Patients with certain cancers and blood disorders might need a bone marrow transplant to live. But, this treatment is complex and hard. Luckily, stem cell therapy is now a promising option, giving hope to many.
They help replace the bone marrow with stem cells. This way, the body can make healthy blood cells again.
Stem cell transplants have opened up new ways to treat diseases like leukemia and lymphoma. This means patients have more treatment choices now.
Key Takeaways
- Stem cell therapy is a viable alternative to bone marrow transplants.
- Stem cell transplants are used to treat various cancers and blood disorders.
- This treatment involves restoring the patient’s bone marrow to produce healthy blood cells.
- Leukemia and lymphoma patients can benefit from stem cell transplants.
- Stem cell therapy offers new hope for patients with certain medical conditions.
Understanding Bone Marrow Transplants
Bone marrow transplants are complex procedures. They involve replacing damaged or diseased bone marrow with healthy stem cells. This is a medical treatment that aims to restore health.
What is a Bone Marrow Transplant?
A bone marrow transplant is a way to replace damaged bone marrow with healthy stem cells. It’s used for conditions like leukemia and lymphoma. Common Indications for Bone Marrow Transplants
Bone marrow transplants help treat cancers and blood disorders. They are often used for:
- Leukemia
- Lymphoma
- Multiple myeloma
- Aplastic anemia
Choosing to have a bone marrow transplant depends on several things. These include the disease type and stage, and the patient’s health.
Limitations and Challenges of Traditional Transplants
Traditional bone marrow transplants have challenges. These include:
- Graft-versus-host disease (GVHD), where the donor’s immune cells attack the recipient’s tissues.
- Finding a compatible donor can be hard, which is a big problem for diverse ethnic backgrounds.
- The conditioning before the transplant can cause serious side effects.
| Condition | Success Rate | Common Complications |
| Leukemia | 60-80% | GVHD, infections |
| Lymphoma | 50-70% | GVHD, organ toxicity |
| Multiple Myeloma | 40-60% | Infections, GVHD |
The Need for Alternatives
Bone marrow transplantation is a lifesaver but comes with big challenges. Finding a donor, dealing with transplant issues, and keeping a good quality of life are major hurdles. These problems push for new treatment options.
Donor Availability Issues
Finding a compatible donor is a big challenge in bone marrow transplants. The National Marrow Donor Program (NMDP) has a donor registry. But, finding a match is harder for people from different ethnic groups.
Patients from diverse ethnic backgrounds often face difficulties in identifying a suitable donor. This can delay or even prevent them from getting a transplant.
Transplant-Related Complications
Bone marrow transplants can lead to several complications. These include graft-versus-host disease (GVHD), infections, and organ damage. GVHD happens when the donor’s immune cells attack the recipient’s body.
Managing these complications is tough. It requires careful monitoring and often more treatments. These can affect the patient’s quality of life.
| Complication | Description | Management Strategies |
| Graft-versus-host disease (GVHD) | Immune reaction against the recipient’s body | Immunosuppressive medications, supportive care |
| Infections | Increased susceptibility due to immunosuppression | Prophylactic antibiotics, antifungals, and antivirals |
| Organ damage | Toxicity from conditioning regimens | Monitoring, supportive care, dose adjustments |
Quality of Life Considerations
The impact of bone marrow transplantation on a patient’s quality of life is huge. The procedure involves tough conditioning regimens and can lead to complications. Patients often feel tired, have cognitive changes, and emotional distress that can last long after the transplant.
Alternative therapies aim to lessen these effects. They want to improve patient outcomes and quality of life.
Stem Cell Therapy: The Leading Alternative
Stem cell therapy is a new hope for patients with blood-related disorders. It uses stem cells to repair or replace damaged tissues. This could change regenerative medicine forever.
Differences from Traditional Bone Marrow Transplants
Stem cell therapy is different from traditional bone marrow transplants. It doesn’t take stem cells directly from bone marrow. Instead, it uses stem cells from blood and umbilical cord blood.
Key differences include:
- The source of stem cells
- The method of stem cell collection
- The conditioning regimen required before transplantation
- The chance of reduced graft-versus-host disease (GVHD)
Types of Stem Cells Used in Treatments
Stem cell therapy uses different types of stem cells. Each type has its own uses and benefits. The most common types are:
- Hematopoietic Stem Cells (HSCs): Treats blood-related disorders and cancers.
