Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we know how vital it is to correctly diagnose 3rd degree AV block, or complete heart block. This serious condition means the heart’s electrical signals don’t reach the ventricles. It’s a life-threatening issue that needs quick action.
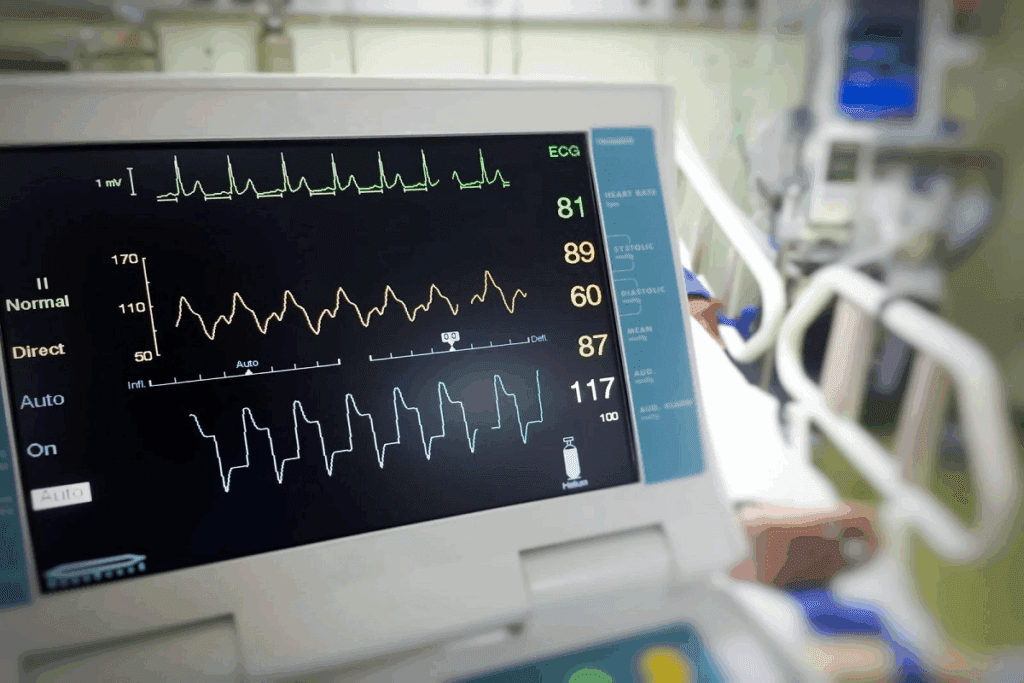
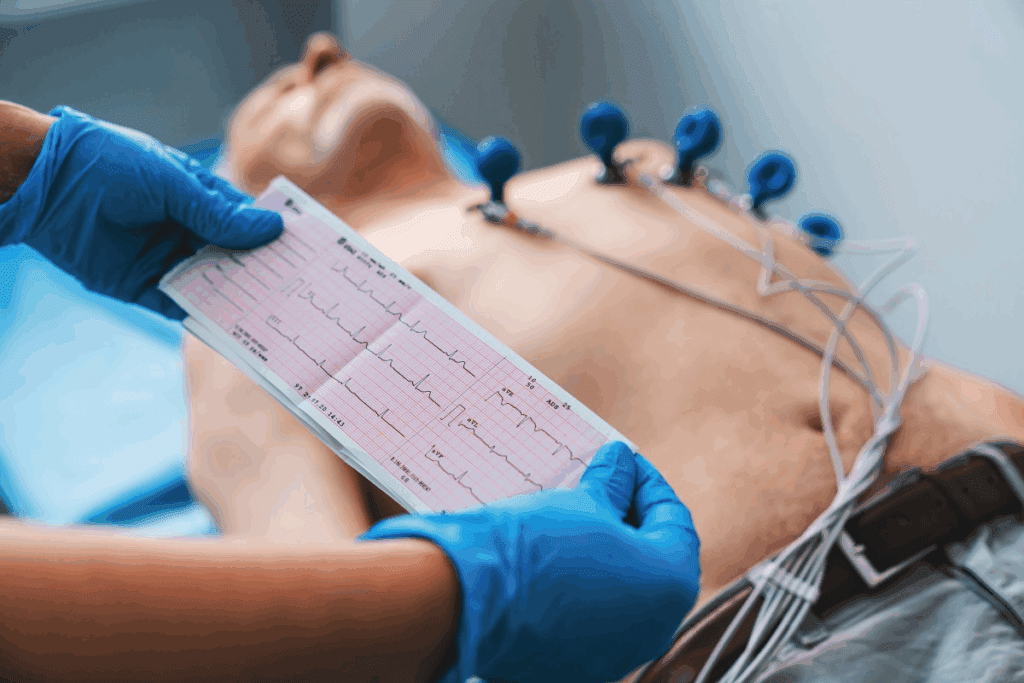
The electrocardiogram (ECG) is key in spotting this problem. It shows when there’s no link between P waves and QRS complexes. Knowing these ECG signs is critical for doctors to give the right care fast. We’ll look at the 7 main ECG signs for diagnosing and treating 3rd degree heart block.
