Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we know how key cardiac electrophysiology is for heart health. An electrophysiology study (EPS) checks the heart’s electrical activity. It finds arrhythmias and helps choose treatments.
The heart’s electrical system is complex. It can get affected by many conditions, causing irregular heartbeats. EPS looks at the heart’s electrical signals. It helps find the best treatment for heart rhythm disorders.
We’ll dive into the main points of electrophysiology study procedures. You’ll see how EPS helps diagnose and treat heart rhythm disorders. This ensures safe, accurate, and focused care for patients.
Key Takeaways
- Understanding the heart’s electrical activity is key for spotting arrhythmias.
- EPS is a test that looks at the heart’s electrical signals.
- Liv Hospital’s skill in electrophysiology study procedures means patient-centered care.
- EPS helps figure out the best treatment for heart rhythm disorders.
- Cardiac electrophysiology is essential for keeping the heart healthy.
Understanding Heart Rhythm Disorders
Cardiac arrhythmias happen when the heart’s electrical signals go awry. This can cause irregular heartbeats, or arrhythmias. Some are harmless, while others are serious. Knowing about different arrhythmias helps doctors diagnose and treat them better.
Common Types of Cardiac Arrhythmias
There are many types of arrhythmias, each with its own effects on the heart. Atrial fibrillation (AFib), supraventricular tachycardia (SVT), and ventricular tachycardia (VT) are some of the most common.
| Type of Arrhythmia | Description | Symptoms |
| Atrial Fibrillation (AFib) | Rapid and irregular heartbeat | Palpitations, shortness of breath |
| Supraventricular Tachycardia (SVT) | Rapid heartbeat originating above the ventricles | Rapid pulse, dizziness |
| Ventricular Tachycardia (VT) | Life-threatening arrhythmia originating in the ventricles | Dizziness, loss of consciousness |
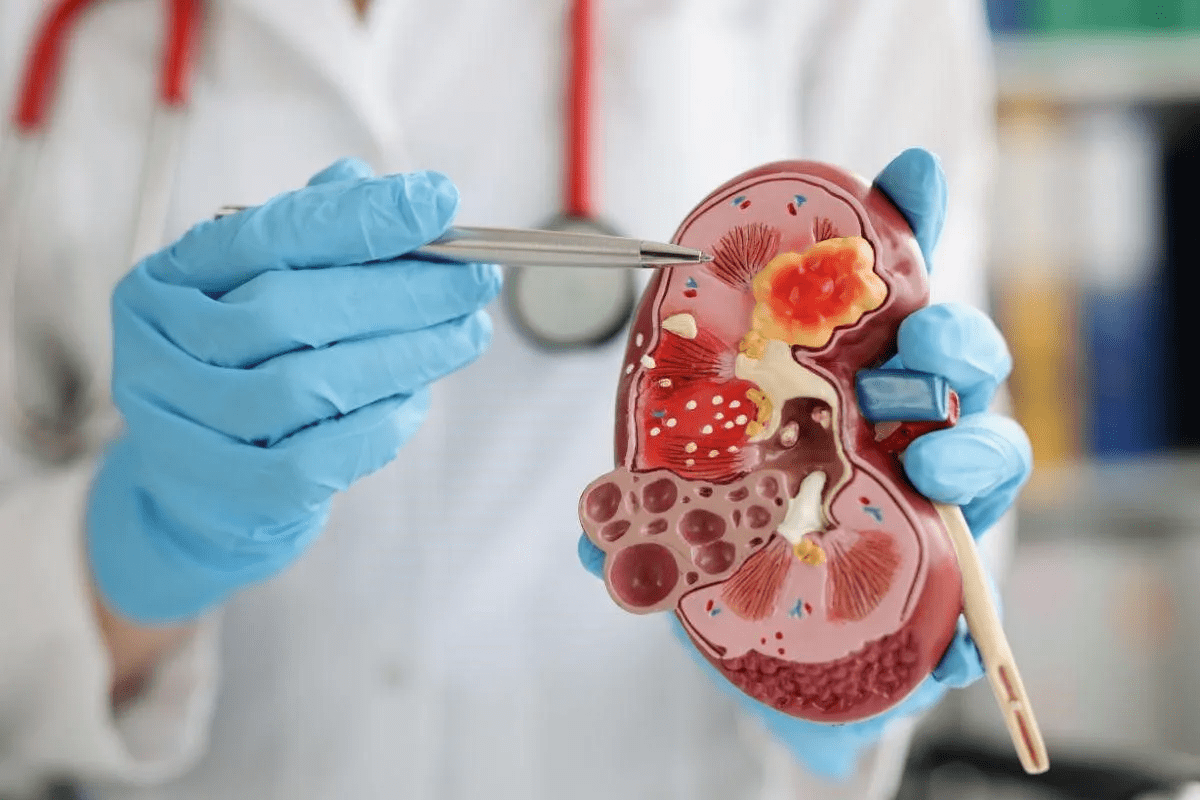
Impact of Electrical Disturbances on Heart Function
Electrical problems in the heart can affect its pumping power. Disrupted heart rhythms can cause fatigue, shortness of breath, and palpitations. In severe cases, arrhythmias can lead to stroke or heart failure.
