| Gender (Female) | Potential increased risk |
Medical Conditions
Some health issues can also raise your risk for PAT. These include:
- Hypertension: High blood pressure can strain the heart and increase the risk of PAT.
- Heart Disease: Conditions like coronary artery disease and heart valve disorders can contribute to PAT.
- Thyroid Disorders: Both hyperthyroidism and hypothyroidism can affect heart rhythm and increase the risk of PAT.
- Obstructive Sleep Apnea: This condition can lead to increased stress on the heart and potentially contribute to PAT.
By understanding and tackling both demographic and medical risk factors, you can lower your chance of getting PAT. And if you do get it, managing it better can help.
Immediate Management Techniques for PAT Episodes
Managing PAT episodes right away is key to feeling better and avoiding serious issues. Stay calm and use proven methods when you have a PAT episode.
Vagal Maneuvers
Vagal maneuvers help slow your heart rate and might turn PAT into a normal rhythm. They are often the first thing doctors suggest for PAT.
- Valsalva Maneuver: Try to breathe out hard with your mouth closed and nostrils pinched. This can help your vagus nerve.
- Carotid Massage: Massaging the carotid sinus gently can also help your vagus nerve. But do this carefully and only if a doctor tells you to.
- Diving Reflex: Putting an ice pack on your face or dipping your face in cold water can also trigger this reflex.
Emergency Response Guidelines
Even though vagal maneuvers work well, knowing when to get emergency help is important. If your PAT episode is bad, lasts a long time, or comes with chest pain, shortness of breath, or dizziness, call for help right away.
Signs you should get emergency care include:
- Severe symptoms that don’t get better with vagal maneuvers
- History of heart disease or other health issues
- Signs of heart problems, like low blood pressure or losing consciousness
In emergencies, doctors might give you medicine to control your heart rate or fix the arrhythmia.
Medication Options for Treating Paroxysmal Atrial Tachycardia
Understanding the treatment options for Paroxysmal Atrial Tachycardia (PAT) is key. Medications help control symptoms and prevent future episodes. They improve life quality for those with PAT.
Acute Treatment Medications
For sudden PAT episodes, several medications can help. Adenosine is often the first choice because it works fast and well.
Beta-blockers (like metoprolol) and calcium channel blockers (like verapamil) also help. They slow the heart and fix the rhythm. These are given through an IV in a hospital to ensure quick care.
Long-term Pharmacological Management
For managing PAT long-term, the aim is to stop episodes and lessen symptoms. Beta-blockers are often used because they control heart rate and reduce episodes.
Calcium channel blockers are another choice for those who can’t take beta-blockers. Sometimes, anti-arrhythmic medications like flecainide or propafenone are used for frequent episodes.
Healthcare providers must customize treatment plans. They consider how often and how severe PAT episodes are, along with the patient’s health and past treatments.
Interventional Procedures for Persistent PAT
For those with ongoing Paroxysmal Atrial Tachycardia, new treatments are available. When usual treatments fail, more serious options are explored.
Catheter Ablation
Catheter ablation is a key treatment for some PAT cases. It uses catheters to destroy the heart’s bad electrical paths. This stops the arrhythmia.
The benefits of catheter ablation for PAT include:
- High Success Rate: Many patients see a complete end to PAT episodes after the procedure.
- Minimally Invasive: Done through small cuts, it’s less invasive than open surgery.
- Quick Recovery: Most can get back to normal in just a few days.
Surgical Approaches
Surgery might be needed for PAT, if other treatments don’t work. Surgical methods tackle the arrhythmia’s root cause.
Surgical options include:
- Maze Surgery: Creates scar tissue in the heart’s upper chambers. This guides the heart’s electrical signals.
- Surgical Ablation: Like catheter ablation but done during open-heart surgery. It’s more precise.
These treatments mark a big step forward in managing PAT. They offer new hope to those who haven’t found relief elsewhere.
Lifestyle Modifications to Manage Paroxysmal Atrial Tachycardia
Changing our lifestyle can greatly help manage Paroxysmal Atrial Tachycardia. Making smart choices in our daily lives can lessen PAT episodes. This method works well with medical treatments and lets us take charge of our health.
Dietary Considerations
What we eat is key in managing PAT. Some foods can make episodes worse, while others can help prevent them. A diet full of fruits, veggies, whole grains, and lean proteins is best. Drinking lots of water is also important.