Key Takeaways
- Understanding the definition and significance of 3rd degree AV block.
- Recognizing the role of ECG in diagnosing complete heart block.
- Identifying the key ECG findings associated with this condition.
- The importance of timely and appropriate care for patients with 3rd degree heart block.
- Liv Hospital’s approach to managing complete heart block with expert care.
What Is 3rd AV Block? Definition and Pathophysiology

To understand third-degree AV block, we need to look at its definition and how it works. This condition stops the electrical signals from moving from the atria to the ventricles. This means the atria and ventricles beat on their own, a situation called AV dissociation.
The block can happen at different parts of the heart’s electrical system. It can block signals at the AV node, the His bundle, or the bundle branches.
Complete Electrical Dissociation Between Atria and Ventricles
In third-degree AV block, the SA node’s electrical signals can’t reach the ventricles. So, the atria and ventricles beat at their own rates. This makes the heart’s contractions not in sync.
Key characteristics of AV dissociation include:
- Independent P waves and QRS complexes on the ECG
- Atrial rate typically faster than the ventricular rate
- Variable relationship between P waves and QRS complexes
Anatomical Locations of Block
The block in third-degree AV block can happen in different places. It can block signals at the AV node, the His bundle, or the bundle branches. Where the block is affects the heart’s rhythm.
| Location of Block | Typical Escape Rhythm | Characteristics |
| AV Node | Junctional Escape | Narrow QRS, rate 40-60 bpm |
| His Bundle or Bundle Branches | Ventricular Escape | Wide QRS, rate 20-40 bpm |
Underlying Mechanisms of AV Dissociation
AV dissociation in third-degree AV block comes from damage to the heart’s electrical system. This damage can be from many causes. It can be from heart disease, ischemia, or from certain medicines.
Knowing how AV dissociation works is key to treating third-degree AV block. The ECG is very important for diagnosing and planning treatment.
Common Causes and Risk Factors
Third-degree AV block can come from many causes and risk factors. Knowing these is key to diagnosing and treating it well.
Degenerative Conduction System Disease
Degenerative changes in the heart’s conduction system are a big reason for third-degree AV block, mainly in older people. As we get older, the heart’s conduction system can get scarred and hardened. This process is linked to aging and can get worse with heart disease.
Ischemic Heart Disease
Ischemic heart disease is another big cause of third-degree AV block. Heart attacks can harm the conduction system, causing complete AV block. Heart attacks can cause inflammation and damage that messes up normal heart rhythm.
Medication-Induced AV Block
Some medicines can cause third-degree AV block by affecting the heart’s rhythm. Drugs like beta-blockers, calcium channel blockers, and anti-arrhythmics can slow down the heart’s rhythm. It’s important to watch closely when giving these medicines, mainly to those with heart rhythm problems.
Other Etiologies
Other, less common reasons for third-degree AV block include diseases like amyloidosis, inflammation of the heart, and heart problems from birth.
“Infiltrative diseases can disrupt the normal functioning of the heart’s conduction system, leading to severe conduction abnormalities.”
These conditions show how varied the causes of complete heart block are. They stress the importance of a thorough check-up.
Key ECG Finding #1: Complete AV Dissociation
In third-degree AV block, the ECG shows complete AV dissociation. This means there’s a total block in the normal heart rhythm pathway. The atria and ventricles beat independently, affecting the heart’s function.
Independent P Waves and QRS Complexes
Complete AV dissociation is marked by independent P waves and QRS complexes on an ECG. P waves, showing atrial activity, beat faster than the ventricular rate shown by QRS complexes. This means atrial and ventricular contractions are not synchronized, disrupting normal heart rhythm.
On an ECG strip, you’ll see P waves not followed by QRS complexes. QRS complexes beat at a rate not tied to P waves. This lack of association is key to diagnosing this condition.
