Last Updated on November 25, 2025 by Ugurkan Demir

Congestive Heart Failure (CHF) is a serious condition where the heart can’t pump blood well. At Liv Hospital, we know how important it is to accurately check for CHF. Finding it early helps manage it better and improves patient care.
We put our patients first, giving them the best care for CHF. We look for the main physical exam findings that help us diagnose CHF.
Discover essential CHF physical assessment findings for better diagnosis.
CHF can cause symptoms like shortness of breath, tiredness, and swelling. Knowing what CHF is and its effects helps doctors give better care and support to patients.
Key Takeaways
- Accurate physical assessment is key for diagnosing CHF.
- Early diagnosis is vital for better CHF management.
- Liv Hospital offers full care for CHF patients.
- Finding important physical exam findings is essential for CHF assessment.
- Understanding CHF and its symptoms is key for targeted care.
Understanding Congestive Heart Failure: Pathophysiology and Clinical Impact
Congestive heart failure (CHF) affects millions worldwide. It’s important to understand its causes and effects. Healthcare providers need to know the details of CHF to care for patients well.
Definition and Mechanism of Reduced Cardiac Output
CHF means the heart can’t pump enough blood. This leads to reduced cardiac output. The body tries to compensate by tightening blood vessels and holding onto fluid, making things worse.
The heart, kidneys, and hormones work together in a complex way. This is what happens in CHF.
The reasons for less blood flow in CHF are many. They include:
- Impaired myocardial contractility
- Increased afterload due to hypertension or aortic stenosis
- Diastolic dysfunction
Rising Global Incidence and Mortality Rates
More people are getting CHF, thanks to an older population and better survival from heart attacks. Over 26 million people worldwide have CHF, and this number is growing.
| Region | Prevalence of CHF | Mortality Rate |
| North America | 2.5% | 12% |
| Europe | 2.2% | 11% |
| Asia | 1.8% | 10% |
Common Presenting Symptoms and Clinical Burden
People with CHF often have dyspnea on exertion, trouble breathing when lying down, and swelling in their legs. These symptoms make life harder and limit what they can do. CHF also means a lot of hospital visits and high costs.
Spotting and treating CHF early is key. It helps patients feel better and saves money and effort for everyone.
The Critical Role of CHF Physical Assessment in Clinical Practice
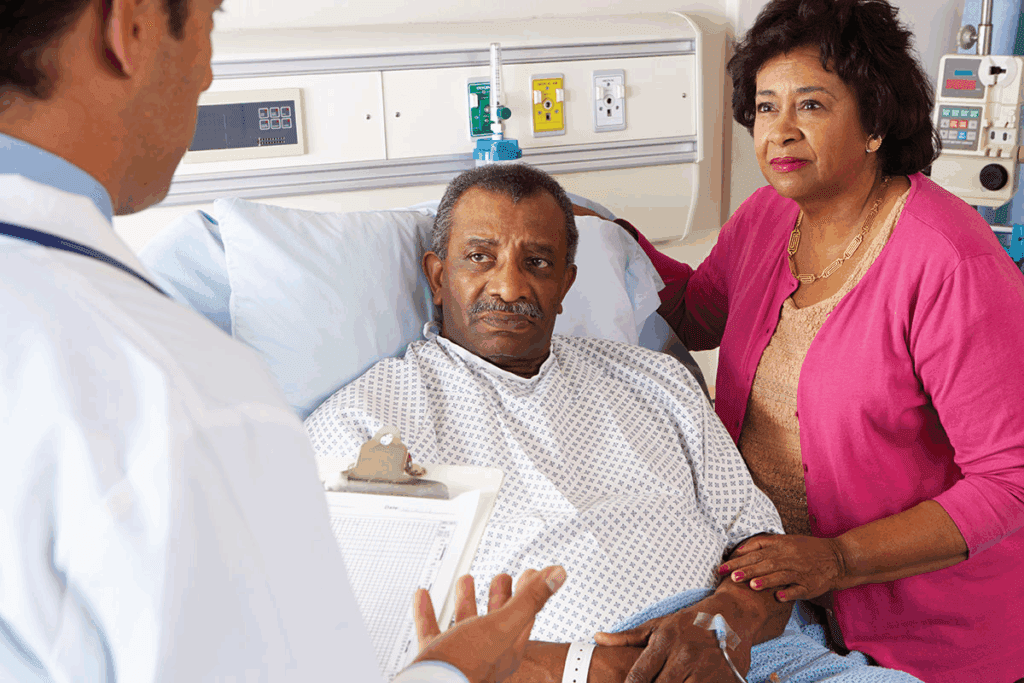
CHF physical assessment is key in clinical practice. It gives us vital info for diagnosing and treating patients. We use a detailed physical exam to check those with suspected congestive heart failure (CHF).