- Mesenchymal Stem Cells (MSCs): Helps repair tissues by turning into different cell types.
- Embryonic Stem Cells: Can turn into any cell type, but is controversial.
The American Society of Clinical Oncology says, “Stem cell therapy uses stem cells to repair or replace damaged tissues. It’s a promising alternative to traditional bone marrow transplants.”
Conditions Treatable with Stem Cell Therapy
Stem cell therapy can treat many conditions. These include:
- Blood cancers like leukemia and lymphoma
- Bone marrow failure syndromes
- Certain genetic disorders
- Autoimmune diseases
As research grows, stem cell therapy’s uses are expanding. It offers hope to patients who can’t have traditional bone marrow transplants.
Peripheral Blood Stem Cell Transplantation
The Peripheral Blood Stem Cell Transplantation has changed how stem cells are used for transplants. It takes stem cells from the blood, making it a gentler option than bone marrow harvesting.
Collection Process and Advantages
The process starts with apheresis. This is when the patient’s or donor’s blood is drawn and the stem cells are separated. Then, the blood parts are returned to the body. This method is better because it doesn’t need surgery, making it safer and quicker to recover.
Key benefits of Peripheral Blood Stem Cell Transplantation include:
- Less invasive procedure compared to bone marrow harvesting
- Faster recovery time
- Reduced risk of surgical complications
Comparing Outcomes with Traditional Bone Marrow Transplants
Research has looked at how Peripheral Blood Stem Cell Transplantation compares to bone marrow transplants. Peripheral Blood Stem Cell Transplantation often gives more stem cells. This can mean faster recovery for patients.
The results of Peripheral Blood Stem Cell Transplantation are watched closely. This is to make sure patients get the best care.
Patient Experience and Recovery
Patients usually find Peripheral Blood Stem Cell Transplantation more comfortable than bone marrow transplants. This is because it doesn’t involve surgery. But, patients might get chemotherapy or radiation, which can cause side effects. Recovery is often faster, allowing patients to get back to their lives sooner.
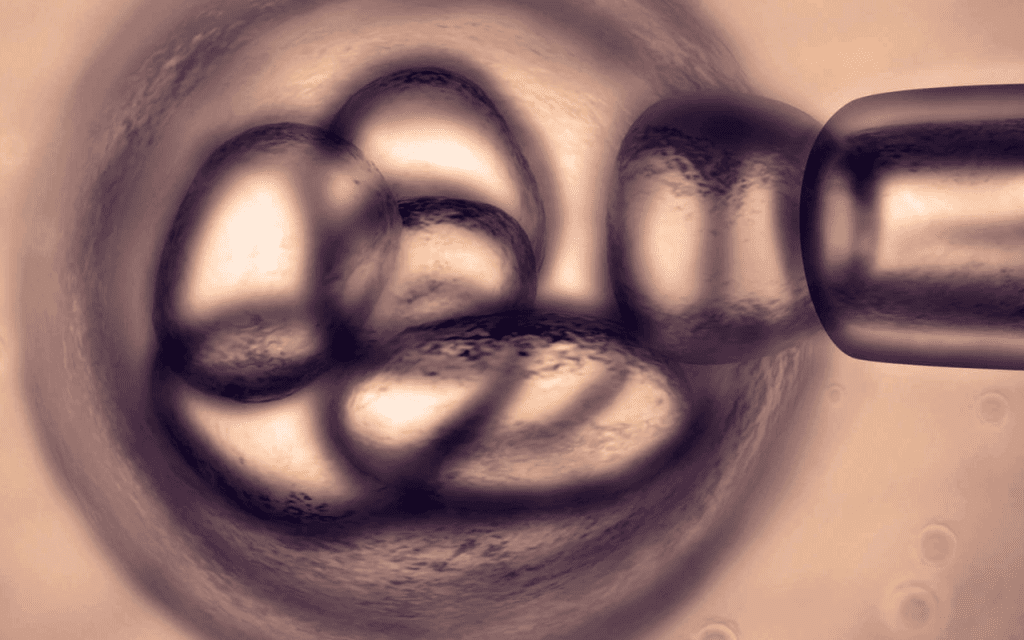
Cord Blood Transplantation
Umbilical cord blood was once seen as waste. Now, it’s a key part of stem cell therapy and transplantation. This change is because cord blood is full of stem cells that help treat blood disorders.