Recognizing the Pattern on ECG Strips
To spot complete AV dissociation on ECG strips, observe closely. Look for P waves not linked to QRS complexes and a ventricular rate slower than the atrial rate. P waves may appear to move through QRS complexes without a clear link.
Here’s a table to help recognize these features:
| Feature | Description |
| P Waves | Independent of QRS complexes, typically at a faster rate |
| QRS Complexes | Occur at a slower rate, not associated with P waves |
| AV Association | No consistent relationship between P waves and QRS complexes |
Distinguishing from Incomplete AV Blocks
It’s important to tell complete AV dissociation apart from incomplete AV blocks. Incomplete blocks, like first-degree or second-degree, show some link between P waves and QRS complexes. Third-degree AV block, on the other hand, shows complete dissociation.
Knowing the differences helps us care for patients better. Spotting complete AV dissociation on an ECG lets us diagnose third-degree AV block correctly and start the right treatment.
Key ECG Finding #2: Regular P Waves with Independent QRS Rhythm
Regular P waves with an independent QRS rhythm are a hallmark of third-degree AV block on ECG. This pattern is key for diagnosing complete heart block.
Atrial Rate vs. Ventricular Rate Discrepancy
In third-degree AV block, the atrial rate is faster than the ventricular rate. The P waves, driven by the sinoatrial node, occur at a consistent rate. But the QRS complexes happen at a slower, independent rate.
This difference between atrial and ventricular rates is a key diagnostic feature. We look for this discrepancy when interpreting ECGs.
The atrial rate is usually normal or slightly increased. This shows the body’s attempt to compensate for reduced cardiac output. The ventricular rate, on the other hand, is significantly slower, often between 40-60 bpm, depending on the escape pacemaker site.
P Wave Morphology and Consistency
Analyzing the P wave morphology and consistency is essential. In third-degree AV block, P waves are typically consistent in morphology. This indicates a single source of atrial activation, usually the sinoatrial node.
We look for P waves that are consistent in shape, amplitude, and direction. This suggests a normal sinus rhythm or other consistent atrial rhythm. Any variation in P wave morphology may indicate an ectopic atrial rhythm or other pathology.
Pattern Recognition Techniques
Pattern recognition is a critical skill for diagnosing third-degree AV block on ECG. We use several techniques to identify the characteristic pattern of regular P waves with an independent QRS rhythm.
One effective method is to carefully examine long rhythm strips. We look for the consistent P-P interval and the independent QRS complexes. Another approach is to use calipers or digital calipers on an ECG machine to measure the P-P and R-R intervals, confirming their regularity and independence.
“The key to diagnosing third-degree AV block lies in recognizing the dissociation between atrial and ventricular activity on the ECG.” – Medical Expert
By combining these pattern recognition techniques with a thorough understanding of the ECG findings, we can accurately diagnose third-degree AV block and provide appropriate management.
Key ECG Finding #3: Escape Rhythm Characteristics
Diagnosing third-degree AV block requires understanding the escape rhythm. This rhythm is key for ventricular contraction when the normal pathway is blocked.
The escape rhythm can start from the AV junction or the ventricles. Knowing these features is vital for correct diagnosis and treatment.
Junctional Escape Rhythm Features (40-60 bpm)
A junctional escape rhythm has a rate of 40-60 bpm. It has a narrow QRS complex. This narrow QRS means the rhythm starts from the AV junction.
This rhythm is usually more stable and faster. It helps keep a steady ventricular rate in complete heart block.
Ventricular Escape Rhythm Features (20-40 bpm)
A ventricular escape rhythm is slower, with a rate of 20-40 bpm. It has a wide QRS complex. This wide QRS shows it starts from within the ventricles.
Ventricular rhythms are often less stable. They may lead to asystole or severe bradycardia.
Stability of Escape Rhythms
The stability of the escape rhythm is key for a good heart rate and stability. The rhythm’s stability depends on its origin, heart disease, and other conditions.
It’s important to watch the rhythm’s characteristics and stability on ECG. This helps manage patients with third-degree AV block and decide if pacing is needed.
Key ECG Finding #4: QRS Complex Morphology Variations
In third-degree AV block, the QRS complex can change a lot. This change shows where the heart’s rhythm starts. Doctors need to know this to understand the block’s level and how the heart is trying to compensate.
Narrow QRS in Junctional Escape
A narrow QRS, under 120 ms, means the rhythm starts at the AV junction. This is because the electrical signal goes through the ventricles normally. This leads to a synchronized heartbeat.
Junctional escape rhythms beat between 40-60 times per minute. They have a narrow QRS unless there’s a problem with how the signal is sent.
