Last Updated on December 1, 2025 by Bilal Hasdemir
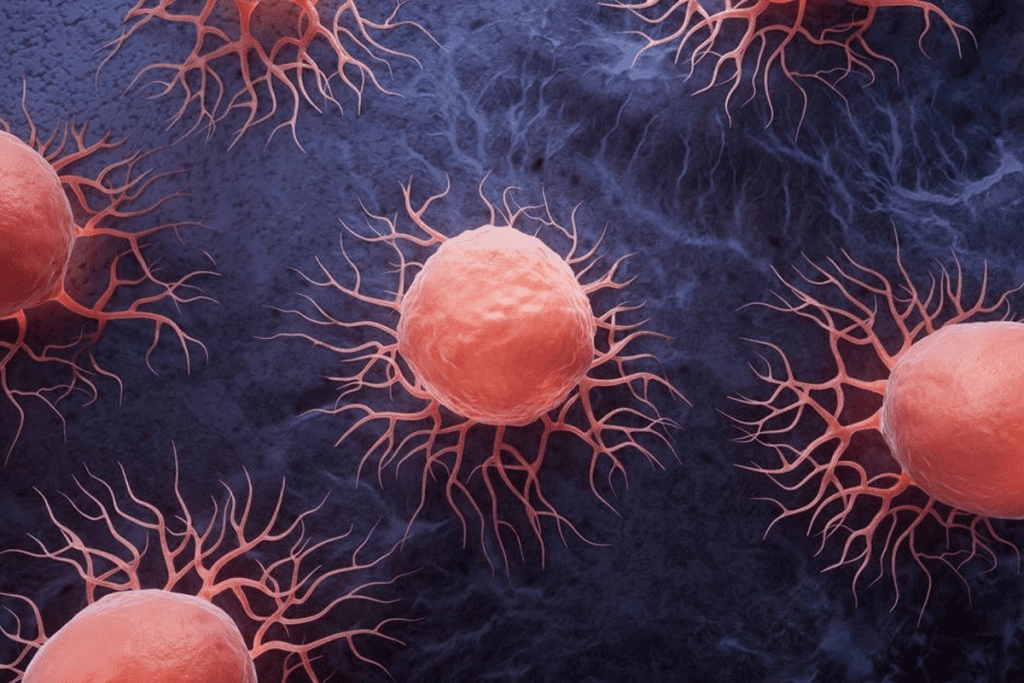
Mesenchymal stem cells are seen as a key player in regenerative medicine. They show promise in treating many health issues.
Bone Marrow MSCs are one of the most important types of mesenchymal stem cells in regenerative medicine. They play a vital role in repairing tissues, supporting immune balance, and treating many health issues. Recent studies highlight their ability to transform into bone, cartilage, and fat cells. Along with other MSC sources like adipose tissue and umbilical cord, bone marrow MSCs remain the gold standard for research and clinical use.
Recent studies have highlighted the diverse capabilities of these cells. They can turn into different cell types. This includes cells in bone, cartilage, and fat tissues.
The mesenchymal stem cells are versatile because they come from different places. This includes adipose tissue and bone marrow. Knowing about the different types of MSCs is important for using them to help people.
Key Takeaways
- Mesenchymal stem cells are a promising tool in regenerative medicine.
- They have the ability to differentiate into multiple cell types.
- The versatility of MSCs is attributed to their various sources.
- Understanding the different types of MSCs is important for their use.
- Research is ongoing to fully use the capabilities of these cells.
Understanding Mesenchymal Stem Cells (MSCs)
MSCs, or Mesenchymal Stem Cells, are special cells that can turn into many types of cells. They stick to plastic and have certain markers on their surface.
Definition and Basic Characteristics
MSCs are multipotent stromal cells that can become different cell types. These include osteoblasts, chondrocytes, and adipocytes. They stick to plastic and have markers like CD73, CD90, and CD105. But they don’t have markers like CD34 and CD45 found in blood cells.
| Characteristics | Description |
| Surface Markers | CD73, CD90, CD105 |
| Differential Potentia | Osteoblasts, Chondrocytes, Adipocytes |
| Hematopoietic Markers | Lack of CD34, CD45 |
Historical Discovery and Research Evolution
The discovery of MSCs started in the 1960s by Friedenstein and his team. They found cells in bone marrow that could change into different cell types. Ever after, research on MSCs has grown a lot. It has focused on how to get them, study them, and use them for healing.
Bone Marrow MSCs: The Gold Standard
BM-MSCs are seen as the top choice for MSC research. This is because they are well-studied and proven to be useful in treatments.
