Last Updated on November 25, 2025 by Ugurkan Demir

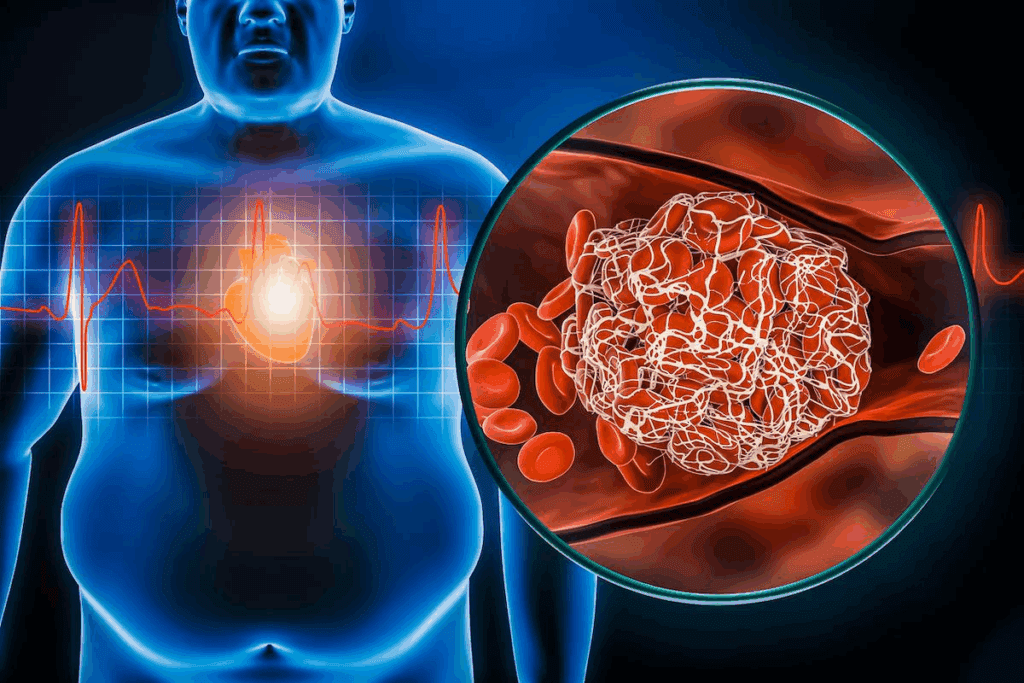
Cardiomyopathy is a heart muscle disease with different types, like hypertrophic, dilated, restrictive, and arrhythmogenic cardiomyopathy. To treat it well, we need to know exactly what’s wrong. This is done through echocardiography, cardiac MRI, and blood tests.
At Liv Hospital, we focus on top-notch care for cardiomyopathy. Our team creates personalized management plans for each patient. We aim to make the heart healthy again and avoid future problems.
Learn how to treat cardiomyopathy effectively through diagnosis, medication, and lifestyle care.
Key Takeaways
- Cardiomyopathy has many types, each needing its own treatment.
- Getting the right diagnosis is key and uses advanced tests.
- We work with patients to make plans that fit them best.
- Liv Hospital follows global standards and the latest treatment methods.
- Our goal is to improve heart health and stop future issues.
Understanding Cardiomyopathy: Definition and Types
Cardiomyopathy is a group of conditions that harm the heart muscle. This leads to poor heart function. It includes many diseases that affect the heart muscle, making it hard for the heart to pump blood well.
What is Cardiomyopathy?
Cardiomyopathy is a term for diseases that harm the heart muscle. These diseases can make the heart muscle enlarged, thickened, or stiff. This makes it harder for the heart to pump blood.
Understanding cardiomyopathy is key to managing and treating it. We will look at the different types and what they mean.
Major Types of Cardiomyopathy
Cardiomyopathy is divided into several main types. Each type affects the heart muscle differently. The main types are:
- Hypertrophic Cardiomyopathy: This is when the heart muscle thickens, making it hard to pump blood.
