Last Updated on November 25, 2025 by Ugurkan Demir
ECG third degree av block atrioventricular (AV) block, also known as complete heart block, is a serious heart condition. It stops electrical signals from the atria from reaching the ventricles. This makes the atria and ventricles beat on their own, a condition called AV dissociation.
This condition is very serious and needs immediate medical help. At Liv Hospital, we focus on top-notch heart care. Knowing the ECG signs of third-degree AV block is key for diagnosing and treating it.
Key Takeaways
- Third-degree AV block is a life-threatening condition requiring prompt medical attention.
- It is characterized by the complete failure of conduction from the atria to the ventricles.
- AV dissociation results in independent atrial and ventricular activity.
- Recognizing ECG characteristics is critical for diagnosis and treatment.
- Liv Hospital is dedicated to modern heart care and patient-focused excellence.
Understanding Third Degree AV Block
Third-degree AV block, also known as complete heart block, is a serious heart condition. It needs immediate medical help. This condition causes AV dissociation, where the heart’s upper and lower chambers beat at different rates. This can lead to severe problems.
Definition and Pathophysiology
Third-degree AV block stops the electrical signals from moving between the heart’s upper and lower chambers. This means the chambers work on their own, leading to AV dissociation. The upper chambers beat normally, but the lower chambers beat slower, usually between 40-60 times per minute.
The heart’s electrical system is interrupted in third-degree AV block. This can happen for many reasons. These include heart damage, heart attacks, infections, and some medicines.
Causes and Risk Factors
Many things can cause third-degree AV block. These include heart damage, heart attacks, infections, and some medicines. We will look at the main causes and risk factors.
- Degenerative changes in the heart’s electrical system
- Ischemic events, such as myocardial infarction
- Infections, such as myocarditis or endocarditis
- Certain pharmacological agents, such as anti-arrhythmic medications
Knowing the causes and risk factors is key to treating third-degree AV block. Healthcare professionals can then give better care and help improve patient outcomes.
ECG Third Degree AV Block: Basic Principles
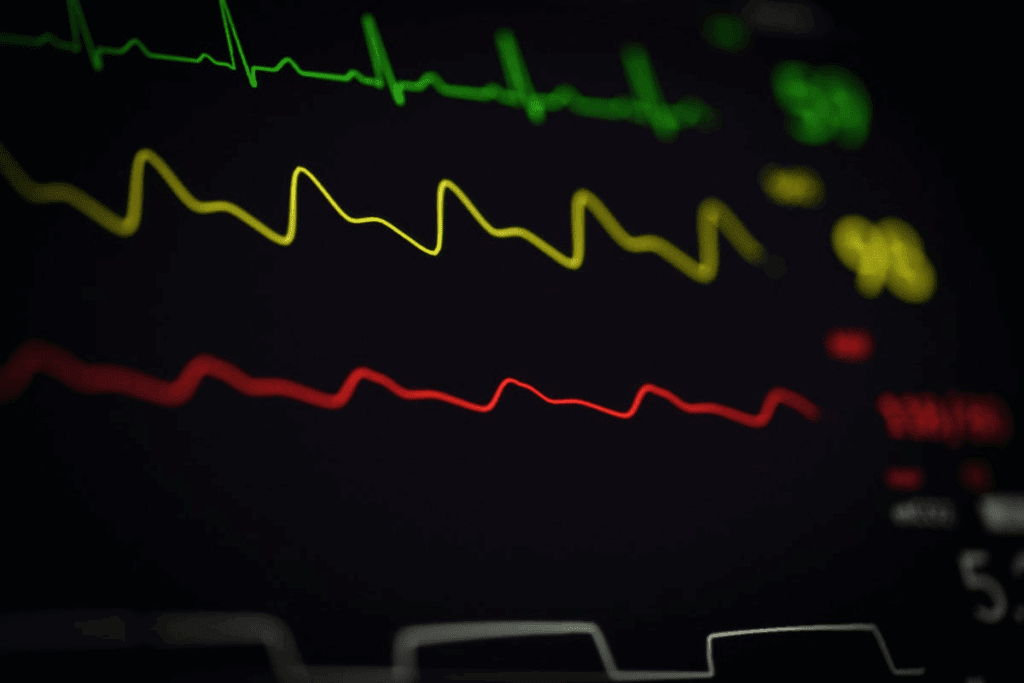
To diagnose third-degree AV block on an ECG, look for specific patterns. These patterns show that the atria and ventricles beat on their own.