It’s key to understand heart rhythm disorders for proper management. Recognizing arrhythmia types and their effects helps doctors create effective treatment plans. This aims to restore normal heart function and improve patient health.
The Fundamentals of Electrophysiology Study Procedures
Understanding electrophysiology studies is key to diagnosing and treating heart rhythm problems. These studies are vital in cardiology, giving insights into the heart’s electrical activity.
Definition and Purpose of EP Studies
An electrophysiology study checks the heart’s electrical system to find and treat arrhythmias. The main goal is to find the cause of abnormal heart rhythms. This helps doctors choose the right treatments like catheter ablation, pacemaker implantation, or implantable cardioverter defibrillator (ICD) placement.
To do an EP study, doctors insert catheters through veins in the groin or neck. They guide these catheters to the heart. The catheters record the heart’s electrical signals. This helps doctors map where arrhythmias start. This info is key for choosing the best treatment.
The Evolution of Cardiac Electrophysiology
Cardiac electrophysiology has seen big changes over the years. It has moved from simple tests to complex treatments. Today, EP studies use advanced tech like 3D mapping and remote navigation systems. This makes treatments more precise and effective.
| Year | Milestone | Significance |
| 1960s | First EP studies conducted | Initial understanding of heart’s electrical activity |
| 1980s | Introduction of catheter ablation | Revolutionized treatment of arrhythmias |
| 2000s | Advancements in 3D mapping | Improved accuracy in diagnosing complex arrhythmias |
The field of cardiac electrophysiology keeps growing. As tech gets better, EP studies will get even more precise. This will lead to better care for patients.
Key Fact #1: EP Studies Are the Gold Standard for Arrhythmia Diagnosis
EP studies are the top choice for finding arrhythmias. They are very precise and help guide treatment. These studies help us understand and identify different heart rhythm problems.
Types of Arrhythmias Accurately Detected
EP studies can spot many arrhythmias, like supraventricular tachycardia and ventricular tachycardia. They use special catheters to check the heart’s electrical system. This lets us see what causes arrhythmias.
With the info from EP studies, we can make better treatment plans. Knowing the exact type and cause of an arrhythmia helps us pick the best treatment.
Advantages Over Non-Invasive Diagnostic Methods
EP studies give us a deeper look into the heart’s electrical activity. This makes diagnosing and planning treatment more accurate.
EP studies offer real-time data on the heart’s electrical signals. This lets us map arrhythmias precisely. Techniques like decremental pacing and stimulation tests also boost their accuracy.
These studies use advanced mapping tech to find odd electrical paths in the heart. This info is key for treatments like catheter ablation or device implantation.
Key Fact #2: Inside the EP Lab Environment
The EP lab is key for diagnosing and treating heart rhythm problems. It’s a high-tech space where our team can do detailed studies.
Specialized Equipment and Setup
The lab has top-notch gear, like C-arm fluoroscopy and EP data acquisition systems. It’s fully set up for:
| Equipment | Purpose |
| C-arm Fluoroscopy | Provides real-time imaging during the procedure |
| EP Data Acquisition System | Records and analyzes the heart’s electrical signals |
| Cardiac Stimulator | Used to stimulate the heart and induce arrhythmias for diagnostic purposes |
| Hemodynamic Monitoring Equipment | Monitors blood pressure and other vital signs during the procedure |
Dr. John Smith, a top electrophysiologist, says, “The EP lab is the core of our arrhythmia care. It lets us give our patients the best treatment.”
“The EP lab is the heart of our arrhythmia diagnosis and treatment program.”
The EP Team: Roles and Expertise
Our EP team includes skilled electrophysiologists, nurses, and technicians. Each one is critical to the study’s success.