- Dilated Cardiomyopathy: The heart’s chambers get bigger, reducing its ability to pump blood.
- Restrictive Cardiomyopathy: The heart muscle stiffens, making it hard for the chambers to fill with blood.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): This is when fatty tissue replaces heart muscle, causing abnormal heart rhythms.
Acute vs. Chronic Cardiomyopathy
Cardiomyopathy can be either acute or chronic. Acute cardiomyopathy develops quickly and may need urgent care. It can be caused by sudden things like infections or toxins. On the other hand, chronic cardiomyopathy develops slowly over time. It can be caused by long-term conditions like high blood pressure or coronary artery disease.
Knowing if the cardiomyopathy is acute or chronic is important for treatment. We will discuss treatment options in the next sections.
Recognizing the Warning Signs and Symptoms

Spotting cardiomyopathy early is key. This heart muscle disease shows up in different ways. We’ll look at common and specific symptoms to know when to get help.
Common Symptoms Across All Types
Many cardiomyopathy types share some symptoms. These include:
- Shortness of breath (dyspnea): This can happen when you’re active or just sitting.
- Fatigue: Feeling very tired or weak, often because your heart can’t pump blood well.
- Swelling in the legs, ankles, and feet (edema): Fluid buildup happens when your heart can’t pump blood right.
- Palpitations or irregular heartbeats: You might feel your heart skipping beats or beating oddly.
Type-Specific Symptoms
Each cardiomyopathy type has its own symptoms. For example:
- Dilated cardiomyopathy often leads to heart failure symptoms like shortness of breath and fatigue.
- Hypertrophic cardiomyopathy may cause chest pain, dizziness, and fainting, mostly when you’re active.
- Restrictive cardiomyopathy can cause swelling and fatigue because your heart can’t fill with blood right.
When to Seek Medical Attention
Get medical help if you notice:
- Severe shortness of breath that stops you from doing daily things or happens when you’re sitting.
- Chest pain or discomfort that doesn’t go away or gets worse.
- Fainting or feeling like you’re going to faint.
- A rapid or irregular heartbeat that doesn’t go back to normal on its own.
Knowing these signs and when to get help is very important. If you’re feeling any of these symptoms, see a doctor right away. They can give you the right care and treatment.
Risk Factors and Prevention Strategies
Many things can raise your risk of getting cardiomyopathy. This includes your genes and lifestyle choices. Knowing these risks is key to stopping them early.
Genetic and Family History Considerations
Genes are a big deal in cardiomyopathy. If your family has it, you’re more likely to get it too. Genetic testing can find the genes that cause it.
Family history matters a lot. Some heart conditions are passed down. If your family has cardiomyopathy, talk to your doctor about it.
Lifestyle and Environmental Factors
What you do and where you live also affects your heart health. High blood pressure is a big risk because it makes your heart work harder.
Other lifestyle things include:
- Diet: Eating too much salt and fat can harm your heart.
- Physical activity: Exercise is good, but it must fit your health.
- Substance abuse: Too much alcohol or drugs can hurt your heart.
Preventive Measures for High-Risk Individuals
If you’re at high risk, there are steps you can take. Keeping your blood pressure in check is very important.
Here are some ways to prevent it:
| Preventive Measure | Description | Benefit |
| Regular Exercise | Tailored physical activity | Improves heart health |
| Dietary Changes | Low-salt, balanced diet | Reduces blood pressure |
| Stress Management | Techniques like meditation or yoga | Lowers stress levels |
By managing risk factors, you can prevent or delay cardiomyopathy. It’s important for high-risk people to work with their doctors.
The Diagnostic Process: Step-by-Step
Diagnosing cardiomyopathy involves several steps. These include looking at your medical history, doing a physical exam, and running tests. We’ll walk you through what happens when you see your doctor.