Umbilical Cord Blood as a Stem Cell Source
Cord blood comes from the umbilical cord after birth. It’s packed with hematopoietic stem cells. These cells can turn into any blood cell type, making cord blood very useful for transplants.
Getting cord blood is easy and doesn’t hurt. It’s different from other ways to get stem cells.
Benefits and Limitations of Cord Blood
Using cord blood has many advantages. It’s easy to get, has less risk of GVHD, and can be used from donors who aren’t a perfect match. But, there are downsides too.
For example, there’s not much stem cell material in one cord blood unit. This can cause slower healing and more infections.
| Benefits | Limitations |
| Ready availability | Limited stem cell quantity |
| Reduced risk of GVHD | Delayed engraftment |
| Use of partially matched donors | Increased risk of infections |
Expanding Applications in Treatment
Cord blood is being used more to treat diseases like leukemia and genetic disorders. Scientists are also exploring new uses, like in regenerative medicine.
Cord Blood Banking Considerations
Thinking about cord blood banking means looking at costs, how likely it is to be used, and ethical issues. Cord blood banking can be private for family use or public for anyone. It’s important to talk to doctors before making a decision.
Reduced-Intensity Conditioning Transplants
For those not fit for standard bone marrow transplants, reduced-intensity conditioning transplants offer a lifeline. This method is less harsh, making it better for older folks or those with health problems.
The “Mini Transplant” Approach
Known as “mini transplants,” these use less chemotherapy and radiation than usual. This makes the treatment safer, with fewer side effects and death risks.
This method counts on the new immune system to fight off disease. It’s a gentler way to switch to a donor’s immune system, which can help avoid some problems.
Candidates for Reduced-Intensity Conditioning
Older adults, those with health issues, or those who’ve had a lot of treatment before are good candidates. Doctors look at the patient’s health, disease, and past treatments to decide.
- Older patients or those with significant comorbidities
- Patients with relapsed or refractory diseases
- Individuals who have undergone previous intensive treatments
Success Rates and Considerations
Success with these transplants depends on many things, like the disease, patient health, and how well the donor’s cells match. While it can be a cure for some, it comes with risks like GVHD and disease coming back.
Research shows these transplants can work as well as the usual kind for some patients. They have the advantage of being less deadly. But, picking the right patients and watching them closely is key to success.
“Reduced-intensity conditioning regimens have expanded the eligibility for allogeneic hematopoietic cell transplantation to older and sicker patients, providing a potentially curative option for those who were previously considered ineligible.”
As research keeps improving, these transplants might help more people. They offer hope to those who couldn’t get traditional transplants before.
Autologous vs. Allogeneic Transplantation
Autologous and allogeneic transplants are two main ways to use stem cells. Each has its own benefits and things to think about. The choice depends on the patient’s health, age, and condition.
Using Your Own Cells: Autologous Transplants
Autologous transplants use a patient’s own stem cells. This method avoids graft-versus-host disease (GVHD). GVHD happens when donor cells attack the patient’s body. These transplants are often used for cancers like multiple myeloma and lymphoma.
Advantages of Autologous Transplants:
- Reduced risk of GVHD
- Faster engraftment
- Lower risk of transplant-related complications
Donor Cells: Allogeneic Transplants
Allogeneic transplants use stem cells from a donor. They are good for patients with genetic disorders or certain leukemias. The donor cells can replace the patient’s bad immune system with a healthy one.
Key Considerations for Allogeneic Transplants:
- Risk of GVHD
- Need for a compatible donor
- Potential for graft-versus-tumor effect
Choosing the Right Approach for Different Conditions
The choice between autologous and allogeneic transplants depends on the patient’s condition and medical history. For example, autologous transplants might be better for some cancers. Allogeneic transplants could be better for genetic disorders.
| Transplant Type | Cell Source | Advantages | Disadvantages |
| Autologous | Patient’s own cells | Reduced risk of GVHD, faster engraftment | Limited by availability of healthy cells |
| Allogeneic | Donor cells | Graft-versus-tumor effect, can treat genetic disorders | Risk of GVHD, need for compatible donor |
In conclusion, both autologous and allogeneic transplants have their roles in treating different conditions. Knowing the differences helps make better choices for stem cell therapy.