Here are some tips for a PAT-friendly diet:
- Try to cut down on caffeine and alcohol, as they can cause arrhythmias
- Eat less high-sodium foods to keep blood pressure in check
- Eat more foods rich in omega-3s, like fish and nuts
Stress Management Techniques
Stress can trigger PAT episodes. So, it’s vital to find ways to manage stress. Techniques like deep breathing, meditation, and yoga can help lower stress and boost well-being.
Here are more ways to handle stress:
- Regular exercise can help reduce stress and keep the heart healthy
- Getting enough sleep is important for rest and recovery
- Talking to friends, family, or support groups can help with emotional stress
By focusing on diet and stress management, people with PAT can live better lives. They can also cut down on how often episodes happen.
Potential Complications of Untreated PAT
Untreated PAT can harm your heart and daily life. It can cause serious problems that affect your heart and how you live every day.
Cardiac Consequences
Untreated Paroxysmal Atrial Tachycardia can lead to heart issues. These include:
- Heart Failure: Long-term tachycardia can weaken the heart, possibly causing heart failure.
- Tachycardia-induced Cardiomyopathy: Long-term rapid heart rates can damage the heart muscle.
- Stroke and Thromboembolism: The irregular heart rhythm can cause blood clots, raising the risk of stroke.
Impact on Daily Functioning
Untreated PAT also affects your daily life. Symptoms like palpitations, dizziness, and shortness of breath can:
- Limit Physical Activity: Making it hard to do daily tasks and exercise.
- Affect Mental Health: Causing anxiety and stress from unpredictable episodes.
- Impair Cognitive Function: Possibly affecting your focus and productivity.
Knowing these risks shows why managing PAT is key to keeping your heart and life quality good.
Conclusion: Living Well with Paroxysmal Atrial Tachycardia
We’ve looked into Paroxysmal Atrial Tachycardia (PAT), a heart rhythm issue. It causes sudden, fast heart rates. Knowing the causes, symptoms, and treatments is key to managing PAT well.
Living with PAT means making lifestyle changes, taking medicine, and sometimes getting procedures. A healthy lifestyle can help lessen how often and how bad the episodes are.
Studies show that with the right care, people with PAT can live full and active lives. It’s vital to work with doctors to create a care plan that fits you.
Handling PAT is a long-term effort. It means watching symptoms, changing treatments when needed, and making smart lifestyle choices. By being involved in your care, you can reduce PAT’s impact on your life.
Good management of PAT helps keep your life quality high. You can keep doing things you love and lower the risk of problems linked to PAT.
FAQ
What is Paroxysmal Atrial Tachycardia (PAT)?
Paroxysmal Atrial Tachycardia is a sudden, fast heart rate. It starts in the atria.
How does PAT differ from other forms of Supraventricular Tachycardia (SVT)?
PAT comes from the atria. Other SVTs can start from different places, like the AV node.
What are the primary causes of Paroxysmal Atrial Tachycardia?
PAT is often caused by heart problems, non-heart triggers, and other health issues. These can affect the heart’s electrical system.
What are the common symptoms of PAT?
Symptoms include heart palpitations, fast heart rate, dizziness, and shortness of breath. Some people may not feel anything during an episode.
How is PAT diagnosed?
Doctors use an electrocardiogram (ECG) and Holter monitoring to find the fast heart rate. These tests show the heart’s electrical activity.
What are the risk factors for developing PAT?
Risk factors include age, health conditions, and lifestyle choices. These can affect heart health.
How can PAT episodes be managed immediately?
Vagal maneuvers, like the Valsalva maneuver, can help. If symptoms don’t go away, seek medical help.
What medication options are available for treating PAT?
Adenosine is used for quick treatment. For ongoing management, beta blockers and anti-arrhythmics are options.
What interventional procedures are available for persistent PAT?
For ongoing PAT, catheter ablation or surgery can target the arrhythmia source. This aims to restore normal rhythm.
How can lifestyle modifications help manage PAT?
Changes like diet, stress management, and avoiding triggers can reduce PAT episodes. They help manage symptoms.
What are the possible complications of untreated PAT?
Untreated PAT can lead to heart failure and affect daily life. It can lower quality of life.
What is the difference between PAT and ventricular tachycardias?
PAT starts in the atria, while ventricular tachycardias start in the ventricles. They have different symptoms and treatments.
Can PAT be cured?
PAT can be managed and treated. A “cure” depends on the cause and treatment response. Ongoing monitoring is often needed.
References
- Liwanag, M., & Willoughby, C. (2023, June 26). Atrial tachycardia. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542235/
- Kotadia, I. D., et al. (2020). Supraventricular tachycardia: An overview of diagnosis and management. Progress in Cardiovascular Diseases, https://www.sciencedirect.com/science/article/pii/S1470211824036510