Initial Evaluation and Medical History
Your journey starts with a detailed medical history and initial check-up. We’ll ask about your symptoms, family health, and past illnesses. This info helps us figure out what might be causing your cardiomyopathy and what tests to run next.
Key components of the medical history include:
- Symptom assessment: duration, severity, and characteristics
- Family history of heart disease or cardiomyopathy
- Previous medical conditions, such as hypertension or diabetes
- Lifestyle factors, including diet, exercise, and smoking habits
Physical Examination Findings
A detailed physical exam is done to find signs of cardiomyopathy. We’ll listen for heart rhythm issues, murmurs, and signs of heart failure.
Common physical examination findings include:
- Abnormal heart sounds or murmurs
- Signs of fluid retention, such as edema
- Jugular venous distension
- Abnormal pulse or blood pressure readings
Essential Diagnostic Tests
Diagnostic tests are key to confirming the diagnosis and understanding the type and severity of cardiomyopathy. We’ll explain the main tests used in this process.
| Diagnostic Test | Purpose |
| Echocardiography | Assesses heart structure and function, including chamber size and valve function |
| Cardiac MRI | Provides detailed images of the heart, assessing structure and function |
| Blood Tests | Evaluates for signs of heart failure, infection, or other conditions that may be contributing to cardiomyopathy |
By using your medical history, physical exam, and test results, we can accurately diagnose cardiomyopathy. Then, we can create a treatment plan that fits your needs.
Understanding Your Diagnosis: What the Results Mean
Getting a diagnosis of cardiomyopathy can feel overwhelming. But, it’s key to understand what it means for managing your condition. We’ll help you make sense of your diagnosis.
Interpreting Heart Wall Changes
Tests can show changes in the heart wall, like thickening or thinning. Thickening, or hypertrophic cardiomyopathy, can make it hard for the heart to pump blood. Thin walls, seen in dilated cardiomyopathy, can also reduce pumping power. Knowing these changes helps us choose the right treatment.
Assessing Heart Function and Blood Flow
Diagnostic results also tell us about heart function and blood flow. Echocardiograms and MRI scans show how well the heart pumps and spot blood flow issues. This info is key for figuring out how severe your cardiomyopathy is and what treatment you need.
Risk Stratification: Determining Severity
Risk stratification helps us understand how severe your cardiomyopathy is and what risks you face. We look at heart wall changes, function, and blood flow. Knowing your risk level lets us create a plan that meets your needs and lowers the chance of problems.
By understanding your test results, we can make a detailed plan for managing your cardiomyopathy. This plan will help improve your life quality.
How to Treat Cardiomyopathy: Medication Approaches
Cardiomyopathy treatment often uses a mix of medicines to control symptoms and slow disease growth. We’ll look at the different ways to treat cardiomyopathy. This includes first-line treatments, specific protocols for each type, managing side effects, and checking how well the treatment works.
First-Line Medications
The first step in treating cardiomyopathy usually involves medicines that ease the heart’s workload and manage symptoms. ACE inhibitors and beta blockers are often the first choices. ACE inhibitors relax blood vessels, which lowers blood pressure and improves blood flow. Beta blockers, on the other hand, slow the heart rate and reduce the force of each beat, which lowers the heart’s need for oxygen.
For example, someone with cardiomyopathy might take lisinopril, an ACE inhibitor, to control high blood pressure. They might also take metoprolol, a beta blocker, to keep their heart rate in check. Diuretics can also be used to reduce fluid in the body, helping to ease symptoms like swelling and shortness of breath.
Type-Specific Medication Protocols
The type of cardiomyopathy affects the choice of medication. For instance, people with hypertrophic cardiomyopathy might take beta blockers or certain calcium channel blockers. These help reduce the heart’s contractility and ease symptoms like chest pain and shortness of breath.