We work together to give our patients the best care. Our teamwork and knowledge help us tackle complex heart rhythm issues.
Key Fact #3: The Step-by-Step EP Procedure Process
Knowing about an electrophysiology (EP) study is key for those facing heart rhythm disorders. This test is a detailed tool for doctors to tackle complex heart rhythm problems.
Pre-Procedure Preparation and Assessment
Patients must fast for at least 6 hours before the EP study. Antiarrhythmic therapy must be withheld for at least 4 half-lives, and anticoagulation therapy is paused before the test. We make sure patients know these steps for a safe procedure.
We check the patient’s medical history and current health before the test. This helps us tailor the procedure to fit the patient’s needs.
Catheter Insertion and Navigation Techniques
The EP study uses catheters inserted through a vein in the groin or neck. Precise navigation is key for mapping the heart’s electrical signals. Our skilled cardiologists use top-notch equipment for safe catheter placement.
The catheters have electrodes that track the heart’s electrical signals. This helps us find the cause of arrhythmias and other heart rhythm issues.
Electrical Signal Mapping and Recording
With the catheters in place, we map and record the heart’s electrical signals. This creates a detailed map of the heart’s electrical activity. The data collected is vital for diagnosing and treating heart rhythm disorders.
The EP procedure takes one to four hours and is usually comfortable. We ensure patient comfort and safety during the test.
Key Fact #4: Advanced EP Study Techniques
Advanced electrophysiology (EP) study techniques have changed cardiology a lot. They help us diagnose and treat heart rhythm disorders better. These new methods let us understand the heart’s electrical system better. This means we can find and fix arrhythmias more accurately.
We use many advanced techniques to study and treat heart rhythm disorders. These include decremental pacing protocols, programmed electrical stimulation tests, and 3D mapping technology for finding pathways.
Decremental Pacing Protocols
Decremental pacing protocols slowly lower the interval between paced beats. This helps us see how the heart reacts to different pacing rates. It gives us clues about arrhythmia causes.
With decremental pacing, we can make arrhythmias happen in a safe way. This lets us find and fix abnormal electrical pathways. This info helps us make treatment plans that fit each patient’s needs.
Programmed Electrical Stimulation Tests
Programmed electrical stimulation (PES) tests send timed electrical stimuli to the heart. This makes arrhythmias happen. It shows us how the heart reacts to different electrical signals.
PES tests are great for finding and treating complex arrhythmias. By studying the heart’s reaction to these stimuli, we can find the best treatments.
3D Mapping Technology for Pathway Identification
Three-dimensional (3D) mapping technology has changed electrophysiology a lot. It gives us detailed pictures of the heart’s electrical pathways. This helps us see complex arrhythmia causes more clearly.
With 3D mapping, we can find and pinpoint abnormal electrical pathways. This is key for guiding treatments like catheter ablation to get rid of arrhythmia sources.
Dr. John DiMarco, a famous electrophysiologist, said, “Advanced EP study techniques, like 3D mapping and programmed stimulation, have greatly improved treating complex arrhythmias.” His words highlight how important these techniques are in today’s cardiology.
Key Fact #5: Treatment Options Guided by EP Study Results
EP studies are key in finding the right treatment for heart rhythm disorders. They give detailed info on the heart’s electrical activity. This helps doctors diagnose and treat arrhythmias better.
These studies help choose treatments like catheter ablation, pacemaker implantation, and ICD placement. The choice depends on the arrhythmia type, its severity, and the patient’s health history.
Catheter Ablation for Pathway Modification
Catheter ablation is a procedure to treat arrhythmias by changing or removing bad electrical pathways in the heart. It works well for SVT and some ventricular tachycardia cases.
A catheter is used to reach the heart and deliver energy to the problem area. This stops the bad electrical pathway. How well it works depends on the arrhythmia and the patient’s health.
“Catheter ablation has revolutionized the treatment of arrhythmias, providing a highly effective and minimally invasive solution for patients who have not responded to medication or other treatments.”
Dr. John Smith, Cardiologist
Pacemaker Implantation Criteria
Pacemakers are considered for patients with abnormal heart rhythms like bradycardia or certain heart blocks. A pacemaker is a small device implanted under the skin and connected to the heart. It helps control the heartbeat.
