A bone marrow transplant is a life-saving procedure that replaces damaged or diseased bone marrow with healthy blood-forming stem cells. This treatment is often used to manage various cancers, blood disorders, and other conditions. The goal of a bone marrow transplant is to restore the body’s ability to produce healthy blood cells by infusing healthy stem cells, which then travel to the bone marrow and begin generating new blood cells. The bone marrow transplant success rate varies depending on factors such as the patient’s condition, donor compatibility, and type of transplant, with survival rates ranging from approximately 50% to over 90% in select cases, reflecting advances in transplant techniques and post-transplant care.
Key Takeaways
- A bone marrow transplant is a procedure that replaces damaged bone marrow with healthy stem cells.
- The goal is to restore the body’s ability to produce healthy blood cells.
- The success of the transplant depends on various factors.
- Understanding the procedure and its outcomes is important.
- A successful transplant can significantly improve a patient’s quality of life.
Understanding Bone Marrow Transplants
A bone marrow transplant is a medical breakthrough for treating many blood diseases. It moves healthy cells into a patient’s body to replace bad ones.
What is a Bone Marrow Transplant?
This procedure replaces a patient’s bone marrow with healthy stem cells. It aims to cure diseases and cancers by making healthy blood cells.
Transplants are divided into autologous and allogeneic types. The success of a transplant depends on the type and the disease being treated.
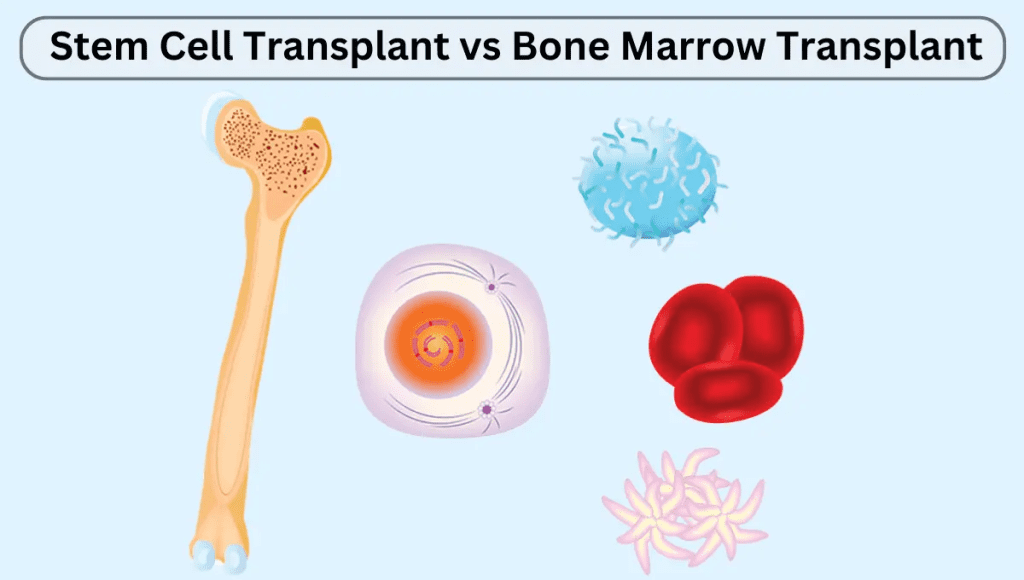
Types of Bone Marrow Transplants
There are two main types of bone marrow transplants.
- Autologous Transplant: Uses the patient’s own stem cells, collected, stored, and then reinfused.
- Allogeneic Transplant: Uses stem cells from a donor, who can be related or unrelated.
| Transplant Type | Description | Advantages | Disadvantages |
| Autologous | Uses patient’s own cells | Lower risk of GVHD | Potential for contamination with cancer cells |
| Allogeneic | Uses donor’s cells | Can provide graft-versus-tumor effect | Higher risk of GVHD and rejection |
Common Conditions Requiring Transplantation
Bone marrow transplants are used to treat both malignant conditions, such as leukemia and lymphoma, and non-malignant disorders, such as aplastic anemia and thalassemia.
- Cancers: Leukemia, lymphoma, and multiple myeloma are common reasons for transplants.