Haploidentical Transplantation
Haploidentical transplantation uses cells from a partially matched donor. This expands the donor pool for those needing a transplant. It’s very helpful for people without a fully matched donor.
Partially Matched Donor Transplants
Donors in haploidentical transplantation are usually family members. They share half of the recipient’s genetic material. This partial match is enough for a transplant, but it comes with some risks.
Advantages of partially matched donors include a quick transplant process. But, managing graft-versus-host disease (GVHD) is key. This requires careful planning and post-transplant care.
Expanding the Donor Pool
Haploidentical donors greatly increase the donor pool. Almost everyone has a haploidentical family member. This is great for patients from diverse backgrounds who often struggle to find a match.
- Immediate availability of donors
- Increased chances of finding a donor for patients from diverse ethnic backgrounds
- Potential for reduced time to transplant
Recent Advances in Haploidentical Approaches
Recent improvements in haploidentical transplantation aim to better outcomes. These include better conditioning regimens and ways to prevent GVHD. These changes have made survival rates similar to those with matched donors in some studies.
Key developments include using post-transplant cyclophosphamide to prevent GVHD. Also, optimizing conditioning regimens to improve engraftment and reduce side effects.
The ongoing development of haploidentical transplantation is making it a strong option for patients needing a transplant.
Microtransplantation: A Newer Approach
Medical technology has led to microtransplantation, a new way to use stem cells. This method uses small amounts of donor stem cells. It might be better than old transplant ways.
How Microtransplantation Works
Microtransplantation uses donor stem cells to help the immune system. It doesn’t need harsh treatments to prepare the body. This could make the transplant last longer and be more stable.
First, a good donor is found. Then, stem cells are taken from them. These cells are given to the patient to help them.
Potential Benefits Over Traditional Transplants
Microtransplantation might lower the risk of graft-versus-host disease (GVHD). GVHD is a big problem with old transplant methods.
It could also mean less chance of dying from treatment and better life quality. This is because it doesn’t need strong treatments.
Current Research and Applications
Researchers are working to make microtransplantation better. They’re looking at how many stem cells to use and the best treatments.
Early studies look good for treating blood cancers. More trials are checking if it works for other diseases too.
- Looking into microtransplantation for acute myeloid leukemia
- Seeing if it works for myelodysplastic syndromes
- Checking its use in lymphoma
As research grows, microtransplantation is becoming a key part of stem cell therapy. It offers hope for patients and doctors.
CAR-T Cell Therapy: A Revolutionary Alternative
CAR-T cell therapy is a new way to fight cancer. It’s different from traditional bone marrow transplants. This method takes a patient’s T cells, changes them to attack cancer, and puts them back in the body.
Engineering Immune Cells to Fight Cancer
The first step is to get T cells from the patient’s blood. These cells are then changed in a lab to find and kill cancer cells. After being changed, these cells are put back into the patient to fight cancer.
Key benefits of CAR-T cell therapy include its targeted approach, reducing harm to healthy cells, and its long-term cancer control. But, it can cause serious side effects like cytokine release syndrome, which needs careful management.
FDA-Approved CAR-T Therapies
Several CAR-T cell therapies have been approved by the FDA for blood cancers. Tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) have shown great results in trials. Researchers are also looking into using CAR-T for other cancers and making it safer.
Comparing CAR-T with Transplantation
CAR-T cell therapy is different from bone marrow transplants. Bone marrow transplants replace a patient’s immune system with a donor’s. CAR-T cell therapy changes the patient’s own immune cells. This can lead to fewer problems and a quicker recovery for some.
Patient Selection and Considerations
Choosing the right patients for CAR-T cell therapy is key. Doctors look at the cancer type, stage, previous treatments, and overall health. It’s also important to manage expectations about side effects and the need for close monitoring after treatment.
In conclusion, CAR-T cell therapy is a promising option for some patients. Its innovative method and possible benefits make it a significant advancement in cancer treatment.
