Last Updated on December 1, 2025 by Bilal Hasdemir
Every year, millions of people worldwide suffer injuries that need immediate surgery. Trauma surgeries are key to saving lives and preventing disabilities. The ultimate list of common trauma surgeries. Our essential guide reveals the critical, awful procedures surgeons perform to save lives.
Orthopedic trauma surgery is very important. It fixes bone and muscle injuries from accidents or violence.
The need for prompt and appropriate emergency surgery is significant. It greatly affects how well patients do in critical care.
Key Takeaways
- Trauma surgeries include many types, like orthopedic, abdominal, thoracic, and neurosurgical.
- Orthopedic trauma surgery is key for fixing bone and muscle injuries.
- Emergency surgery is vital for saving lives and preventing long-term disability.
- Quick surgery is critical in trauma care.
- Surgical trauma care is essential for better patient outcomes.
The need for prompt and appropriate emergency surgery is significant.
Definition and Scope of Trauma Surgery

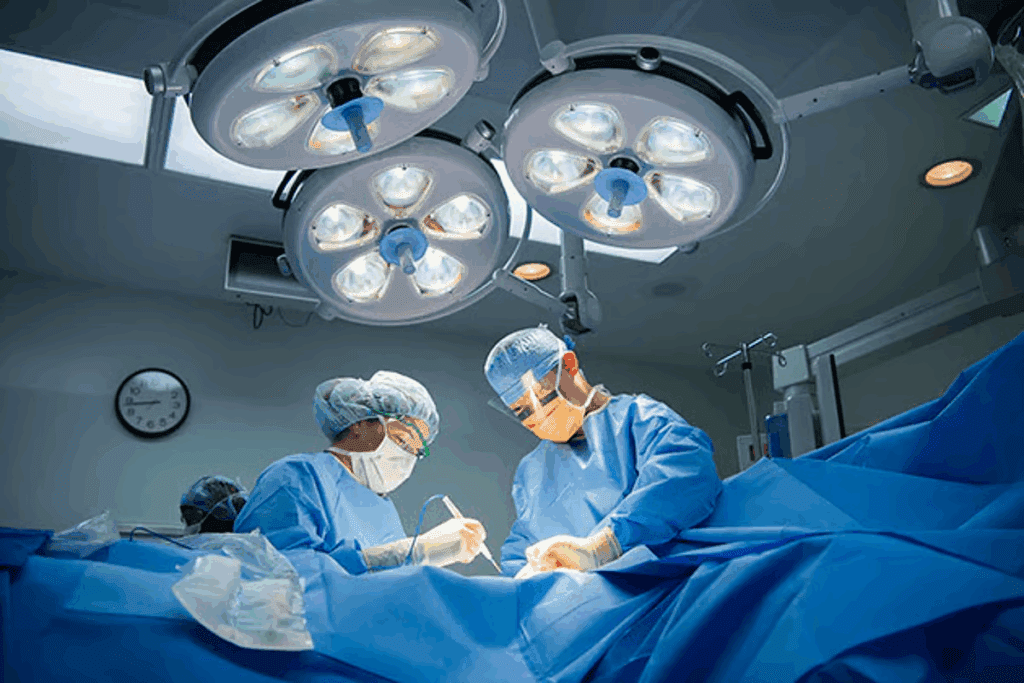
Trauma surgery deals with injuries from accidents, violence, and natural disasters. It includes emergency and reconstructive surgeries. Surgeons must handle complex and dangerous injuries.
Trauma care has gotten better. New surgical techniques and imaging technologies are key. These advancements have greatly improved patient care.
Historical Development of Trauma Care
The history of trauma care is filled with important milestones. The first trauma centers were set up to focus on trauma care. They brought together resources and expertise.
Advances in surgery, imaging, and trauma centers have shaped trauma care. This evolution has led to better patient care.
Trauma Centers and Their Classification
Trauma centers are ranked from Level I to Level III. Level I centers offer the most advanced care. They have the staff and facilities for the most critical cases.
| Level | Description | Capabilities |
| Level I | Highest level of care | Comprehensive care, including specialized staff and facilities |
| Level II | High level of care | Initial stabilization and assessment, with some specialized care |
| Level III | Moderate level of care | Initial assessment and stabilization, with some surgical capabilities |
Knowing how trauma centers are classified is important. It helps ensure patients get the right care. It also helps emergency teams decide where to send patients.
In summary, trauma surgery has made huge strides. Advances in care and the creation of trauma centers have been key. Understanding trauma centers is vital for grasping the complexity of trauma care.
Common Trauma Surgeries in the United States
Trauma surgeries are a big problem for the US healthcare system. They affect different people and places in different ways. Things like money, health access, and violence or accidents play big roles.
Statistical Overview of Trauma Cases
Trauma is a big cause of sickness and death in the US. Millions of people get hurt every year. The American College of Surgeons says trauma is a big part of emergency room visits and hospital stays.