- Blood Disorders: Aplastic anemia, sickle cell disease, and thalassemia are non-cancerous conditions treated with transplants.
| Condition | Survival Rate |
| Leukemia | Varies by subtype |
| Lymphoma | 50-70% 5-year survival |
| Multiple Myeloma | 50-60% 5-year survival |
| Aplastic Anemia | 70-90% long-term survival |
Understanding bone marrow transplants helps patients and doctors make better choices about this complex treatment.
Defining Success in Bone Marrow Transplantation
Success in bone marrow transplants is measured in many ways. It looks at how well the patient does right after the transplant and how they do over time. It’s about understanding the transplant process and what affects the results.
Short-term vs. Long-term Success Metrics
Right after the transplant, doctors check if the new blood cells are working. This is called engraftment. Later, they look at how long the patient stays disease-free and how long they live.
- Engraftment: When the new stem cells start making blood cells.
- Disease-free survival: How long a patient stays without disease after treatment.
- Overall survival: The percentage of patients alive after a certain time post-transplant.
Clinical Definitions of Engraftment
Engraftment is a big step in a bone marrow transplant’s success. It happens when the new blood cells start to grow. This is shown when the neutrophil count goes over 500 cells per microliter.
Disease-free Survival as a Measure of Success
Disease-free survival is a key long-term check. It shows if the treatment worked to get rid of the disease. Many things can affect this, like the disease type, the patient’s health, and how well the donor and recipient match.
Knowing these metrics helps patients and doctors understand transplant success. It helps them make better choices about treatment.
The Timeline of Recovery After Transplant
Knowing the recovery timeline after a bone marrow transplant is key for patients and their families. The journey is long and has different stages, each with its own hurdles and achievements.
Immediate Post-Transplant Period (0-30 Days)
The first few weeks after a transplant are very important. Doctors watch for signs of the new marrow working and for any problems like infections or GVHD. Patients usually stay in the hospital or nearby to get help fast if they need it.
Early Recovery Phase (30-100 Days)
In the early stages of recovery, patients start to see their blood counts go up. But, their immune system is weak, making them more likely to get sick. It’s important to see the doctor often during this time to check on progress and fix any issues quickly.
Long-term Recovery (Beyond 100 Days)
As patients get further into recovery, their immune system starts to get stronger, and they can start doing more things again. But, some might face late problems like chronic GVHD or damage to organs. It’s important to keep seeing the doctor and getting support during this time.
| Recovery Phase | Key Characteristics | Common Challenges |
| Immediate Post-Transplant (0-30 Days) | Hospitalization, initial engraftment signs | Infections, GVHD |
| Early Recovery (30-100 Days) | Rising blood counts, immune system reconstitution begins | Infections, GVHD |
| Long-term Recovery (Beyond 100 Days) | Gradual immune system recovery, return to normal activities | Late effects, chronic GVHD, organ damage |
Every person’s journey after a bone marrow transplant is different. Knowing about the different stages can help patients and their families get ready for what’s ahead. It helps them understand what to expect during the recovery process.
Key Indicators of Successful Engraftment
Recovery after a bone marrow transplant is tracked through key signs of engraftment success. This success is vital for the transplant’s success. It affects the bone marrow transplant success rate and stem cell bone marrow transplant success rate.
Blood Count Recovery
Recovery of blood counts is a main sign of successful engraftment. This includes more white blood cells, red blood cells, and platelets. Neutrophil recovery is key, showing the body can fight infections.
Chimerism Analysis
Chimerism analysis checks for donor cells in the body. A higher donor cell percentage means engraftment is likely successful.
Immune System Reconstitution Markers
Rebuilding the immune system is key to engraftment. Watching for T cells and B cells helps see if the immune system is working right.
| Indicator | Description | Significance |
| Blood Count Recovery | Increase in white blood cells, red blood cells, and platelets | Signifies the body’s ability to produce blood cells |
| Chimerism Analysis | Presence and proportion of donor cells | Indicates the level of donor cell engraftment |
| Immune System Reconstitution | Recovery of T cells and B cells | Marks the restoration of immune function |
Keeping an eye on these signs is key to knowing if the bone marrow transplant worked. It helps in making the right choices for care after the transplant.