Gene Therapy Approaches
The field of gene therapy is growing fast, bringing new hope to those with genetic defects. It aims to fix these problems at their source. Gene therapy makes changes to the genetic material of living cells to fight or prevent disease.
This area of research is promising. It could treat many diseases without the need for bone marrow transplants.
Correcting Genetic Defects Without Transplantation
Gene therapy tries to fix diseases by fixing the genetic problem. This method could eliminate the need for bone marrow transplants. It does this by replacing a faulty gene with a healthy one, repairing a damaged gene, or controlling a gene’s expression.
Current Gene Therapy Treatments
Several gene therapy treatments have been approved. For example, Luxturna treats a rare form of blindness. Zolgensma is used for spinal muscular atrophy. These show gene therapy’s power to tackle severe genetic conditions.
Future Directions in Gene Therapy
The future of gene therapy is bright. Scientists are working hard to make it even better. They’re looking into new ways to deliver genes, improving gene editing tools like CRISPR/Cas9. They’re also exploring treatments for complex diseases like cancer and heart problems.
| Therapy Type | Current Status | Potential Applications |
| Gene Replacement | Approved for certain conditions | Rare genetic disorders |
| Gene Editing | In clinical trials | Cancer, genetic diseases |
| Gene Regulation | Early research stages | Complex diseases, cancer |
Mesenchymal Stem Cell (MSC) Therapy
Mesenchymal Stem Cell (MSC) therapy is a new hope in regenerative medicine. MSCs can turn into different cell types. This makes them great for fixing damaged tissues.
Understanding MSCs and Their Potential
MSCs come from tissues like bone marrow and fat. They can help the immune system, reduce swelling, and help grow new tissue.
Key characteristics of MSCs include:
- Ability to differentiate into multiple cell types
- Immunomodulatory properties
- Capacity to support tissue repair
Current Applications in Various Diseases
MSC therapy is being tested for many diseases. These include:
- Orthopedic injuries and degenerative diseases
- Autoimmune disorders, such as multiple sclerosis and lupus
- Graft-versus-host disease (GVHD)
- Cardiovascular diseases
Studies show MSCs can help these conditions. Many patients see better health and life quality.
Combining MSCs with Other Treatments
MSC therapy works better with other treatments. For instance, mixing MSCs with gene therapy or drugs can improve results.
Current research is focused on optimizing these combination therapies to make them safer and more effective. As research grows, we’ll see new ways to use MSCs in medicine.
Accessing Alternative Transplant Options
Looking into alternative transplant options requires a careful approach. This includes looking at FDA-approved treatments and clinical trials. Patients need to consider their medical needs and personal situation.
FDA-Approved Treatments vs. Clinical Trials
Patients often have to choose between FDA-approved treatments and clinical trials. FDA-approved treatments are safe and effective, having gone through lots of testing. Clinical trials offer new therapies that might not be available yet.
It’s important to weigh the benefits and risks of each choice. FDA-approved treatments are proven, but clinical trials might offer new treatments with unknown effects.
| Treatment Type | Benefits | Risks/Considerations |
| FDA-Approved Treatments | Proven safety and efficacy, established protocols | May not be suitable for all patients or conditions |
| Clinical Trials | Access to innovative therapies, potentially better outcomes | Unknown effects and side effects, strict rules |
Insurance Coverage and Financial Considerations
Understanding insurance coverage and financial considerations is key. Patients need to know what their insurance covers, including FDA-approved treatments and clinical trials.
- Check insurance policies for coverage of alternative transplant options.
- Look for financial help programs to cover treatment costs.
- Talk to healthcare providers about possible costs to plan financially.
Finding Specialized Treatment Centers
Finding specialized treatment centers is important for alternative transplant options. These centers have teams skilled in new treatments.
To find a good center, patients can:
- Ask their primary doctor for recommendations.
- Search online for centers with the right expertise.
- Get advice from patient advocacy groups on trusted centers.
Questions to Ask Your Healthcare Provider
When talking to healthcare providers about transplant options, ask the right questions. Ask about:
- The benefits and risks of treatments or trials.
- Expected results compared to traditional transplants.
- Support services for treatment challenges.
