Last Updated on November 25, 2025 by Ugurkan Demir

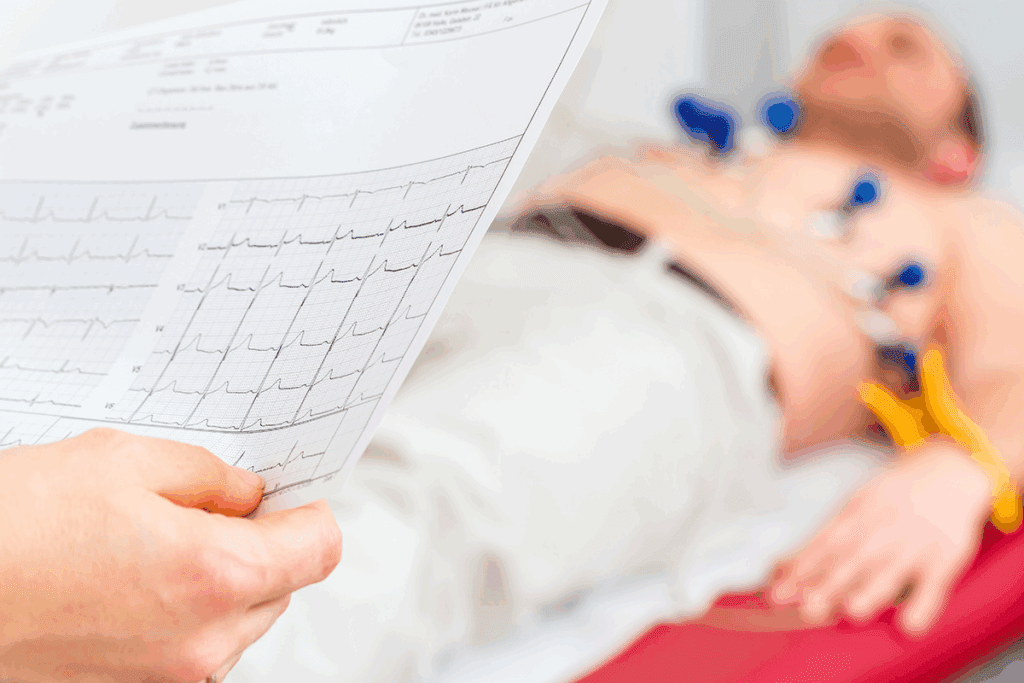
Spotting third-degree heart block on ECG quickly is critical. It can save lives. At Liv Hospital, we focus on top-notch healthcare for all patients, including those from abroad.
Third-degree AV block stops electrical signals from the atria reaching the ventricles. This causes the heart’s upper and lower chambers to beat out of sync. On an ECG, you’ll see P waves and QRS complexes that don’t match up. The atrial rate is always higher than the ventricular rate.
Key Takeaways
- Third-degree AV block is a serious cardiac condition requiring prompt attention.
- ECG findings are key for diagnosing third-degree AV block.
- AV dissociation is a hallmark of third-degree AV block on ECG.
- P waves and QRS complexes occur independently in third-degree AV block.
- The atrial rate is consistently higher than the ventricular rate in third-degree AV block.
What Is 3rd Degree Heart Block? Pathophysiology and Significance
Third-degree heart block, also known as complete AV block, is a serious heart condition. It stops electrical signals from moving between the atria and ventricles. This makes the atria and ventricles beat on their own, which can be very dangerous if not treated right away.
Definition and Mechanism of Complete AV Block
Complete AV block happens when the electrical path between the atria and ventricles is broken. This can occur at different levels, like the AV node or the bundle of His. As a result, the SA node’s electrical signals can’t reach the ventricles, causing AV dissociation.
The ventricles then start an escape rhythm to keep the heart beating. This rhythm can start from the AV junction or the ventricles. Knowing the rate and width of this rhythm helps doctors understand where and why the block is happening.
Epidemiology and Common Causes
Third-degree heart block can be caused by many things, including:
- Heart attack or myocardial infarction, which can damage the electrical conduction system.
- Cardiomyopathy, a disease of the heart muscle that can affect the heart’s electrical activity.
- Serious injury to the chest, which can disrupt the heart’s normal functioning.
- Genetic heart conditions that affect the electrical conduction system.
- Certain infections and inflammatory conditions that can impact the heart.
- Electrolyte imbalance, which can affect the heart’s electrical activity.
- Lyme disease, an infection known to cause heart block in some cases.
- Myocardial fibrosis, scarring of the heart tissue that can disrupt electrical pathways.
- Open heart surgery, which can inadvertently damage the conduction system.
- Overdose of certain drugs that affect heart rhythm.
- Valve disease, conditions affecting the heart valves that can also impact the conduction system.