Bone Marrow Transplant Success Rates: What the Data Shows
Looking at bone marrow transplant survival statistics gives us a peek into how well this treatment works. It’s a key treatment for serious diseases like leukemia and lymphoma.
Overall Success Statistics
The success rate of bone marrow transplants has grown thanks to new medical tech and better care after the transplant. Success rates change based on the disease, the transplant type, and the patient’s health. For example, non-malignant conditions have different results than malignant ones.
Recent studies show a big jump in survival rates for transplant patients. This is thanks to better donor matching, new immune therapies, and better care.
Success Rates by Disease Type
Success rates for bone marrow transplants vary by disease. For instance, acute myeloid leukemia patients’ survival rates depend on the disease’s stage at transplant. Multiple myeloma patients have seen better results with new treatments and transplants.
Knowing these disease-specific success rates helps set realistic hopes and make better treatment choices.
Factors Influencing Statistical Outcomes
Many things affect bone marrow transplant success rates. These include the patient’s age, health, disease specifics, and how well the donor and recipient match. The transplant type, autologous or allogeneic, also affects success.
Improvements in prep regimens and post-transplant care have also boosted results. Keeping a close eye on patients is key to spotting and treating problems early.
Medical Tests That Measure Transplant Success
Doctors use many tests to check if a bone marrow transplant worked. These tests show how well the patient is recovering and if the transplant was successful.
Complete Blood Counts
The Complete Blood Count (CBC) is a key test. It checks the levels of blood cells like white blood cells, red blood cells, and platelets. When a patient starts to have more healthy blood cells, it means the transplant is working.
Key components of a CBC include:
- White Blood Cell Count (WBC): Shows if the body can fight off infections.
- Red Blood Cell Count (RBC): Important for carrying oxygen.
- Platelet Count: Crucial for blood clotting.
Bone Marrow Biopsies
Bone marrow biopsies are also important. They take a small sample of bone marrow for tests. Doctors look at the marrow’s health, if there’s any disease, and how well it’s working.
The biopsy results can indicate:
- Engraftment status: If the donor cells are making blood cells.
- Disease recurrence: If the original disease is coming back.
Molecular Testing for Disease Markers
Molecular testing finds specific genetic markers of the disease. Tests like PCR or FISH can spot any remaining disease cells. This helps doctors know the risk of the disease coming back.
| Test | Purpose | Indications of Success |
| Complete Blood Count (CBC) | Measures blood cell levels | Normalizing blood cell counts |
| Bone Marrow Biopsy | Evaluates marrow health and disease presence | Healthy marrow cellularity, absence of disease |
| Molecular Testing | Detects genetic markers of disease | Undetectable or minimal residual disease |
Imaging Studies
Imaging tests like PET scans or CT scans check how the body is doing after the transplant. They look for any signs of disease coming back or other problems.
These tests help doctors fully understand if a bone marrow transplant was successful. They make sure the patient gets the best care possible.
Common Complications That May Affect Success

After a bone marrow transplant, patients may face complications that can change their outcome. Bone marrow transplants save many lives but come with risks. These risks can affect how well the transplant works.
Graft-Versus-Host Disease (GVHD)
Graft-versus-host disease happens when the donor’s immune cells attack the recipient’s body. It can be acute, happening in the first 100 days, or chronic, appearing later.
GVHD Management: Doctors use immunosuppressive drugs to control GVHD. Sometimes, GVHD can help fight cancer, making the transplant more effective.
Infections
Patients are at high risk for infections because their immune system is weakened. They can get serious infections from bacteria, viruses, and fungi.
Infection Prevention: To prevent infections, doctors give antibiotics and antivirals. Patients also learn about hygiene to avoid germs.
Organ Damage
Organ damage can happen to the liver, lungs, and heart. It might be caused by the treatment before the transplant or problems after it.