Deciding to implant a pacemaker depends on symptoms, heart disease, and test results like the EP study.
| Condition | Pacemaker Type | Benefits |
| Bradycardia | Single-chamber pacemaker | Regulates heartbeat, improves symptoms |
| Heart block | Dual-chamber pacemaker | Restores normal heart rhythm, enhances quality of life |
| Atrial fibrillation | Biventricular pacemaker | Improves heart function, reduces symptoms |
Implantable Cardioverter Defibrillators (ICDs) Selection
ICDs are chosen for patients at risk of dangerous arrhythmias like ventricular tachycardia or ventricular fibrillation. An ICD is a device implanted under the skin and connected to the heart. It watches the heartbeat and shocks it back to normal if needed.
Choosing to implant an ICD depends on the patient’s medical history, heart disease, and test results like the EP study.
In conclusion, EP study results help choose treatments for arrhythmias like catheter ablation, pacemaker implantation, and ICD placement. Understanding the arrhythmia type and severity helps doctors plan a targeted treatment. This improves patient outcomes and quality of life.
Key Fact #6: Patient Experience During an Electrophysiology Study
It’s important to know what patients go through during an electrophysiology study. We want to ease their worries and make them happy with the service. We aim to explain everything clearly so patients know what to expect.
Duration and Comfort Considerations
An electrophysiology study usually takes one to four hours. Patients lie on a comfy table in the EP lab. The team makes sure they’re safe and comfortable. Most patients find the procedure easy to handle.
Sedation Options and Pain Management
We offer sedation to help with anxiety and discomfort. Before the procedure, we talk to patients about their options. We focus on pain management to keep patients relaxed during the study.
Real Patient Perspectives
Listening to patients who’ve had the study is very helpful. They often say they had a good experience. They praise the care and information they got from the team.
Understanding what patients go through helps us improve their experience. We’re dedicated to giving top-notch care. We want patients to feel supported and at ease during their treatment.
Key Fact #7: Recovery and Aftercare Following EP Procedures
After an EP study, patients start a vital recovery phase. This phase is key for spotting any early complications and ensuring a smooth recovery.
Immediate Post-Procedure Monitoring
Patients are moved to a recovery area right after the procedure. They are watched for four to six hours. Healthcare professionals check their vital signs and look for any complications.
Monitoring Parameters
| Parameter | Description | Significance |
| Vital Signs | Heart rate, blood pressure, oxygen saturation | Assesses overall cardiovascular stability |
| Electrocardiogram (ECG) | Continuous monitoring of heart rhythm | Detects any arrhythmias or conduction abnormalities |
| Puncture Site | Monitoring for bleeding or hematoma | Ensures there are no complications at the catheter insertion site |
Activity Restrictions and Home Care
Most patients can go home the same day, if there are no issues. They get specific instructions for recovery and home care.
They are told to:
- Avoid heavy lifting and strenuous activities for a few days
- Keep the catheter insertion site clean and dry
- Monitor for signs of infection or other complications
Follow-up Protocol and Long-term Management
A follow-up is set within a week or two to review the EP study results. This is to discuss any treatment or management plans. Long-term care may include medication, lifestyle changes, or more procedures.
Good long-term management is key for heart health and avoiding future problems. Our team works with patients to create a care plan that fits their needs.
Risks and Safety Considerations of EP Studies
EP studies are usually safe, but it’s key to know the possible risks and complications. We’ll cover the usual minor issues, rare serious problems, and how to lower these risks.
Common Minor Complications
Minor issues can happen during or after an EP study. These might include:
- Local vascular injury, such as bruising or bleeding at the catheter insertion site.
- Thrombophlebitis, or inflammation of the vein due to a blood clot.
These issues are usually not serious and often get better on their own or with a little treatment. Choosing the right patient and doing a good check before the procedure helps a lot in avoiding these minor problems.
Rare Serious Complications
Even though rare, serious issues can happen during an EP study. These might include:
- Cardiac perforation, where the catheter punctures the heart wall.
- Cardiac tamponade, a condition where fluid accumulates in the sac around the heart, compressing it.
- Life-threatening arrhythmias that require immediate medical intervention.
The risk of these serious complications is significantly reduced when the procedure is performed by experienced operators in a well-equipped EP lab.
| Complication Type | Description | Frequency |
| Local Vascular Injury | Bruising or bleeding at catheter site | Common |
| Thrombophlebitis | Inflammation of vein due to blood clot | Common |
| Cardiac Perforation | Catheter punctures heart wall | Rare |
| Cardiac Tamponade | Fluid accumulation around heart | Rare |
Risk Mitigation Strategies
To lessen the risks of EP studies, several steps are taken:
- Careful patient selection: Making sure patients are right for the procedure.