Knowing what causes third-degree heart block is key to diagnosing and treating it. This condition is serious because it can lead to slow heart rates and less blood flow. Quick medical action is needed to prevent serious problems.
The Fundamental Concept: AV Dissociation Explained

AV dissociation is a key idea behind third-degree heart block ECG findings. It shows how the normal rhythm between the heart’s upper and lower chambers is broken.
Independent Atrial and Ventricular Activity
In third-degree heart block, the atria and ventricles beat on their own. This is because there’s a complete block in the electrical signals between them.
The atria beat faster because they’re controlled by the sinoatrial (SA) node. This node fires more often than the ventricles’ natural rate.
Key features of independent atrial and ventricular activity include:
- The atria and ventricles contract at their own rates.
- The atrial rate is consistently higher than the ventricular rate.
- There is no association between P waves and QRS complexes on the ECG.
P Waves and QRS Complexes: The Disconnection
The disconnection between P waves and QRS complexes is a key sign of AV dissociation in third-degree heart block. On the ECG, P waves don’t lead to QRS complexes, and QRS complexes happen without P waves.
P waves show when the atria depolarize, while QRS complexes show ventricular depolarization. In AV dissociation, these happen separately. This means there’s no coordination between atrial and ventricular contractions.
- P waves occur at a regular interval (PP interval) but are not associated with QRS complexes.
- QRS complexes occur at a slower rate than P waves and are not preceded by P waves.
- The PR interval is variable and not consistent, as there is no fixed relationship between P waves and QRS complexes.
Recognizing 3rd Degree Heart Block ECG Patterns
Third-degree AV block shows up on an ECG with specific signs. These signs help doctors tell it apart from other heart blocks. The diagnosis is based on these patterns seen on a 3rd degree block ECG strip.
One key sign of third-degree AV block is the lack of connection between atrial and ventricular activity. This is shown on the ECG as no link between P waves and QRS complexes.
Complete Absence of PR Interval Relationship
In third-degree AV block, there’s no PR interval relationship. The PR interval, which shows when the heart starts to beat, is not steady. This is because atrial and ventricular electrical activities are separate.
“The lack of a steady PR interval is key to spotting third-degree AV block,” say cardiology experts.
Regular P Waves with Constant PP Interval
Even though atrial and ventricular activities are separate, the atrial rhythm is regular. The PP interval, which shows how often the atria beat, stays the same. This means the SA node is working right, and the atria are beating at a steady rate.
Variable RR Intervals and Their Significance
The RR interval, which shows how often the ventricles beat, can change. This change is because of the ventricular escape rhythm. It can be affected by where the block is and the ventricular rate.
The variable RR intervals on an ECG are important. They show the ventricular rate isn’t controlled by the normal heart pacemaker. Instead, a ventricular escape pacemaker is in charge. This can cause different health problems.
Knowing these ECG patterns is key for diagnosing and treating 3rd degree AV block. Doctors need to be able to read 3rd degree heart block rhythm strips well to give the right care.
7 Critical ECG Findings in Complete AV Block
To diagnose third-degree AV block, doctors look closely at the ECG for seven key signs. These signs help them understand the condition and how to care for the patient.
1. AV Dissociation: The Hallmark Finding
The main sign of third-degree AV block is AV dissociation. This means the heart’s upper and lower chambers beat independently. P waves and QRS complexes don’t match up.
2. Atrial Rate Consistently Higher Than Ventricular Rate
In complete AV block, the heart’s upper chambers beat faster than the lower chambers. The upper chambers keep their normal rhythm. But, the lower chambers beat slower, controlled by a different pacemaker.
3. Regular P Waves with No Relationship to QRS
P waves show a steady rhythm in the upper chambers. But, they don’t follow the QRS complexes, showing no connection between the two.
4. Escape Rhythm Characteristics
The lower chambers’ rhythm in third-degree AV block is kept by an escape rhythm. This rhythm can start from the AV junction or the ventricles. Its rate and QRS width give clues about the block’s location and its effects on the heart.
In third-degree AV block with a junctional escape rhythm, the QRS complexes are narrow. This means the ventricles are activated through the normal His-Purkinje system. On the other hand, ventricular escape rhythms cause wide QRS complexes.
Knowing these seven ECG signs is key to diagnosing and treating third-degree AV block. By studying the ECG, doctors can spot these signs and plan the right treatment.
Junctional Escape Rhythm in Third Degree AV Block
In third-degree AV block, a junctional escape rhythm is key. It helps keep the heart beating when the usual path is blocked.
Narrow QRS Complex Characteristics (35-50 BPM)
A junctional escape rhythm has narrow QRS complexes. These complexes beat between 35-50 BPM. This is slower than normal but faster than ventricular rhythms, making it more stable.
“The junctional escape rhythm acts as a safety net,” studies in cardiology say. It keeps the ventricular rate steady when normal AV conduction fails.