Graft Failure
Graft failure means the bone marrow doesn’t make blood cells. It can be primary, where it never works, or secondary, where it fails after working.
| Complication | Description | Management |
| Graft-Versus-Host Disease | Donor immune cells attack recipient’s body | Immunosuppressive medications |
| Infections | Bacterial, viral, fungal infections due to immunosuppression | Prophylactic antibiotics, antivirals, hygiene practices |
| Organ Damage | Damage to organs like liver, lungs, heart | Monitoring, supportive care |
| Graft Failure | Failure of bone marrow to produce blood cells | Re-transplantation, supportive care |
Knowing about these complications helps set realistic goals and improve results for bone marrow transplant patients. While these risks are serious, medical progress is making these procedures safer and more successful.
The Role of Donor Matching in Transplant Outcomes
Bone marrow transplant success rates depend a lot on donor matching. The match between the donor and the recipient is key for a good transplant.
Importance of HLA Matching
Human Leukocyte Antigen (HLA) matching is very important in choosing a donor. HLA genes help our immune system fight off diseases. A good match between donor and recipient lowers the risk of complications.
HLA matching is done by testing the genes of both the donor and the recipient. The closer the match, the better the transplant results.
Related vs. Unrelated Donors
Donors can be related or not. Siblings are often a good match because they share genes.
Unrelated donors are found through registries. The chance of finding a match depends on the registry’s diversity and the recipient’s HLA type.
| Donor Type | Match Rate | Advantages | Disadvantages |
| Related | Higher | Lower risk of GVHD, faster engraftment | Limited availability, possible inherited diseases |
| Unrelated | Variable | Wide availability, diverse donor pool | Higher risk of GVHD, longer search time |
Haploidentical Transplants
Haploidentical transplants use donors who are half-matched, like a parent or child. These transplants are becoming more common thanks to new treatments.
They are an option for those without a fully matched donor.
Cord Blood Options
Cord blood transplants use stem cells from umbilical cord blood. These cells are less mature and have a lower risk of GVHD.
They are useful for those with few donor options, but the cell dose can be a problem.
In conclusion, donor matching is very important for bone marrow transplant success. Knowing about HLA matching, the role of related and unrelated donors, and options like haploidentical and cord blood transplants helps make better choices.
Age and Health Factors Affecting Transplant Success
When thinking about a bone marrow transplant, age and health are key. These factors greatly affect how well the transplant will work. It’s important for doctors to look at these closely before starting the transplant.
Pediatric vs. Adult Outcomes
Age is a big factor in bone marrow transplant success. Younger patients usually do better because they have fewer health problems and a stronger immune system. Kids often have the best chances because of their health and strength.
Adults, and older adults in particular, face more challenges. But, thanks to better medical care and transplant methods, adults can also have good outcomes.
Impact of Pre-existing Conditions
Health problems before the transplant can change its success. Issues like diabetes, heart disease, and past infections can make things harder.
- Diabetes: Patients with diabetes might take longer to recover and are more likely to get infections.
- Heart Disease: Heart problems can lead to more complications during and after the transplant.
- Previous Infections: Severe infections in the past can weaken the immune system and affect health after the transplant.
Performance Status Before Transplant
A patient’s health before the transplant is a big clue to their outcome. Those who are more active and healthy tend to do better and have fewer problems.
Comorbidity Indices
Comorbidity indices measure how health problems affect patient outcomes. These tools help doctors understand risks and plan treatments better.
By looking at age and health, doctors can guess how well a bone marrow transplant will work. They can then make treatment plans that fit each patient’s needs.
Leukemia Bone Marrow Transplant Life Expectancy
Bone marrow transplants can cure leukemia, but life expectancy varies by type. Success depends on the patient’s health, leukemia characteristics, and donor-recipient match.
Acute Myeloid Leukemia Outcomes
Patients with Acute Myeloid Leukemia (AML) may see good results from a transplant. Those in remission tend to live longer than those with active disease.
A quote from a renowned hematologist emphasizes the disease’s status at transplant:
“The status of the disease at the time of transplant is a critical factor in determining the outcome for AML patients.”
Acute Lymphoblastic Leukemia Outcomes
Acute Lymphoblastic Leukemia (ALL) patients also benefit from transplants, mainly those with high-risk features or in second remission. The graft-versus-leukemia effect helps improve outcomes.