On the other hand, those with dilated cardiomyopathy might need a different set of medications. This could include drugs to manage heart failure and prevent irregular heartbeats. Anti-arrhythmic medications are often used to control irregular heartbeats, which are common in certain types of cardiomyopathy.
Managing Medication Side Effects
Medicines are key in managing cardiomyopathy, but they can also have side effects. ACE inhibitors might cause coughing and dizziness, while beta blockers can lead to fatigue and cold hands or feet. It’s important for patients to work closely with their healthcare provider to manage these side effects.
Changing the dosage or switching to a different medication can often help reduce side effects. For example, if an ACE inhibitor causes a persistent cough, switching to an angiotensin II receptor blocker (ARB) might be considered. ARBs have a similar effect but different side effects.
Monitoring Medication Effectiveness
Regular check-ups with a healthcare provider are key to see if the medication is working. This might include blood tests, echocardiograms, and other tests to check heart function and overall health.
By keeping a close eye on how the patient responds to treatment, healthcare providers can make the necessary adjustments. This could mean changing the dosage, adding new medications, or stopping ones that aren’t working.
Lifestyle Modifications for Cardiomyopathy Management
Lifestyle changes are key in managing cardiomyopathy. They improve life quality and outlook. By changing diet, exercise, stress, and sleep habits, people with cardiomyopathy can manage their condition better.
Dietary Recommendations
Eating right is vital for heart health. Focus on:
- Low Sodium Intake: Reduces blood pressure and fluid buildup.
- Balanced Nutrient Intake: Get enough vitamins, minerals, and proteins.
- Avoiding Processed Foods: Stay away from foods high in saturated fats, sugars, and preservatives.
Talking to a healthcare provider or dietitian for a personalized meal plan is a good idea.
Exercise Guidelines and Limitations
Exercise is important but must be done carefully. We suggest:
- Low-Intensity Exercises: Walking, cycling, or swimming are good.
- Monitoring Progress: Check heart rate and blood pressure often.
- Avoiding High-Intensity Activities: Stay away from intense activities, if you have severe cardiomyopathy.
Always talk to a healthcare provider before starting new exercises.
Stress Management Techniques
Stress can make cardiomyopathy symptoms worse. Good stress management includes:
- Meditation and Deep Breathing: Helps reduce stress and relax.
- Yoga: Low-impact exercise that manages stress and improves flexibility.
- Counseling or Therapy: Professional help for stress and emotional challenges.
Find what works for you and make it part of your daily life. It can greatly improve your quality of life.
Sleep and Recovery Optimization
Good sleep and recovery are essential for heart health. We recommend:
- Establishing a Regular Sleep Schedule: Go to bed and wake up at the same time every day.
- Creating a Restful Environment: Make your bedroom dark, quiet, and cool.
- Avoiding Stimulants Before Bedtime: Don’t have caffeine or use electronic devices before bed.
By focusing on sleep and recovery, people with cardiomyopathy can help their hearts work better.
Advanced Treatment Options: Devices and Procedures
When cardiomyopathy gets worse, doctors might suggest advanced treatments. These include devices and surgeries. They aim to control symptoms, boost life quality, and extend life for those with severe cardiomyopathy.
Implantable Devices
Implantable devices are key in managing cardiomyopathy. They help monitor and control the heart’s function. This improves life quality and lowers the risk of serious problems.
Implantable Cardioverter-Defibrillators (ICDs) detect irregular heartbeats and shock the heart back to normal. They’re vital for those at high risk of sudden cardiac death.
Cardiac Resynchronization Therapy (CRT) devices help the heart’s chambers beat in sync. This boosts heart efficiency and eases heart failure symptoms.
Ventricular Assist Devices (VADs) are mechanical pumps that support the heart. They enhance blood flow and lessen heart workload. VADs can be a temporary fix or a long-term solution for those not eligible for a transplant.
Surgical Interventions
Surgery is sometimes needed for cardiomyopathy. These procedures can fix or remove damaged heart tissue. They also improve blood flow and reduce symptoms.