Complete AV Dissociation
Complete AV dissociation is key to third-degree AV block. On an ECG, you’ll see:
- Regular P waves
- Regular QRS complexes
- No consistent relationship between P waves and QRS complexes
This means the electrical signals from the atria don’t reach the ventricles. This is because of a block in the AV node or further down.
Independent Atrial and Ventricular Activity
In third-degree AV block, the atria and ventricles beat on their own. The atria are controlled by the SA node, leading to a normal P wave rate of 60-100 bpm.
The ventricles, though, are controlled by an escape pacemaker. This can be in the AV junction or the ventricles themselves. The ventricular rate is slower, usually 40-60 bpm if the pacemaker is junctional.
This independent activity is what makes third-degree AV block different from other heart blocks.
Knowing these basics is key to diagnosing and managing third-degree AV block. By spotting the ECG patterns of complete AV dissociation and independent atrial and ventricular activity, doctors can give the right care to patients with this condition.
Key Finding #1: AV Dissociation
AV dissociation is a key sign of third-degree AV block. It shows the atria and ventricles beat on their own. This means there’s a total break in the usual flow of electrical signals between them.
Identifying P Waves and QRS Complexes
To spot AV dissociation on an ECG, we need to find the P waves and QRS complexes. P waves show when the atria depolarize. QRS complexes show when the ventricles depolarize. In third-degree AV block, these happen separately.
Looking closely at the ECG is key to spotting P waves. They might be hidden by QRS complexes or T waves. It’s also important to find QRS complexes and see if they’re conducted or escape beats.
Absence of Consistent PR Intervals
A key sign of AV dissociation is the lack of steady PR intervals. The PR interval is the time from the start of atrial depolarization (P wave) to the start of ventricular depolarization (QRS complex). In third-degree AV block, the PR intervals change randomly because the atria and ventricles don’t work together.
Usually, the atrial rate is higher than the ventricular rate. The PR intervals change without a pattern. This change is a main way to tell third-degree AV block apart from other heart block types.
Key Finding #2: Regular P Waves with Independent QRS Complexes
Third-degree AV block is marked by regular P waves and independent QRS complexes on an ECG. This pattern shows that the atria and ventricles beat on their own. This is called AV dissociation.
To grasp the meaning of this, we must look at how the atria and ventricles rate compare. We also need to know how to tell third-degree AV block apart from other AV block types.
Atrial Rate vs. Ventricular Rate
In third-degree AV block, the atria beat faster than the ventricles. The atrial rate is usually normal (60-100 bpm). But, the ventricular rate is slower, often between 40-60 bpm. This is due to a junctional escape rhythm.
If a ventricular escape rhythm takes over, the ventricular rate can drop to 20-40 bpm.
Table 1: Comparison of Atrial and Ventricular Rates in Third-Degree AV Block
| Parameter | Typical Rate (bpm) |
| Atrial Rate | 60-100 |
| Ventricular Rate (Junctional Escape) | 40-60 |
| Ventricular Rate (Ventricular Escape) | 20-40 |
Differentiating from Other Types of AV Block
To tell third-degree AV block apart from other AV block types, we look at the ECG. In third-degree AV block, P waves and QRS complexes are not linked. This is known as complete AV dissociation.
First-degree AV block has a long PR interval. Second-degree AV block shows some dropped beats. But third-degree AV block has no link between P waves and QRS complexes.
By studying the ECG for regular P waves and independent QRS complexes, we can spot third-degree AV block. We also understand the atrial and ventricular rates. This helps us tell it apart from other AV conduction issues.
Key Finding #3: Junctional Escape Rhythm Characteristics
Third-degree AV block shows several key ECG signs, like a junctional escape rhythm. This rhythm helps when the normal AV pathway is blocked.
Narrow QRS Complexes
Junctional escape rhythms have narrow QRS complexes, usually under 120 ms. This is because the rhythm starts near the AV node. It leads to a more normal way of activating the ventricles.
Rate Range of 40-60 BPM
The rate of a junctional escape rhythm is between 40-60 beats per minute (bpm). This rate is faster than ventricular escape rhythms. It helps keep the heart output good in third-degree AV block.
Hemodynamic Stability
Junctional escape rhythms in third-degree AV block are more stable. The faster rate and better ventricular contraction help keep blood pressure stable. This ensures vital organs get enough blood.