Wide QRS in Ventricular Escape
A wide QRS, over 120 ms, means the rhythm starts in the ventricles. This happens when the ventricles start the heartbeat. The heart rate is slower, usually 20-40 beats per minute.
Ventricular escape rhythms have a wide QRS. This is because the electrical signal spreads slowly through the ventricular muscle, not following the usual path.
Implications of QRS Width for Diagnosis
The QRS complex’s width is key for diagnosis. A narrow QRS usually means the rhythm starts at the AV junction. This suggests the block is at or above the AV node. A wide QRS means the rhythm starts in the ventricles, indicating a block further down.
Knowing where the rhythm starts is vital for treating third-degree AV block. It helps doctors choose the right treatment for patients.
Key ECG Finding #5: Bradycardia and Hemodynamic Consequences
Bradycardia, or a slow heart rate, is a key finding in complete heart block. It can lead to serious problems with blood flow. This happens because the heart’s electrical signals are not working together right.
Typical Heart Rate Ranges in Complete Heart Block
In complete heart block, the heart beats much slower than usual. The rate can be between 20-60 beats per minute. Junctional escape rhythms are faster, at 40-60 bpm. Ventricular escape rhythms are slower, at 20-40 bpm.
| Escape Rhythm Origin | Typical Heart Rate Range (bpm) |
| Junctional | 40-60 |
| Ventricular | 20-40 |
Clinical Signs of Hemodynamic Compromise
Bradycardia in complete heart block can cause dizziness, fainting, and low blood flow. These symptoms happen because the heart rate is too slow. It can’t keep up with the body’s needs, making things worse during stress or activity.
“The presence of bradycardia in third-degree AV block can lead to inadequate perfusion of vital organs, resulting in symptoms such as fatigue, shortness of breath, and even loss of consciousness.”
ECG Indicators of Unstable Bradycardia
On an ECG, signs of unstable bradycardia include a very slow heart rate and wide QRS complexes. These show the heart is not working well. They also suggest the heart might get worse.
It’s very important to spot these ECG signs. They help doctors act fast to avoid bad outcomes in patients with complete heart block.
Key ECG Finding #6: Rhythm Strip Analysis Techniques
When looking at ECG strips for third-degree AV block, a careful method is key. We need to closely check the P waves, QRS complexes, and how they relate to each other.
Systematic Approach to 3rd Degree Block ECG Strips
To analyze ECG strips well, we should follow a clear process:
- Measure the P-P and R-R intervals to spot any gap between atrial and ventricular rhythms.
- Study the shape of P waves and QRS complexes to figure out where they come from and if they stay the same.
- Look for signs of AV dissociation, like P waves and QRS complexes that move on their own.
Ladder Diagram Method for Confirmation
The ladder diagram method helps confirm third-degree AV block. It makes the ECG strip easier to understand by showing the link between P waves and QRS complexes.
Common Pitfalls in Interpretation
When we interpret ECG strips, we should watch out for common mistakes, such as:
| Pitfall | Description |
| Misdiagnosing second-degree AV block | Missing the fact that there’s no AV conduction |
| Failing to recognize AV dissociation | Not spotting P waves and QRS complexes that act alone |
Knowing these common mistakes and using a systematic way can help us get better at reading ECGs.
Key ECG Finding #7: Differential Diagnosis on ECG
To accurately diagnose third-degree AV block, we must consider several key differential diagnoses on ECG. This involves distinguishing third-degree AV block from other conditions that may present with similar ECG findings.
Differential diagnosis is key because the management and prognosis of third-degree AV block differ from other conditions. Second-degree AV blocks, like high-grade second-degree AV block, can be hard to tell apart from third-degree AV block. It’s important to analyze the P wave and QRS complex morphology and their relationship.
Distinguishing from 2nd Degree AV Blocks
When distinguishing third-degree AV block from second-degree AV blocks, it’s essential to examine the ECG strip closely. In second-degree AV block, some P waves are conducted to the ventricles. In third-degree AV block, there is complete dissociation between atrial and ventricular activity.
| Characteristic | 2nd Degree AV Block | 3rd Degree AV Block |
| P Wave Conduction | Some P waves conducted | No P waves conducted |
| AV Association | Some association | Complete dissociation |
| QRS Complex | May be normal or wide | May be normal or wide, depending on escape rhythm |
Non-conducted PACs vs. Complete Heart Block
Non-conducted premature atrial contractions (PACs) can sometimes be mistaken for third-degree AV block. But, in non-conducted PACs, the P wave before the blocked P wave is premature and often has a different morphology than the sinus P waves.