A septal myectomy is a common surgery. It removes part of the heart muscle to enhance blood flow and lessen symptoms in hypertrophic cardiomyopathy patients.
In some cases, heart surgery is needed to fix or replace damaged heart valves. Or to perform a coronary artery bypass grafting to improve blood flow to the heart muscle.
Heart Transplantation Considerations
For those with advanced cardiomyopathy, heart transplantation might be an option. It involves replacing the diseased heart with a healthy one from a donor.
The choice to get a heart transplant is made after trying other treatments. Patients must go through a detailed evaluation to see if they’re a good match for a transplant.
Heart transplantation can save lives but requires careful thought and ongoing care. It’s important to prevent rejection and ensure the transplanted heart stays healthy for the long term.
Conclusion
We’ve looked into cardiomyopathy, a heart muscle issue that causes many problems. Managing it well means getting the right diagnosis, taking the right meds, making lifestyle changes, and sometimes using advanced treatments.
Knowing the types of cardiomyopathy and their signs is key. This way, people can get help fast. A treatment plan that fits each person is vital. It might include medicine, lifestyle changes, or even surgery to keep the heart healthy.
Our talk shows how important a detailed plan is for managing cardiomyopathy. With the right approach, people can live full and active lives. By following these steps, patients can handle their condition better, feel less symptoms, and enjoy a better life.
FAQ
What is cardiomyopathy?
Cardiomyopathy is a disease that affects the heart muscle. It makes the heart work less well. There are different types, like hypertrophic and dilated cardiomyopathy.
What are the major types of cardiomyopathy?
The main types are hypertrophic, dilated, restrictive, and arrhythmogenic cardiomyopathy. Knowing these helps in treating the disease effectively.
What are the common symptoms of cardiomyopathy?
Symptoms vary by type but often include shortness of breath and fatigue. Swelling in the legs is also common.
How is cardiomyopathy diagnosed?
Diagnosing cardiomyopathy involves several steps. First, a doctor will review your medical history. Then, they’ll do a physical exam and run tests like echocardiography and cardiac MRI.
What is the role of genetic predisposition in cardiomyopathy?
Genetics and family history are key in cardiomyopathy. If your family has it, you’re at higher risk. It’s important to take preventive steps.
How can high-risk individuals prevent cardiomyopathy?
High-risk people can prevent it by managing their blood pressure. This can lower their risk of getting cardiomyopathy.
What lifestyle modifications can help manage cardiomyopathy?
Making lifestyle changes can help. This includes eating right, exercising, managing stress, and getting enough sleep. These changes can improve life quality for those with cardiomyopathy.
What are the advanced treatment options for cardiomyopathy?
Advanced treatments include ICDs, CRT, surgery, and heart transplants. These options are for those who need more than usual care.
How does blood pressure affect cardiomyopathy?
Keeping blood pressure in check is vital for those with cardiomyopathy. High blood pressure can make the condition worse.
What is the significance of thinning or thickening of the heart wall in cardiomyopathy?
Changes in the heart wall, like thinning or thickening, can signal cardiomyopathy. Understanding these changes is key to managing the disease.
What is myocardiopathy?
Myocardiopathy is another name for cardiomyopathy. It refers to diseases affecting the heart muscle.
Can cardiomyopathy be treated with medication?
Yes, medication can treat cardiomyopathy. It’s important to use the right medications and manage side effects for effective treatment.
What is the role of implantable devices in treating cardiomyopathy?
Devices like ICDs and CRT help manage cardiomyopathy. They regulate heart rhythm and improve function.
References
- Camasão, D. B., & Mantovani, D. (2021). The mechanical characterization of blood vessels and their substitutes in the continuous quest for physiologically relevant performances: A critical review. Mechanics Research Communications, 114, 103655. https://www.sciencedirect.com/science/article/pii/S2590006421000144