In 2019, the CDC said accidents were among the top 10 reasons people died in the US. The cost of treating trauma is huge, over $400 billion a year.
| Year | Total Trauma Cases | Trauma-Related Deaths | Estimated Cost (Billions) |
| 2018 | 2,815,612 | 146,571 | $380 |
| 2019 | 2,933,495 | 149,463 | $410 |
| 2020 | 3,045,111 | 152,191 | $420 |
Demographic Patterns in Trauma Surgery
Some groups get hurt more than others. Young men are at high risk because of violence, sports, and car accidents.
Age and gender matter a lot. Older people fall and get hurt, while younger people get hurt in accidents or violence.
Impact of Geographic and Socioeconomic Factors
Where you live and how much money you have affect trauma surgery. Rural areas have trouble getting to trauma centers because of distance.
Socioeconomic status also matters. People with less money have trouble getting the care they need. This can lead to worse outcomes and more deaths.
It’s clear we need to do more to help people in different places and with different incomes get better trauma care.
Patient Evaluation and Preparation for Trauma Surgery
The need for prompt and appropriate emergency surgery is significant.
Initial Assessment and Triage
The first check-up on a trauma patient is key. It needs to be quick and thorough. Triage helps figure out how urgent the patient’s needs are. This helps make sure everyone gets the care they need.
The first steps usually follow the Advanced Trauma Life Support (ATLS) guide. It focuses on finding life-threatening injuries first. This includes checking the airway, breathing, circulation, disability, and exposure (ABCDE).
Diagnostic Imaging in Trauma
Imaging is a big part of checking trauma patients. Tools like X-rays, CT scans, and ultrasound help find injuries fast.
Which imaging tool to use depends on the patient’s situation and what injuries are suspected. For example, CT scans are great for spotting internal injuries in stable patients.
| Imaging Modality | Primary Use in Trauma | Advantages |
| X-ray | Initial assessment of bone fractures and dislocations | Quick, widely available |
| CT Scan | Detailed assessment of internal injuries | High sensitivity for detecting internal injuries |
| Ultrasound | Rapid assessment of free intraperitoneal fluid and cardiac activity | Non-invasive, quick, bedside |
Preparing the Critically Injured Patient for Surgery
Getting a critically injured patient ready for surgery is a big job. It involves making sure their vital signs are stable and their immediate needs are met. This might include giving fluids, blood, and managing pain and anxiety.
The aim is to make the patient as ready as possible for surgery. Good communication among the trauma team, surgeons, and other healthcare workers is key.
Orthopedic Trauma Surgery
Orthopedic trauma surgeons are key in helping patients with severe bone injuries. They do many complex surgeries, like fixing fractures and saving limbs. Each surgery needs great skill and knowledge of bones.
Fracture Repair and Fixation Techniques
Fixing fractures is a big part of their job. Surgeons use different methods to put bones back together. This helps bones heal and function better.
The right method depends on the fracture’s type and the patient’s health.
Some common ways to fix fractures include:
- Intramedullary nailing for long bone fractures
- Plate fixation for periarticular fractures
- External fixation for temporary stabilization
A top orthopedic surgeon says, “The goal is to fix bones well and keep soft tissues safe.”
“The goal is to restore the patient’s pre-injury level of function as closely as possible.”
Joint Reconstruction After Trauma
After severe injuries, fixing joints is often needed. This can be simple or very complex. The aim is to make joints work right again.
| Procedure | Description | Indications |
| Arthroscopic Debridement | Removal of damaged cartilage and bone fragments | Mild to moderate joint damage |
| Osteotomy | Realignment of bone to improve joint congruence | Malunion or deformity |
| Joint Replacement | Replacement of damaged joint with prosthesis | Severe joint destruction |
Amputation and Limb Salvage Procedures
Choosing between amputation and saving a limb is tough. Doctors look at how bad the injury is and the patient’s health. They also think about how well the limb might work again.
Trying to save a limb means doing many things. This includes cleaning wounds, stabilizing bones, and rebuilding soft tissues.
A study on saving limbs said, “Success comes from teamwork among doctors, vascular experts, and rehab teams.” Thanks to new surgery techniques and prosthetics, saving limbs or amputations are getting better.
Abdominal Trauma Surgery
Abdominal trauma surgery is a specialized field. It deals with complex injuries to solid and hollow organs. Surgeons use various techniques to manage these injuries.
Exploratory Laparotomy and Damage Control
Exploratory laparotomy is a key procedure in this field. It lets surgeons check injuries inside the abdomen. Damage control surgery is important here. It aims to stabilize the patient by stopping bleeding and preventing infection before fixing the damage.
Doctors decide on exploratory laparotomy based on how the patient looks and what tests show. They make an incision to see the organs and check for injuries.