Isolation and Characterization Methods
To get BM-MSCs, scientists use density gradient centrifugation. This method sorts cells by density. It’s key to getting pure MSCs.
Characterization of BM-MSCs involves checking for certain surface markers. These markers are CD73, CD90, and CD105. They help identify MSCs and rule out other types of cells.
Unique Properties and Clinical Significance
BM-MSCs have immunomodulatory properties. They can adjust the immune system to help repair tissues. They can also turn into different cell types, which is great for fixing damaged tissues.
BM-MSCs are used in many clinical trials. They help with diseases like graft-versus-host disease, osteoarthritis, and heart problems. Their power comes from helping tissues heal and balancing the immune system.
| Source | Isolation Method | Clinical Applications |
| Bone Marrow | Density Gradient Centrifugation | Graft-versus-host disease, Osteoarthritis |
| Adipose Tissue | Enzymatic Digestion | Cosmetic Surgery, Tissue Repair |
| Dental Pulp | Enzymatic Digestion | Dental Tissue Repair, Regenerative Dentistry |
This table shows how BM-MSCs stand out. They have special uses and benefits compared to other sources like fat tissue and dental pulp. This shows their wide range of uses and their healing power.
Adipose-Derived MSCs
Adipose-derived mesenchymal stem cells (AD-MSCs) are a new option for stem cell therapy. They come from liposuction, which gives a lot of stem cells.
To get AD-MSCs, we first do liposuction. Then, we break down the tissue and spin it to get the stem cells. This method is easy and can give a lot of cells.
Extraction Procedures and Cell Yield
Getting AD-MSCs starts with liposuction. We take out fat tissue and then process it to get the stem cells. Enzymatic digestion breaks down the tissue, and then we spin it to separate the cells. This leaves us with a lot of AD-MSCs ready for use.
Research shows AD-MSCs can be made in big amounts. This makes them great for fixing damaged tissues. They are easier to get than stem cells from bone marrow.
Comparative Advantages to Other MSC Sources
AD-MSCs have big advantages over other stem cells. Getting them is easy because of liposuction. Getting stem cells from other places can be harder.
Studies say AD-MSCs are good for fixing tissues and controlling the immune system. They can turn into many cell types and help the body. This makes them a good choice for fixing damaged tissues.
Even though AD-MSCs look promising, we need to know more about them. We must study them more to use them safely and effectively in medicine.
Umbilical Cord MSCs
umbilical cord MSCs collection techniques
The umbilical cord is a rich source of MSCs. It offers a non-invasive way to collect these cells. This makes it a promising area for therapy.
Collection and Processing Techniques
UC-MSCs are taken from the umbilical cord after birth. This method is non-invasive and ethically acceptable. The MSCs are found in the Wharton’s jelly, a gel-like part of the cord.
Advanced processing techniques are used to get these cells ready for therapy. This involves breaking down the tissue and growing the cells in a controlled setting.
First, enzymes are used to release the MSCs from the tissue. Then, they are grown in a controlled environment. This is important to get enough cells for treatment.
Proliferation Capacity and Differentiation Potentia
UC-MSCs grow quickly in culture. They can also turn into different cell types like bone and fat cells. This makes them useful for many treatments.
These cells also have immunomodulatory properties. This means they can help the body accept transplants without rejecting them. Their ability to control the immune system is a big plus for therapy.
Placental MSCs
MSCs from the placenta are being studied for their immunomodulatory properties and possible uses in medicine. The placenta is a rich source of MSCs. It’s a non-invasive and less controversial source than other MSC sources.
Harvesting and Ethical Considerations
Getting MSCs from the placenta requires careful thought about ethics and procedure. Unlike bone marrow or fat, placental MSCs come from tissues that are usually thrown away after birth. This makes getting them less controversial.
Harvesting methods usually involve getting MSCs from the placental tissue. This can be done through enzymatic digestion or explant culture. These methods help get a lot of MSCs that are good for use in medicine.
Immunomodulatory Properties and Applications
Placental MSCs are known for their immunomodulatory properties. They can change the immune response and help fix damaged tissues. They make many cytokines and growth factors, which helps them treat inflammatory and autoimmune diseases.
| MSC Source | Immunomodulatory Properties | Clinical Applications |
| Placental MSCs | High cytokine secretion, immune response modulation | Regenerative medicine, autoimmune disease treatment |
| Endometrial MSCs | Supports endometrial regeneration, angiogenic potentia | Gynecological disorders, fertility treatments |
| Fetal Limb Bud MSCs | High proliferative capacity, multilineage differentiation | Tissue engineering, developmental biology studies |
The table shows the different immunomodulatory properties and clinical applications of MSCs from various sources, including the placenta. Scientists are always finding new ways these cells can help in regenerative medicine.