The key traits of junctional escape rhythms are:
- Narrow QRS complexes from the AV node origin
- Rate of 40-60 bpm for stable heart output
- More stable blood flow and organ perfusion
Knowing these traits is key for diagnosing and treating third-degree AV block. A junctional escape rhythm shows the heart’s effort to compensate for the block. Its features help decide on treatment.
Key Finding #4: Ventricular Escape Rhythm Patterns
Ventricular escape rhythms on an ECG are key in patients with complete heart block. They start in the ventricles and have wide QRS complexes. This makes them slower than junctional rhythms.
Wide QRS Complexes
Ventricular escape rhythms show wide QRS complexes, over 120 ms. This is because of how the ventricles activate. Junctional rhythms, on the other hand, have narrow QRS complexes unless there’s a delay.
Slower Rate (20-40 BPM)
The rate of ventricular escape rhythms is slower, between 20 to 40 beats per minute. This is because the ventricles’ natural rhythm is less efficient than the SA node or junctional tissue.
Hemodynamic Implications
The effects of ventricular escape rhythms on the heart are significant. Their slower rate and abnormal activation can lower cardiac output. This might cause dizziness, fatigue, or even fainting. It’s important to understand these effects to manage third-degree AV block patients well.
To better understand ventricular escape rhythms, let’s look at this table:
| Characteristic | Description | Clinical Implication |
| QRS Complex Width | Wide QRS complexes (>120 ms) | Abnormal ventricular activation |
| Rate | 20-40 bpm | Decreased cardiac output |
| Hemodynamic Impact | Reduced cardiac efficiency | Potential for dizziness, fatigue, or syncope |
When dealing with third-degree AV block, these points are vital. They affect the patient’s heart function and overall health.
Key Finding #5: Variable PR Intervals Without Pattern
Complete heart block is marked by PR intervals that change a lot and don’t follow a pattern. In third-degree AV block, the heart’s upper and lower chambers don’t work together well. This makes the PR intervals very unpredictable.
Looking at an ECG for third-degree AV block, measuring PR intervals is key. We see big changes in the time between P waves and QRS complexes. This shows a big problem with how the heart’s signals are sent.
Measuring PR Intervals in Complete Heart Block
To measure PR intervals, we look at when P waves start and QRS complexes begin. In complete heart block, these times are all over the place. This is because the heart’s upper and lower parts don’t work together.
Here’s how we do it:
- Find the P waves and QRS complexes
- Measure the time from P wave start to QRS complex start
- Look at many PR intervals to see if they’re all different
Clinical Significance of PR Variability
PR intervals that change a lot mean a lot to doctors. It shows the heart’s normal signal path is broken. This is important for figuring out third-degree AV block and knowing it’s not something else.
The big deal is:
- Figuring out third-degree AV block
- Telling it apart from other heart block issues
- Helping decide how to treat it
Spotting PR intervals that change a lot helps us diagnose third-degree AV block right. Then, we can start the right treatment, like getting a pacemaker to help the heart beat in sync.
Key Finding #6: Bradycardia in Third Degree Heart Block
Third-degree AV block often leads to bradycardia, a slow heart rate. This slow rate can affect the heart’s output and the patient’s health.
Typical Heart Rate Ranges
The heart rate in third-degree AV block is usually slow, often under 60 beats per minute (bpm). Sometimes, the rate can be even lower. For example, a junctional escape rhythm might keep the rate between 40-60 bpm. A ventricular escape rhythm can be slower, between 20-40 bpm.
Hemodynamic Consequences
Bradycardia from third-degree AV block can lower cardiac output. This might cause symptoms like dizziness, fatigue, and shortness of breath. In severe cases, it can lead to hypotension and poor blood flow to vital organs. “The slow heart rate can significantly impact the patient’s hemodynamic status, necessitating prompt clinical evaluation and management.”
As clinicians, we must watch and manage bradycardia in patients with third-degree AV block. A clinical study’s quote highlights that
“Effective management of bradycardia is key to avoiding bad outcomes in patients with third-degree AV block.”
This shows the importance of quick action to keep the heart output right and avoid problems.
Key Finding #7: Identifying Capture or Escape Beats
The seventh key finding in diagnosing third-degree AV block is about capture and escape beats on the ECG. It’s key to know the difference. This helps us understand the rhythm and its clinical importance.
Differentiating Escape Mechanisms
Capture beats go from the atria to the ventricles. Escape beats start in the ventricles or AV junction. It’s important to tell these beats apart to grasp the arrhythmia’s cause.
- Capture beats show the atrial impulse reaches the ventricles.
- Escape beats are ventricular or junctional beats when the main pacemaker fails.