Chronic Leukemias and Transplantation
Chronic leukemias, like Chronic Myeloid Leukemia (CML) and Chronic Lymphocytic Leukemia (CLL), have varied transplant outcomes. The decision to transplant is changing with new treatments.
Myelodysplastic Syndrome Outcomes
Myelodysplastic Syndromes (MDS) can turn into AML. Transplanting bone marrow can cure MDS, with results based on disease risk and patient health.
The life expectancy after a bone marrow transplant for leukemia depends on many factors. These include the disease type, its status at transplant, and the patient’s health. Knowing these factors is key to managing expectations and making informed treatment choices.
Success Rates for Lymphomas and Multiple Myeloma
Knowing the success rates of bone marrow transplants is key for those with lymphomas or multiple myeloma. These cancers affect the immune system and bone marrow. Thanks to bone marrow transplants, treatment outcomes have greatly improved.
Hodgkin Lymphoma Transplant Outcomes
Hodgkin lymphoma, a cancer of white blood cells, shows good results with bone marrow transplants. Success rates depend on the disease stage and the patient’s health.
Non-Hodgkin Lymphoma Transplant Outcomes
Non-Hodgkin lymphoma is a wide category, and bone marrow transplants are a key treatment. The transplant’s success depends on the lymphoma type and how well the patient has responded to treatments.
Multiple Myeloma and Transplantation
Multiple myeloma, a cancer of plasma cells in the bone marrow, has seen big improvements with bone marrow transplants. High-dose chemotherapy followed by a transplant has boosted survival rates for many.
For lymphomas and multiple myeloma, bone marrow transplants can be very effective. They offer a chance for a cure for some patients. Here’s a summary of the key outcomes:
| Disease Type | Success Rate Range | Factors Influencing Success |
| Hodgkin Lymphoma | 40-70% | Disease stage, patient health |
| Non-Hodgkin Lymphoma | 30-60% | Lymphoma subtype, previous treatments |
| Multiple Myeloma | 50-80% | Response to prior therapy, patient age |
These numbers highlight the need for personalized treatment plans. Bone marrow transplants can greatly improve outcomes for these patients.
Success Rates for Non-Malignant Conditions
Bone marrow transplantation is a promising treatment for many non-malignant conditions. It has shown great success in managing diseases that were hard to treat before.
Aplastic Anemia
Aplastic anemia makes it hard for the bone marrow to make blood cells. Bone marrow transplants have been very effective for this condition. They work best for patients who don’t respond well to other treatments.
Success rates for aplastic anemia patients can reach 80-90%. This depends on the match with the donor and the patient’s age.
Immune Deficiency Disorders
Immune deficiency disorders, like Severe Combined Immunodeficiency (SCID), can be treated with bone marrow transplants. The success rate varies based on the disorder and the patient’s health at the time of transplant.
Early diagnosis and intervention are key to better outcomes.
Inherited Metabolic Disorders
Inherited metabolic disorders, like Hurler syndrome and adrenoleukodystrophy, also benefit from bone marrow transplants. The procedure can replace faulty cells with healthy ones, potentially stopping the disease’s progression.
Success rates for these conditions are generally high. Studies show improved survival and quality of life for patients.
Hemoglobinopathies
Hemoglobinopathies, such as sickle cell disease and thalassemia major, are also treated with bone marrow transplants. The success rates are encouraging, with some patients seeing a significant reduction in disease severity.
Yet, the decision to have a transplant is made carefully. It’s weighed against the risks and possible complications.
In conclusion, bone marrow transplants are a valuable treatment for many non-malignant conditions. Success rates are encouraging. Further advancements in transplant techniques and care are expected to improve outcomes even more.
Stem Cell Bone Marrow Transplant Success Rate Compared to Traditional BMT
Different sources of stem cells have different success rates in bone marrow transplants. The choice depends on the patient’s condition, donor availability, and the disease being treated.
Peripheral Blood Stem Cell Transplants
Peripheral blood stem cell transplants are becoming more common. They have a high success rate and fewer complications than traditional bone marrow transplants. The ease of collection and the rapid engraftment make them a good choice for many patients.