Stability and Reliability Factors
The stability of a junctional escape rhythm depends on several things. These include the heart’s condition and any other conduction problems. It’s seen as more reliable than ventricular rhythms because of its faster rate and consistent shape.
- Reliable backup mechanism in complete AV block
- Faster rate compared to ventricular escape rhythms
- Narrow QRS complexes indicating supraventricular origin
ECG Examples and Interpretation
When looking at ECGs with third-degree AV block and junctional escape rhythm, look for AV dissociation. Also, check for a steady ventricular rate. The P waves and QRS complexes will be separate, with narrow QRS complexes unless there’s a bundle branch block.
ECG examples usually show a regular junctional rhythm. This rhythm beats between 35-50 BPM. There’s no link between P waves and QRS complexes. Spotting these signs is key to diagnosing third-degree AV block with a junctional escape rhythm.
Ventricular Escape Rhythm: Wide QRS Patterns
Third-degree heart block means no AV conduction. This leads to ventricular escape rhythms. These rhythms have wide QRS complexes and beat slower than junctional rhythms.
Morphology and Rate Characteristics
Ventricular escape rhythms have wide QRS complexes because they start in the ventricles. They beat between 20-40 times per minute. This slow rate can lower cardiac output a lot.
The key traits of ventricular escape rhythms are:
- Wide QRS complexes (>120 ms)
- Slow rate (20-40 bpm)
- Originates from ventricular tissue
- Often irregular
Hemodynamic Consequences and Risks
The effects of ventricular escape rhythms on the heart are big. Their slow and irregular beat can cut down cardiac output. This can cause dizziness, fatigue, and shortness of breath.
People with ventricular escape rhythms face bigger risks. These include:
- Syncope or near-syncope from poor blood flow to the brain
- Heart failure from long periods of low heart output
- Higher chance of ventricular arrhythmias
Identifying Ventricular Origin on ECG
- Wide QRS complexes (>120 ms)
- AV dissociation (P waves and QRS complexes are independent)
- Slow ventricular rate (20-40 bpm)
- Lack of association between P waves and QRS complexes
Spotting these signs is key to diagnosing third-degree heart block and figuring out the rhythm.
Comparing 3rd Degree Block with 1st and 2nd Degree AV Blocks
It’s important to know the differences between AV block degrees for correct diagnosis and treatment. AV blocks are divided into degrees based on how bad the conduction problem is. This affects how doctors treat them.
Key Differentiating Features on ECG
The electrocardiogram (ECG) is key in telling apart 1st, 2nd, and 3rd degree AV blocks. Knowing the ECG signs of each is essential.
1st degree AV block shows a PR interval longer than 0.2 seconds. But, every P wave is followed by a QRS complex. On the other hand, 2nd degree AV block has two types: Mobitz I (Wenckebach) and Mobitz II. Mobitz I shows PR prolongation until a P wave is blocked. Mobitz II blocks P waves without prolonging the PR interval.
3rd degree AV block, or complete AV block, shows no connection between atrial and ventricular activity. The atrial rate is usually faster than the ventricular rate. There’s no link between P waves and QRS complexes.
Progressive Conduction Abnormalities
Going from 1st degree to 3rd degree AV block shows a worsening of AV conduction. Knowing this progression helps predict complications and plan treatment.
| AV Block Degree | ECG Characteristics | Clinical Implication |
| 1st Degree | Prolonged PR interval (>0.2 sec) | Usually asymptomatic, but may progress |
| 2nd Degree Mobitz I | Progressive PR prolongation until blocked P wave | May be benign or progress to higher degree block |
| 2nd Degree Mobitz II | Intermittent blocked P waves without PR prolongation | Higher risk of progression to complete AV block |
| 3rd Degree | Complete AV dissociation, P waves and QRS complexes unrelated | Often symptomatic, requiring pacemaker implantation |
Clinical Significance of Different AV Blocks
AV blocks have different impacts on patients. 1st degree AV block is often harmless. But, 3rd degree AV block needs treatment because it can cause serious symptoms and risks.
It’s vital to spot these differences on an ECG to choose the right treatment. This can range from watching the condition for 1st degree AV block to needing a pacemaker for 3rd degree AV block.
Analyzing 3rd Degree Heart Block Rhythm Strips: Case Examples
Diagnosing 3rd degree heart block depends a lot on reading ECG rhythm strips right. These strips show the heart’s electrical activity. They are key to spotting third-degree heart block.
Classic Complete Heart Block Patterns
ECG rhythm strips show classic complete heart block patterns. These patterns have no link between P waves and QRS complexes. This is a key sign of 3rd degree heart block.
For example, a patient’s ECG might show an atrial rate that’s higher than the ventricular rate. There’s no clear link between the two.