Clinical Significance
Knowing capture or escape beats is vital for understanding third-degree AV block. Seeing these beats helps us see how stable the heart is. It also helps us decide the best treatment.
- Capture beats suggest some AV conduction is happening.
- Escape beats mean the heart depends on secondary pacemakers. This affects pacing therapy.
By studying the ECG for capture and escape beats, doctors can better understand the patient. They can then create a good treatment plan.
Clinical Manifestations and Management
Third-degree AV block, also known as complete heart block, shows clear signs that need quick action. It can really affect a person’s life, so knowing its symptoms and how to manage them is key.
Symptoms and Complications
People with third-degree AV block might feel dizzy, faint, or have trouble getting enough blood to their body. This is because their heart can’t beat fast enough or in a steady rhythm.
Dealing with third-degree AV block can lead to serious problems like heart failure. The heart has to work too hard, which can damage it over time.
Emergency Interventions
For those with third-degree AV block, quick action is often needed, mainly if they’re showing symptoms. Doctors might use medicines like atropine or epinephrine to help the heart beat faster.
In serious cases or when medicine doesn’t work, doctors might need to use electrical pacing. This can be done through the skin or through a vein, as a temporary fix.
Pacemaker Indications
Getting a permanent pacemaker is a common solution for third-degree AV block. It’s often recommended for those with symptoms, as it can greatly improve their life and chances of living longer.
Pacemakers help the heart beat at the right speed and rhythm. Doctors decide if a pacemaker is needed based on symptoms, the cause of the block, and the patient’s health.
Here’s a quick look at how to manage third-degree AV block:
| Management Strategy | Description | Indications |
| Medications (Atropine, Epinephrine) | Temporary increase in heart rate | Symptomatic bradycardia |
| Transcutaneous/Transvenous Pacing | Temporary electrical pacing | Severe bradycardia, hemodynamic instability |
| Permanent Pacemaker | Long-term electrical pacing | Symptomatic third-degree AV block |
Conclusion
Understanding ECG findings in third-degree AV block is key for diagnosis and care. This serious condition needs quick recognition and treatment. We’ve covered the main ECG signs, like AV dissociation and escape rhythms, which are vital for timely care.
Third-degree AV block is a serious issue where electrical signals don’t move from the atria to the ventricles. By spotting these ECG signs, we can give the best care to those affected. This complete heart block summary shows how important ECG reading is in treating third-degree AV block. It leads to a full ecg third degree av block summary.
Our talk on third-degree AV block’s ECG signs and symptoms ends with a call for quick and correct diagnosis. This third degree av block conclusion stresses the importance of ECG knowledge in giving the best patient care.
FAQ
What is third-degree AV block?
Third-degree AV block, or complete heart block, is a serious heart condition. It happens when electrical signals from the atria can’t reach the ventricles. This makes the atria and ventricles beat on their own.
What are the ECG characteristics of third-degree AV block?
ECG signs include AV dissociation and regular P waves with QRS complexes that don’t match. You might also see junctional or ventricular escape rhythms. There can be variable PR intervals, bradycardia, and capture or escape beats.
How is third-degree AV block diagnosed on ECG?
It’s diagnosed when the atria and ventricles beat independently. This is shown by regular P waves and QRS complexes without a consistent link.
What is the difference between junctional and ventricular escape rhythms in third-degree AV block?
Junctional rhythms have narrow QRS complexes and a rate of 40-60 bpm. They are more stable. Ventricular rhythms have wide QRS complexes and a slower rate (20-40 bpm). They have big implications for heart function.
What are the clinical manifestations of third-degree AV block?
Symptoms include dizziness, syncope, and decreased cardiac output. These happen because of bradycardia and the loss of coordinated heart contractions.
How is third-degree AV block managed?
Management often requires emergency actions. A pacemaker is often used to treat it. This helps restore a normal heart rate and improve heart function.
What is the significance of identifying capture or escape beats on ECG in third-degree AV block?
It’s important to tell capture and escape beats apart. This helps understand the arrhythmia’s cause. It also has big implications for patient care.
What are the typical heart rate ranges in third-degree AV block?
The heart rate is usually below 60 bpm. It can be even lower, depending on the rhythm. This can lead to bradycardia and heart problems.
References
- Martinez-Lemus, L. A. (2012). The dynamic structure of arterioles. Basic & Clinical Pharmacology & Toxicology, 110(1), 5-11. https://pubmed.ncbi.nlm.nih.gov/21989114/