Studies show peripheral blood stem cell transplants lead to faster recovery and lower mortality. But, they might have a higher risk of graft-versus-host disease (GVHD) than bone marrow.
Cord Blood Transplants
Cord blood transplants are great for urgent cases without a matched donor. The ability to use cord blood units with less stringent HLA matching requirements helps those from diverse backgrounds. This makes it a valuable option.
Yet, cord blood transplants have slower engraftment and higher graft failure risks. Improvements in double cord blood units and conditioning regimens have helped outcomes.
Bone Marrow Harvest Outcomes
Traditional bone marrow harvests collect stem cells directly from the bone marrow. It’s a long-standing method with a known risk profile. This method is often chosen for certain clinical scenarios.
Bone marrow harvests are preferred for lower chronic GVHD risk. But, the procedure is more invasive and can lead to longer recovery times for donors.
Comparative Success Metrics
Success rates vary among stem cell sources, considering overall survival, disease-free survival, and GVHD incidence. Each type of transplant has its advantages and challenges. The choice must match the patient’s needs.
The decision on which transplant to use depends on the patient’s condition, disease, and donor availability. Advances in techniques are improving outcomes for all stem cell transplants.
Recovery Milestones: What Patients Experience
After a bone marrow transplant, patients go through many recovery milestones. These milestones show if the transplant worked and how well the patient is doing.
Physical Recovery Markers
One early sign of getting better is when blood counts start to rise. This means the new bone marrow is making healthy cells. Patients might also start to feel more energetic, but this can take time.
Physical therapy and rehabilitation are key. They help patients get stronger and move better.
Return to Normal Activities
As patients get better, they can start doing things they used to do. Going back to work or school is a big step. It shows they’re getting healthier and can adapt well.
But, how fast they get back to normal varies. It depends on their health and if they face any problems.
Psychological Adaptation
The mental journey is as important as the physical one. Patients feel many emotions, like relief, gratitude, anxiety, and depression. Counseling and support groups help a lot. They make it easier for patients to deal with their feelings.
Quality of Life Improvements
The real test of a bone marrow transplant is how well the patient lives afterward. Better physical health, emotional state, and enjoying activities again all add up. Patients see their lives improve in different ways, but many live fulfilling lives.
Knowing about these recovery milestones helps patients and their families. It gives them hope and clarity as they go through the transplant journey. By focusing on physical recovery, getting back to normal, mental health, and quality of life, patients can see their progress and the chance for a good outcome.
Long-Term Follow-Up: What to Expect
The journey doesn’t end with the bone marrow transplant; it continues with long-term follow-up. After undergoing a bone marrow transplant, patients enter a critical phase of care. This phase is designed to monitor their health, manage complications, and address any late effects of the transplant.
Routine Monitoring Schedule
Long-term follow-up care involves a routine monitoring schedule. This includes regular check-ups with the healthcare team, blood tests, and other diagnostic procedures. These are done to assess the patient’s overall health and the function of the new bone marrow.
These monitoring activities are key for early detection of any issues. Issues like graft-versus-host disease (GVHD), infections, or organ damage. The visits may decrease over time but are essential for the patient’s care plan.
Late Effects and Complications
Late effects and complications can arise months or even years after the transplant. These may include chronic GVHD, organ dysfunction, and an increased risk of secondary cancers. Understanding these effects is vital for managing them effectively.
Patients should be aware of the signs and symptoms of these complications. They should report them to their healthcare provider promptly. Early intervention can significantly improve outcomes.
Secondary Malignancies Risk
One of the significant concerns during long-term follow-up is the risk of secondary malignancies. Factors like the conditioning regimen used before the transplant and the patient’s overall health can influence this risk.
Regular monitoring and screenings are part of the long-term care plan. They help detect any new cancers early. Patients are also encouraged to follow general cancer prevention guidelines. This includes maintaining a healthy lifestyle and attending recommended screenings.
Fertility and Endocrine Issues
Fertility and endocrine issues are other aspects of long-term follow-up care. The conditioning regimen for the bone marrow transplant can affect gonadal function. This can lead to infertility or hormonal imbalances.