Evidence-Based Approach to Bedside Evaluation
An evidence-based bedside evaluation is vital for accurate CHF diagnosis. It includes a detailed medical history and physical exam. We focus on signs and symptoms linked to CHF.
- Assessing jugular venous distension
- Evaluating peripheral edema
- Auscultating for pulmonary crackles and S3 heart sounds
These signs are key in figuring out how severe CHF is. They help guide further tests.
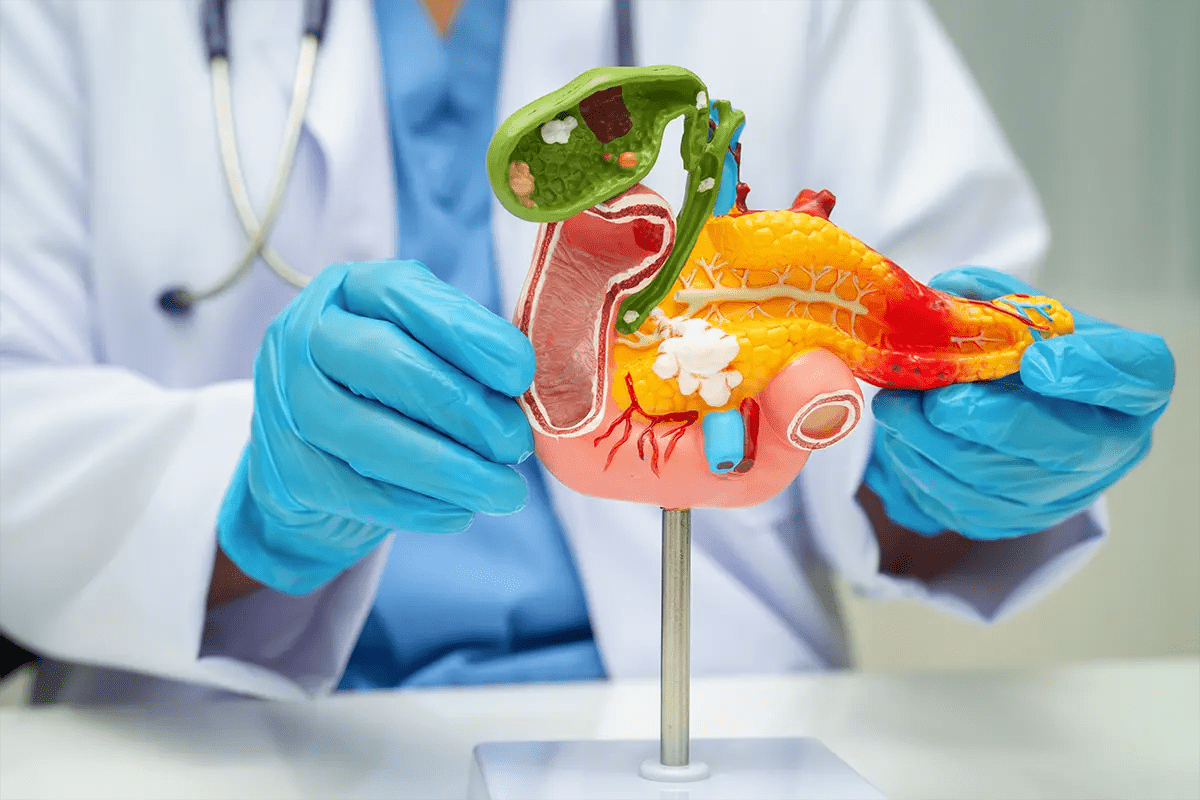
Integration with Laboratory and Imaging Studies
We combine physical assessment findings with lab and imaging studies. This confirms CHF diagnosis and its severity.