Challenging and Atypical Presentations
Not every case of 3rd degree heart block looks the same on an ECG. Some cases have unusual features that need careful study to get right.
Take a patient with a junctional escape rhythm. This makes reading the ECG tricky. A detailed, step-by-step method is needed for a correct diagnosis.
Step-by-Step Analysis Approach
When we analyze ECG rhythm strips for 3rd degree heart block, we use a specific method:
- Identify P waves and QRS complexes
- Determine the atrial and ventricular rates
- Assess the relationship between P waves and QRS complexes
- Look for signs of AV dissociation
This method helps doctors accurately spot 3rd degree heart block. It also helps them tell it apart from other AV block types.
| ECG Feature | 3rd Degree Heart Block | Other AV Blocks |
| P wave and QRS relationship | No consistent relationship | Variable or consistent relationship |
| Atrial Rate | Usually higher than ventricular rate | May be normal or abnormal |
| Ventricular Rate | Typically slower than atrial rate | Variable |
Clinical Presentation and Emergency Management
Patients with 3rd degree heart block need quick medical help. This condition messes up the heart’s electrical system. It causes bradycardia and can be very dangerous.
Bradycardia and Poor Cardiac Output Symptoms
The main symptoms are bradycardia and low heart output. People might feel dizzy, fatigued, and short of breath. These signs show the heart can’t beat fast enough.
Immediate Interventions for Symptomatic Patients
Quick action is key for 3rd degree heart block. First, doctors might give atropine to try and speed up the heart. But, this might not work well.
Then, they might use temporary cardiac pacing. This can be done through the skin or with a temporary pacemaker.
Temporary and Permanent Cardiac Pacing Indications
Temporary pacing helps until a permanent pacemaker can be put in. The choice to go for a permanent pacemaker depends on the cause and the patient’s health.
For those with symptoms, a permanent pacemaker is often the best choice. It can greatly improve survival and quality of life.
It’s vital to act fast when 3rd degree heart block is found. This can prevent serious heart damage and help patients get better.
Conclusion: Mastering 3rd Degree Heart Block Diagnosis
Understanding 3rd degree heart block is key to helping patients. It’s all about knowing how to read ECGs and what symptoms to look for. We’ve talked about the main points of diagnosing this serious heart issue.
Doctors can spot third-degree AV block by looking at the ECG. They look for signs like the heart’s rhythm not matching. This helps them decide on the right treatment, like pacemakers.
Learning to read ECGs well is vital for top-notch healthcare. Knowing about 3rd degree heart block helps doctors give the best care. This is important for patients needing advanced treatments.
FAQ
What is 3rd degree heart block?
3rd degree heart block, also known as complete AV block, is a serious heart condition. It happens when electrical signals between the atria and ventricles are blocked. This leads to the heart beating on its own in two parts.
How is 3rd degree heart block diagnosed on an ECG?
Doctors use an ECG to spot 3rd degree heart block. They look for AV dissociation. This means P waves and QRS complexes don’t match up, with the atria beating faster than the ventricles.
What are the characteristic ECG findings of 3rd degree heart block?
The ECG shows AV dissociation and regular P waves that don’t match QRS complexes. The ventricles beat slower than the atria. This often leads to a ventricular escape rhythm.
What is the difference between 3rd degree heart block and other types of AV blocks?
3rd degree heart block is a complete block between the atria and ventricles. This is different from 1st and 2nd degree AV blocks. Those are partial or intermittent blocks.
How is 3rd degree heart block managed in emergency situations?
In emergencies, doctors use temporary pacing to stabilize the heart. This is followed by permanent pacing in many cases.
What are the clinical implications of 3rd degree heart block?
3rd degree heart block can cause bradycardia and poor cardiac output. It can be life-threatening if not treated quickly.
Can 3rd degree heart block be treated with medication alone?
No, medication alone can’t treat 3rd degree heart block. It usually needs cardiac pacing to manage effectively.
What is the role of cardiac pacing in managing 3rd degree heart block?
Cardiac pacing is key in managing 3rd degree heart block. It ensures a steady heart rate and improves output. This helps alleviate symptoms and prevent complications.
How does a junctional escape rhythm manifest on an ECG in 3rd degree heart block?
A junctional escape rhythm shows up as a narrow QRS complex rhythm. It has a rate between 35-50 BPM. This indicates the rhythm starts from the AV junction.
What are the hemodynamic consequences of a ventricular escape rhythm in 3rd degree heart block?
A ventricular escape rhythm can cause hemodynamic instability. The slow and irregular ventricular rate can lower cardiac output. This may lead to symptoms.
References:
- Mwalimu, J., & Cooper, A. (2024). Multiple variations in abdominal aorta branching with special reference to the presence of accessory renal arteries from an East African female cadaver. Surgical and Radiologic Anatomy, 46(8), 929-934. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11441833/