In conclusion, placental MSCs are a valuable resource in regenerative medicine. Their harvesting methods and immunomodulatory properties make them a good choice for many treatments.
Dental Pulp MSCs
dental pulp MSCs
Dental pulp mesenchymal stem cells (MSCs) are a new hope for healing. They come from the dental pulp, which is full of stem cells. These cells can turn into many different types of cells.
Extraction from Deciduous and Permanent Teeth
Getting MSCs from dental pulp is easy and works well. Dental pulp MSCs can be taken from both baby and adult teeth. This makes them a great source of stem cells. The process starts with taking out the dental pulp and then using enzymes to get the MSCs.
Studies show that MSCs from baby teeth grow faster than those from adult teeth. This makes baby teeth MSCs very useful for some treatments.
The process to get these cells is simple. And the cells act like MSCs should, turning into different cell types. This makes dental pulp MSCs very useful for healing.
Neural and Osteogenic Differentiation Capabilities
Dental pulp MSCs are special because they can turn into neural and osteogenic cells. This is great for fixing brain problems and bones. Research shows they can become like brain cells and bone-building cells.
They are better than some other MSCs, like those from bone marrow or fat. They are easy to get, too, from wisdom teeth or teeth pulled for orthodontics.
A study showed dental pulp MSCs are as good as bone marrow MSCs at making bone cells. This means they could be a great choice for fixing bones.
In short, dental pulp MSCs are a big hope for healing. They are easy to get and can turn into many types of cells. More research is needed to use them in medicine.
Amniotic Fluid and Cord Lining MSCs
Amniotic fluid and cord lining MSCs are becoming more popular. They are special because of their unique properties. These cells are taken from pregnancy and birth, making them a safe and ethical choice.
Collection During Pregnancy and Birth
These cells are collected during pregnancy or right after birth. Amniocentesis is used to get amniotic fluid, which is full of MSCs. The cord lining, often thrown away, also has MSCs that can be used.
This method is safe for both the mother and the baby. It’s why these MSCs are so attractive for medical use.
Regenerative Medicine Applications
These MSCs are very promising for regenerative medicine. They can turn into different cell types and help the body heal. They might help with wound healing, tissue repair, and degenerative diseases.
Studies show they can help fix damaged tissues and organs. This gives hope to those with hard-to-treat conditions. They are being compared to other MSC sources to see how they stack up.
The possibilities for amniotic fluid and cord lining MSCs are huge. Ongoing research is exploring their full benefits. As more is learned, they will likely become a key part of regenerative medicine.
Peripheral Blood and Endometrial MSCs
peripheral blood MSCs
Peripheral blood and endometrial MSCs have special qualities for different uses in medicine. They are found and used in various ways. Their unique traits are key for certain treatments in regenerative medicine.
Isolation Challenges and Techniques
Getting MSCs from blood and endometrial tissues is hard. This is because these cells are rare in these places. To get them, scientists use methods like density gradient centrifugation and immunoselection.
To get blood MSCs, scientists take blood samples and look for specific markers. For endometrial MSCs, they use tissue from biopsies or surgeries.
Comparison of Isolation Techniques
| Technique | Peripheral Blood MSCs | Endometrial MSCs |
| Density Gradient Centrifugation | Effective for initial isolation | Used in combination with other methods |
| Immunoselection | High specificity for MSC markers | Enhances purity of isolated MSCs |
Unique Biological Properties
Peripheral blood MSCs can change the immune system’s response. This makes them good for treating autoimmune diseases. Endometrial MSCs grow a lot and are great for fixing damaged tissues.
Both types of MSCs can turn into different cell types. They can become bone, cartilage, or fat cells. This ability to repair tissues is why they’re useful in medicine.
Compared to other MSC sources, blood and endometrial MSCs have big advantages. Their special qualities and the chance for personal treatments make them stand out in medicine.
Comparative Analysis of MSC Types in Clinical Settings
Studying MSCs from various sources is key to their use in medicine. This includes looking at their ability to change into different cell types and their healing powers. MSCs from bone marrow, fat, and umbilical cord are well-studied. Each has its own special traits and uses.
Differentiation Capabilities Across Sources
The ability of MSCs to change into different cells varies by source. Bone marrow MSCs can turn into bone, cartilage, and fat cells. Adipose-derived MSCs can also change into these cells and are easier to get. Umbilical cord MSCs grow fast and can turn into many cell types.