- Laboratory tests, like BNP and NT-proBNP, help confirm the diagnosis.
- Imaging studies, including echocardiography, show heart structure and function.
Using these tools together makes CHF diagnosis more accurate. It helps us decide on the best treatment.
Sensitivity and Specificity of Physical Findings
It’s important to know how sensitive and specific physical findings are. This helps us understand their clinical value.
| Physical Finding | Sensitivity | Specificity |
| Jugular Venous Distension | High | Moderate |
| Peripheral Edema | Moderate | Low |
| Pulmonary Crackles | Moderate | Moderate |
This table shows the sensitivity and specificity of common CHF physical findings. It stresses the importance of a thorough assessment.
Jugular Venous Distention: Evaluation and Clinical Significance
Understanding jugular venous distention is key for managing heart failure. Jugular venous distention (JVD) shows high central venous pressure. This is common in congestive heart failure (CHF).
Proper Technique for JVD Measurement
Measuring JVD accurately is vital. Patients should sit at a 45-degree angle with their head up. Look at the jugular venous pulse and measure its height against the sternal angle.
It’s important to tell the jugular venous pulse from the carotid pulse. The carotid pulse doesn’t change with breathing or position.
Using tangential lighting helps see the jugular venous pulse better. Healthcare providers need to know how to measure JVD well for good clinical checks.
Correlation with Central Venous Pressure
JVD is linked to central venous pressure (CVP). An elevated JVD means higher CVP, showing right-sided heart failure. This link helps in checking heart failure severity and making treatment plans.
Research shows JVD is a good sign of high CVP. Doctors use JVD to guess CVP without invasive tests.
“The jugular venous pressure is a vital sign that provides insight into the hemodynamic status of patients with heart failure.”
Source: Heart Failure Guidelines
Prognostic Value in Heart Failure Management
JVD’s role in heart failure management is huge. Worsening JVD means a worse outlook and higher risk of bad outcomes in CHF patients. Watching JVD changes helps doctors adjust treatments and improve patient results.
In summary, JVD is a critical part of CHF checks. Its correct measurement and understanding offer important insights into heart failure patients’ health and future. By grasping JVD’s importance, healthcare workers can offer better care to CHF patients.
Peripheral Edema: Distribution Patterns and Grading
Peripheral edema shows up in different ways in CHF patients. It helps doctors know how to treat them. We’ll look at how to check for it, how to write it down, and why it matters in heart failure.
Assessment Techniques and Documentation Standards
To check for peripheral edema, doctors do a detailed exam of the limbs. They use a scale to rate how bad the swelling is. They also look at where the swelling is and if it goes away when pressed.
Key parts of checking for edema are:
- Where the swelling is (e.g., both sides, one side)
- If the swelling goes away when pressed
- How bad the swelling is (0 to 4+)
Bilateral vs. Unilateral Presentation
Edema can be on both sides or just one. Swelling on both sides often means a bigger problem like CHF. Swelling on one side might mean something like a blood clot. It’s important to tell them apart to figure out what’s wrong.
Relationship to Sodium Retention and Venous Congestion
Edema in CHF comes from too much salt and water and from blood not moving well. The heart not working right means less blood to the kidneys. This makes the body hold onto salt and water. The high blood pressure also adds to the swelling.
The reasons for edema in CHF are complex. Knowing these reasons helps doctors treat the heart failure better.
Pulmonary Crackles: Detection and Characterization
Pulmonary crackles are a key sign in diagnosing and managing CHF. We use careful listening to detect and understand these sounds. This helps us make better decisions and see how severe CHF is.
Auscultation Techniques for Pulmonary Edema
Identifying pulmonary crackles through auscultation is essential. We listen to different parts of the lungs with the patient in various positions. Proper technique involves having the patient breathe deeply through their mouth while listening with a stethoscope.