“The presence of non-conducted PACs can mimic third-degree AV block, but careful examination of P wave morphology and timing can help differentiate between the two conditions.”
— ECG Interpretation Guide
AV Dissociation Due to Other Mechanisms
AV dissociation can occur due to mechanisms other than third-degree AV block, such as accelerated junctional or ventricular rhythms. In these cases, the atrial rate is typically slower than the ventricular rate, and there is no clear evidence of AV block.
Understanding these differential diagnoses is critical for accurate ECG interpretation and appropriate patient management. By carefully analyzing the ECG findings and considering the clinical context, we can make a precise diagnosis and develop an effective treatment plan.
Emergency Management of 3rd Degree Heart Block
Dealing with third-degree AV block quickly is key to avoiding big problems. People with this issue need fast help to keep their heart rate steady and blood flowing well.
Immediate Interventions for Symptomatic Patients
For those showing symptoms, quick action is needed. If someone feels dizzy, faints, or their heart isn’t pumping well, they need help right away. Temporary pacing is often used to keep the heart rate stable. This can be done through skin or vein methods.
Temporary Pacing Indications and Methods
Temporary pacing is for those with symptoms of third-degree AV block. The choice between skin or vein pacing depends on the patient’s health and the doctor’s skills. Skin pacing is faster but vein pacing gives a more stable rhythm.
Permanent Pacemaker Considerations
In some cases, a permanent pacemaker is needed for long-term care. The choice to get a pacemaker depends on why the block happened, the patient’s health, and if they have other heart issues.
Handling third-degree AV block well means acting fast. This includes temporary pacing and, if needed, a permanent pacemaker. Knowing how to manage this condition helps doctors save lives.
Conclusion: Importance of Prompt Recognition and Action
Recognizing and managing third-degree AV block quickly is key to avoid serious problems. These include cardiac arrest and death. We’ve listed 7 important ECG signs for diagnosing and treating this condition.
Doctors need to know these ECG signs and the need for quick action. This is because acting fast can greatly improve patient care. The role of quick recognition is huge in managing third-degree AV block effectively.
By knowing the ECG signs of third-degree AV block and acting fast, we can lower the risk of bad outcomes. This improves the care quality for those with this condition. It’s all about spotting the signs and acting quickly.
FAQ
What is third-degree AV block?
Third-degree AV block, also known as complete heart block, is a serious heart condition. It happens when there’s a complete break in the electrical signals between the atria and ventricles. This means the atria and ventricles beat on their own, not together.
What are the common causes of third-degree AV block?
This condition can be caused by several things. It often comes from a degenerative disease of the heart’s electrical system. It can also be caused by heart disease, certain medicines, or conditions like amyloidosis and myocarditis.
How is third-degree AV block diagnosed on an ECG?
Doctors diagnose it by looking at an ECG. They see that the P waves and QRS complexes don’t match up. Instead, they beat at their own rates.
What is the difference between a junctional escape rhythm and a ventricular escape rhythm in third-degree AV block?
Junctional escape rhythms have a faster rate, between 40-60 beats per minute. They have a narrow QRS complex. Ventricular escape rhythms are slower, between 20-40 beats per minute. They have a wide QRS complex.
How do you distinguish third-degree AV block from second-degree AV block on an ECG?
Third-degree AV block shows complete AV dissociation. This means the P waves and QRS complexes don’t work together. Second-degree AV block, on the other hand, shows some connection between them.
What are the hemodynamic consequences of third-degree AV block?
This condition can lead to a very slow heart rate. This can cause dizziness, fainting, and a drop in blood flow. It’s because the heart beats too slowly.
How is third-degree AV block managed in emergency situations?
In emergencies, doctors use temporary pacing. This can be done through the skin or through a vein. It helps keep the heart rate stable and improves blood flow.
What is the role of pacemaker implantation in managing third-degree AV block?
Sometimes, a pacemaker is needed to manage the condition long-term. It helps prevent serious problems.
Can third-degree AV block be caused by medications?
Yes, some medicines can cause AV block. This includes beta-blockers, calcium channel blockers, and certain anti-arrhythmic drugs.
What are the ECG indicators of unstable bradycardia in third-degree AV block?
Signs include a very slow heart rate and wide QRS complexes. There may also be signs of heart damage or ischemia.
References:
- Lung, K., & Lui, F. (2023). Anatomy, Abdomen and Pelvis: Arteries. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK525959/