A study showed that:
- Bone marrow MSCs are best at making bone cells.
- Adipose-derived MSCs are great at making fat cells.
- Umbilical cord MSCs are excellent at making cartilage cells.
Therapeutic Potentials and Limitations
MSCs have many uses in medicine, like fixing damaged tissues and boosting the immune system. Bone marrow MSCs are used to treat diseases like graft-versus-host disease. Adipose-derived MSCs are being looked at for cosmetic and tissue engineering uses. Umbilical cord MSCs are studied for their ability to calm the immune system and treat brain diseases.
But, MSCs also have challenges, such as:
- They might be rejected by the body and need drugs to stop this.
- They could turn into the wrong cells or help tumors grow.
- The quality and strength of MSCs can vary a lot.
In summary, comparing MSCs from different places shows their unique powers and uses. Knowing these differences is important for using them in medicine.
Conclusion
Mesenchymal stem cells (MSCs) are a big hope for regenerative medicine. They could solve many medical problems. MSCs come from different places like bone marrow, fat, and umbilical cords.
MSCs are special because they can help in many ways. Scientists are learning more about them every day. This means MSCs could help with many serious health issues in the future.
We need to keep studying MSCs to use them to their fullest. But what we know so far is very promising. It looks like MSCs could lead to new ways to treat diseases.
FAQ
What are mesenchymal stem cells (MSCs) and their significance in regenerative medicine?
MSCs are special stem cells that can turn into different cell types. They are important in regenerative medicine because they help fix tissues and control the immune system.
What are the different sources of MSCs?
MSCs can come from many places. These include bone marrow, fat tissue, umbilical cord, placenta, dental pulp, amniotic fluid, cord lining, blood, and endometrium.
What are the advantages of using bone marrow MSCs?
Bone marrow MSCs are the top choice because they are well-studied and have special qualities. But, getting them can be hard and might hurt the donor.
How do adipose-derived MSCs compare to other MSC sources?
Adipose-derived MSCs are more accessible and yield higher cell counts compared to bone marrow-derived MSCs. They also work well in the body and can change into different cell types.
What are the ethical considerations surrounding the use of placental MSCs?
Using placental MSCs can be tricky because of concerns about getting the tissue. But, they can help the body and have been used in medicine.
What are the unique properties of dental pulp MSCs?
Dental pulp MSCs can become nerve or bone cells. They are great for fixing teeth and face problems.
How do amniotic fluid and cord lining MSCs compare to other MSC sources?
Amniotic fluid and cord lining MSCs grow fast and can change into many cell types. They are good for fixing the body and have been used in medicine.
What are the challenges associated with isolating MSCs from peripheral blood and endometrium?
Getting MSCs from blood and endometrium is hard because there are few cells. But, these MSCs have special qualities and can help the body.
How do different MSC types compare in terms of their differentiation capabilities and therapeutic potentials?
Different MSC types can change into different cells and help the body in different ways. It’s important to study each type to find the best one for each need.
References
- Mahmood, R., Shaukat, M., & Choudhery, M. S. (2018). Biological properties of mesenchymal stem cells derived from adipose tissue, umbilical cord tissue and bone marrow. AIMS Cell and Tissue Engineering, 2(2), 78“90. https://doi.org/10.3934/celltissue.2018.2.78
- Hass, R., Kasper, C., Böhm, S., & Jacobs, R. (2011). Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue‘derived MSC. Cell Communication and Signaling, 9, Article 12. https://doi.org/10.1186/1478‘811X‘9‘12
- Clinical utility of mesenchymal stem/stromal cells in regenerative medicine and cellular therapy. (2023). Journal of Biological Engineering, 17, Article 44. https://doi.org/10.1186/s13036‘023‘00361‘9
- Pittenger, M. F., Mackay, A. M., Beck, S. C., Jaiswal, R. K., Douglas, R., Mosca, J. D., … & Marshak, D. R. (1999). Multilineage potential of adult human mesenchymal stem cells. Science, 284(5411), 143“147. https://doi.org/10.1126/science.284.5411.143
- Zuk, P. A., Zhu, M., Ashjian, P., De Ugarte, D. A., Huang, J. I., Mizuno, H., … & Hedrick, M. H. (2002). Human adipose tissue is a source of multipotent stem cells. Molecular Biology of the Cell, 13(12), 4279‘4295. https://doi.org/10.1091/mbc.e02‘02‘0092