Patients who are concerned about fertility may wish to discuss options such as sperm or egg banking with their healthcare provider before undergoing the transplant. For those experiencing endocrine issues, hormone replacement therapy or other treatments may be necessary.
Conclusion: The Future of Bone Marrow Transplantation
The field of bone marrow transplantation is growing fast. New research and better care methods are leading to better results for patients. The future of bone marrow transplantation looks bright.
New ways to match donors and manage side effects are making transplants more successful. The use of advanced technologies and personalized medicine will make transplants even safer and more effective.
As doctors keep exploring new possibilities in bone marrow transplantation, patients will get better treatments. The future is full of hope, with new discoveries that will change how we treat blood diseases.
FAQ
What is a bone marrow transplant success rate?
The success rate of a bone marrow transplant depends on several things. These include the disease, the type of transplant, and the patient’s health. Generally, the survival rate ranges from 50% to 90%.
How is the success of a bone marrow transplant measured?
Success is measured by how well the patient’s blood counts recover. It also looks at chimerism analysis and disease-free survival. Tests like complete blood counts and bone marrow biopsies help assess the transplant’s success.
What are the common complications that can affect the success of a bone marrow transplant?
Complications like graft-versus-host disease (GVHD) and infections can affect success. Organ damage and graft failure are also common. These issues can impact the patient’s quality of life and survival.
How does donor matching impact bone marrow transplant outcomes?
Donor matching is key for transplant success. Human leukocyte antigen (HLA) matching helps avoid GVHD and ensures engraftment. Options include related and unrelated donors, as well as cord blood.
What is the impact of age and health factors on bone marrow transplant success?
Age and health greatly influence transplant success. Kids usually do better than adults. Conditions like pre-existing diseases can make success harder.
What are the success rates of bone marrow transplants for leukemia?
Success rates for leukemia vary by type. For acute myeloid leukemia (AML), survival is about 50-60%. Acute lymphoblastic leukemia (ALL) has a 40-50% survival rate. Chronic leukemias and myelodysplastic syndromes have different success rates.
What are the success rates of bone marrow transplants for lymphomas and multiple myeloma?
Success rates for lymphomas and multiple myeloma depend on the disease and patient factors. Hodgkin lymphoma has a 60-70% survival rate. Non-Hodgkin lymphoma and multiple myeloma have 50-60% survival rates.
How do different types of stem cell transplants compare in terms of success rates?
Different stem cell transplants have varying success rates. Peripheral blood stem cell transplants often have faster engraftment and higher success. Cord blood transplants have a higher risk of graft failure.
What can patients expect during long-term follow-up after a bone marrow transplant?
Patients will need regular monitoring with blood tests and check-ups. This is to watch for late effects and complications. They may face risks of secondary malignancies, fertility issues, and endocrine problems.
What is the life expectancy after a bone marrow transplant for leukemia?
Life expectancy after a transplant for leukemia varies. It depends on the leukemia type, the patient’s health, and transplant success. Patients who achieve disease-free survival generally have a better outlook.
References
- ElGohary, G., et al. (2023). Engraftment syndrome after allogeneic stem cell transplantation: incidence, risk, and outcomes. Bone Marrow Transplantation / Nature, (Online). Retrieved from https://www.nature.com/articles/s41409-022-01849-6
- Hutt, D., & co-authors. (2017). Engraftment, graft failure, and rejection. In Hematopoietic Stem Cell Transplantation, NCBI Bookshelf. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK543659/
- Lindahl, H., Vonlanthen, S., Valentini, D., Björklund, A., Sundin, M., & Mielke, S., et al. (2022). Lineage-specific early complete donor chimerism and risk of relapse after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia. Bone Marrow Transplantation / Nature, (Online). Retrieved from https://www.nature.com/articles/s41409-022-01615-8
- Miura, S., Ueda, K., Minakawa, K., Nollet, K. E., & Ikeda, K. (2024). Prospects and potential for chimerism analysis after allogeneic hematopoietic stem cell transplantation. Cells, 13(11), 993. Retrieved from https://www.mdpi.com/2073-4409/13/11/993