Conclusion: The Future of Transplant Alternatives
The future of transplant alternatives is bright, thanks to ongoing research. This includes work in stem cell therapy, regenerative medicine, and immunotherapy.Stem cell therapy is becoming a top choice for patients who can’t get traditional bone marrow transplants. Regenerative therapy and immunotherapy also hold promise in solving transplant-related problems.
As research keeps moving forward, we can expect better results and more treatment options for patients. It’s important to bring these new therapies into everyday medical practice. This will help shape the future of transplant alternatives.
FAQ
What is the difference between a bone marrow transplant and stem cell therapy?
A bone marrow transplant replaces a patient’s bone marrow with healthy stem cells. Stem cell therapy uses stem cells to fix or replace damaged cells. These cells can come from bone marrow, blood, or cord blood.
Are there alternatives to traditional bone marrow transplants?
Yes, there are many alternatives. These include using stem cells from blood or cord blood. Other options include reduced-intensity transplants and gene therapy.
What is peripheral blood stem cell transplantation?
Peripheral blood stem cell transplantation collects stem cells from blood. These cells replace the patient’s bone marrow. It’s a common alternative to traditional transplants.
What are the benefits of cord blood transplantation?
Cord blood transplantation has several benefits. It has a lower risk of graft-versus-host disease. It also uses partially matched units and has a readily available source of stem cells. But, it has a lower stem cell count and slower engraftment.
What is reduced-intensity conditioning, and who is a candidate for it?
Reduced-intensity conditioning uses lower doses of chemotherapy and radiation. It’s for older patients or those with health issues. They can’t handle traditional transplants.
What is the difference between autologous and allogeneic transplantation?
Autologous uses the patient’s own stem cells. Allogeneic uses donor cells. The choice depends on the disease, health, and donor availability.
What is CAR-T cell therapy, and how does it compare to traditional transplantation?
CAR-T cell therapy makes T cells attack cancer cells. It’s not a traditional transplant but treats blood cancers. It’s for patients who haven’t responded to other treatments.
What is gene therapy, and how does it work?
Gene therapy fixes genetic defects by adding healthy genes to cells. It uses viral vectors or gene editing. It treats genetic diseases without transplanting.
How do I access alternative transplant options, and what are the considerations?
Talk to your healthcare provider about alternative options. Consider FDA-approved treatments, clinical trials, insurance, and finances. Look for specialized treatment centers.
What is MSC, and what are its possible uses?
MSC therapy uses mesenchymal stem cells to repair damaged cells. MSCs treat diseases like graft-versus-host disease and autoimmune disorders. They can be used alone or with other treatments.
What is microtransplantation, and how does it work?
Microtransplantation infuses small donor stem cells into the blood. It boosts the immune system to fight cancer. It’s a new approach for blood cancers.
What is haploidentical transplantation, and how does it expand the donor pool?
Haploidentical transplantation uses partially matched donor cells, often from family members. It increases the donor pool. Patients without a full match can find a haploidentical donor.
References
- American Cancer Society. (2024). Stem cell transplant for cancer. Retrieved September 24, 2025, fromhttps://www.cancer.org/cancer/managing-cancer/treatment-types/stem-cell-transplant.html
- U.S. National Library of Medicine. (2024). Peripheral blood stem cell transplant. Retrieved September 24, 2025, fromhttps://medlineplus.gov/peripheralbloodstemcelltransplant.html
- Parents’ Guide to Cord Blood Foundation. (2023). Cord blood transplant: Benefits and limitations. Retrieved September 24, 2025, fromhttps://parentsguidecordblood.org/en/cord-blood-transplant
- National Cancer Institute. (2024). Reduced-intensity conditioning. Retrieved September 24, 2025, fromhttps://www.cancer.gov/publications/dictionaries/cancer-terms/def/reduced-intensity-conditioning
- National Cancer Institute. (2024). CAR T-cell therapy: Engineering immune cells to fight cancer. Retrieved September 24, 2025, fromhttps://www.cancer.gov/about-cancer/treatment/types/immunotherapy/car-t-cells
- U.S. Food & Drug Administration. (2023). What is gene therapy?. Retrieved September 24, 2025, fromhttps://www.fda.gov/consumers/consumer-updates/what-gene-therapy