Differentiating Cardiac from Non-Cardiac Causes
Not all pulmonary crackles are from CHF. We must tell the difference between cardiac and non-cardiac causes, like pneumonia or chronic lung disease. Clinical context and patient history are key in making this distinction.
Correlation with Left Ventricular Dysfunction Severity
The presence and type of pulmonary crackles can show how severe left ventricular dysfunction is. We use this to check how bad CHF is and if treatment is working.
| Crackles Characteristics | LV Dysfunction Severity | Clinical Implication |
| Fine, late inspiratory crackles | Mild | Early sign of CHF, potentially responsive to diuretics |
| Coarse, pan-inspiratory crackles | Moderate to Severe | Indicates significant pulmonary edema, may require intensive therapy |
In conclusion, pulmonary crackles are a vital sign in CHF assessment. Accurate detection and characterization through auscultation provide valuable insights into the severity of left ventricular dysfunction and guide our management strategies.
Cardiac Examination: PMI Displacement and S3 Heart Sound
When checking for congestive heart failure (CHF), looking at the PMI displacement and the S3 heart sound is key. These signs help us understand how well the heart is working and if it’s too big.
Locating the Point of Maximal Impulse
We start by checking the PMI when the patient is lying down. It’s usually at the fifth space, right in the middle. If it’s moved, it could mean the heart is getting too big, which is common in CHF.
Pathophysiology and Detection of S3 Gallop
An S3 heart sound happens early in the heart’s filling phase. It means the heart is filling up too fast, often seen in CHF. To hear it, we use the bell of the stethoscope carefully.
Assessing Ventricular Enlargement at Bedside
By looking at the PMI and the S3 sound, we can tell if the heart is too big. This helps us diagnose and treat CHF better. It lets us focus on the right treatments to help the patient.
FAQ
What is congestive heart failure (CHF) and how is it diagnosed?
CHF is when the heart can’t pump enough blood for the body’s needs. Doctors use physical checks, lab tests, and imaging to spot signs like swollen veins and lungs. These signs help confirm CHF.
What is the pathophysiology of CHF and how does it affect cardiac output?
CHF happens when the heart can’t pump well. This is due to weaker heart muscles, higher blood pressure, and too much fluid. It leads to symptoms like tiredness, breathing trouble, and swelling.
What is the significance of jugular venous distention (JVD) in CHF diagnosis?
JVD shows that the heart is failing on the right side. It’s a key sign of CHF. Doctors measure it to see how bad the heart failure is and to decide on treatment.
How is peripheral edema assessed and what are its implications in CHF?
Doctors check for swelling in the legs and feet. This swelling is common in CHF due to fluid buildup. Checking the swelling helps doctors diagnose and treat CHF.
What is the significance of pulmonary crackles in CHF diagnosis?
Crackles in the lungs mean fluid buildup and heart problems. Doctors listen for these sounds to check the heart’s function. This helps them manage the condition better.
How is the cardiac examination performed in CHF assessment?
Doctors check the heart’s function by feeling the heartbeat and listening for sounds. They also look for signs of heart enlargement. This helps in diagnosing and managing CHF.
What is the role of physical assessment in CHF diagnosis and management?
Physical checks are vital in diagnosing and managing CHF. They help spot signs like swollen veins and lungs. These findings, along with lab and imaging results, guide treatment.
What are the common presenting symptoms of CHF and how do they relate to clinical burden?
Symptoms like shortness of breath, tiredness, and swelling are common in CHF. These symptoms affect a person’s quality of life. Early diagnosis and treatment can help manage these symptoms.
How does CHF impact global health, and what are the rising incidence and mortality rates?
CHF is a big health problem worldwide, with more cases and deaths. It causes a lot of illness, death, and costs. We need better ways to prevent, diagnose, and treat CHF.
References
Government Health Resource. (2025). 7 Key Physical Exam Findings for CHF Assessment. Retrieved from https://www.aafp.org/pubs/afp/issues/2000/0301/p1319.html