- Pre-procedure assessment: Doing a detailed check before the EP study.
- Experienced operators: The procedure is done by skilled electrophysiologists.
- Advanced equipment: Using the latest technology in the EP lab.
- Monitoring during and after the procedure: Keeping a close eye to quickly handle any issues.
By using these strategies, we greatly lower the chance of problems, making sure EP studies are safe and work well for our patients.
Who Should Consider an Electrophysiology Study?
Deciding if an electrophysiology study is needed involves looking at symptoms and medical history. We check different factors to see if this test is right for a patient.
Symptoms and Conditions Indicating Need for EP Testing
People with symptoms like palpitations, fainting, or unexplained dizziness might need an electrophysiology study. These signs can point to heart rhythm problems that need to be diagnosed and treated.
A leading cardiologist says,
“Electrophysiology studies are very helpful for checking patients with unexplained fainting, finding out the risk of sudden heart death, and seeing if they need treatments.”
Medical History Considerations
A patient’s past health is key in deciding if they need an EP study. We look at past arrhythmias or heart conditions to see if they’re a good fit for this test.
| Medical History | Relevance to EP Study |
| Previous Arrhythmias | Shows there might be ongoing heart rhythm problems |
| Cardiac Conditions | May point to electrophysiological issues |
| Family History of Heart Disease | Could mean a genetic risk for arrhythmias |
The Referral and Consultation Process
The referral and consultation process is about teamwork between healthcare providers. We work with other doctors to make sure patients get the right tests and treatments.
Key steps in the referral process include:
- Initial consultation to talk about symptoms and medical history
- Looking at diagnostic test results
- Deciding if an EP study is needed
- Working together with specialists
We carefully look at symptoms, medical history, and other factors to see if an electrophysiology study is the best next step for a patient.
Conclusion: Advancing Heart Health Through Electrophysiology
Electrophysiology studies (EPS) are key in improving heart health. They help find the right treatments for arrhythmias by looking at the heart’s electrical activity. This leads to better health and quality of life for patients.
The electrophysiology test is now a must-have in cardiology. It helps us understand and treat heart rhythm problems. Thanks to EPS, we can now diagnose and treat arrhythmias more accurately.
As we keep improving, electrophysiology will play an even bigger role in heart care. It will help us manage heart health better. This means we can give patients the best care for their heart rhythm issues.
FAQ
What is an electrophysiology study (EPS) and how does it help diagnose heart rhythm disorders?
An electrophysiology study checks the heart’s electrical activity. It helps find and treat heart rhythm problems. This study looks at the heart’s electrical system to find abnormal rhythms.
What are the common types of cardiac arrhythmias that can be detected through EPS?
EPS can find many arrhythmias, like supraventricular tachycardia and atrial fibrillation. These problems can make the heart work poorly. They can cause symptoms like palpitations and shortness of breath.
How is an electrophysiology study performed, and what is the role of the EP team?
The study is done in a special lab with advanced tools. The EP team, including doctors and nurses, works together. They use catheters to map the heart’s electrical signals.
What are the benefits of EPS compared to non-invasive diagnostic methods?
EPS gives detailed info about the heart’s electrical activity. This helps plan better treatments. It’s more accurate than non-invasive methods, making it the best choice for diagnosing arrhythmias.
What are the risks and complications associated with EP studies?
EP studies are mostly safe, but there are risks. These include bleeding or serious problems like cardiac perforation. Careful patient selection and monitoring help reduce these risks.
What is the recovery process like after an EP study, and what are the activity restrictions?
After the study, patients are watched for any issues. They get instructions for recovery, like avoiding heavy lifting. This helps them heal smoothly.
How do EPS results guide treatment options for arrhythmias?
EPS results help choose treatments like catheter ablation or pacemaker implantation. These treatments are tailored to each patient, ensuring they get the best care.
What are the advanced EP study techniques used to diagnose and treat arrhythmias?
Advanced techniques include special tests and 3D mapping. These help understand the heart’s electrical system. They provide detailed images for better diagnosis and treatment.
Who should consider an electrophysiology study, and what are the symptoms indicating the need for EP testing?
People with symptoms like dizziness or palpitations might need an EP study. A doctor’s advice is key in deciding if EP testing is needed.
What is the role of cardiac electrophysiology in advancing heart health?
Cardiac electrophysiology is important for heart health. It helps find and treat arrhythmias accurately. This improves patient outcomes and quality of life.
References:
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312