Solid Organ Injuries (Liver, Spleen, Kidney)
Injuries to solid organs like the liver, spleen, and kidney are common. How these injuries are managed depends on their severity and how stable the patient is.
| Organ | Common Injuries | Management Strategies |
| Liver | Lacerations, Hematomas | Packing, Resection, Embolization |
| Spleen | Lacerations, Rupture | Conservative Management, Splenectomy |
| Kidney | Lacerations, Vascular Injuries | Conservative Management, Nephrectomy |
Hollow Organ Injuries (Intestines, Stomach, Bladder)
Hollow organ injuries are tricky because they can lead to leakage and infection. Quick diagnosis and surgery are key to avoiding serious problems.
- Intestinal Injuries: Repair or resection of the affected segment.
- Gastric Injuries: Primary repair, with or without reinforcement.
- Bladder Injuries: Repair, with or without urinary diversion.
Handling abdominal trauma needs a team effort. Surgeons and other healthcare workers work together to get the best results for patients.
Neurosurgical Trauma Procedures
Neurosurgical interventions are key in treating traumatic brain injuries. These injuries are a major cause of death and disability worldwide. The goal is to save lives and prevent long-term brain damage.
Craniotomy for Traumatic Brain Injury
A craniotomy is a surgery where part of the skull is removed. This allows surgeons to access the brain. It’s critical for relieving pressure from swelling or bleeding in the brain.
Doctors decide on a craniotomy based on the injury’s severity and complications like bleeding in the brain. Intracranial pressure monitoring helps guide the surgery.
Intracranial Pressure Monitoring and Management
Intracranial pressure (ICP) monitoring is essential for severe brain injuries. It involves placing a device in the brain to measure pressure.
Managing ICP is vital to prevent further brain damage. Doctors use sedation, hyperventilation, and sometimes decompressive craniectomy to control it.
| ICP Management Strategy | Description | Indications |
| Sedation | Use of sedatives to reduce agitation and stress | Elevated ICP, agitation |
| Hyperventilation | Temporary reduction of CO2 levels to decrease ICP | Acute ICP elevation |
| Decompressive Craniectomy | Surgical removal of a portion of the skull to relieve pressure | Refractory ICP elevation |
Skull Fracture Repair and Reconstruction
Severe head trauma can cause skull fractures. Some fractures need surgery to repair the skull and protect the brain.
Skull fracture repair uses plates, screws, and bone grafts. These techniques help rebuild the skull’s protective function.
Surgical Management of Traumatic Hematomas
Traumatic hematomas can result from head trauma. These include epidural, subdural, and intracerebral hematomas. Surgery is often needed to relieve pressure on the brain.
The timing and method of surgery depend on the hematoma’s size, location, and effect on brain pressure and function.
Thoracic Trauma Surgery
Thoracic trauma surgery deals with injuries to the chest. These injuries can be very serious and need quick surgery. Surgeons must be very skilled and precise in these surgeries.
Chest Tube Insertion and Thoracostomy
Chest tube insertion, or thoracostomy, is key in managing chest injuries. It involves putting a tube into the pleural space to remove fluid, air, or blood. This helps relieve pressure on the lungs and heart. Effective chest tube placement is very important for better patient outcomes.
Emergency Thoracotomy Procedures
Emergency thoracotomy is a surgery done in emergency situations. It’s used for severe chest injuries with a lot of bleeding or cardiac arrest. Prompt decision-making is key for success.
The steps include making a chest incision, spreading the ribs, and entering the thoracic cavity. The aim is to stop bleeding, fix injuries, and get the heart working again.
Cardiac and Great Vessel Repair
Fixing cardiac and great vessel injuries is very tough in thoracic trauma. It needs precise surgical techniques and deep knowledge of the heart. Surgeons must be good at handling complex cases.
Fixing heart injuries might mean sewing up tears or closing holes. Great vessel injuries, like major artery and vein problems, need careful repair to avoid more issues.
Pulmonary Injury Management
Pulmonary injuries in thoracic trauma can be minor or very serious. Treatment varies from conservative management for small injuries to surgery for severe ones.
Surgery for lung injuries might include removing a lobe, doing a wedge resection, or fixing lung tears. The goal is to keep as much lung function as possible while fixing the injury.
Spinal Trauma Surgery
Spinal trauma surgery is needed to fix complex spinal injuries. It includes procedures to stabilize the spine, relieve pressure on the spinal cord, and help patients recover.
Cervical Spine Stabilization
Cervical spine stabilization is key for neck injuries. It uses different methods to keep the spine stable and protect the spinal cord. Anterior cervical discectomy and fusion (ACDF) is a common method. It removes damaged discs and fuses the vertebrae.
Thoracolumbar Fracture Management
Thoracolumbar fractures are common in spinal trauma. They need careful management to check the spine’s stability. Minimally invasive surgical techniques are used to treat these fractures. They offer quick recovery and less damage to tissues.
| Treatment Approach | Description | Benefits |
| Conservative Management | Non-surgical treatment using bracing and physical therapy | Avoids surgical risks, suitable for stable fractures |
| Surgical Stabilization | Surgical procedure to stabilize the spine | Provides immediate stability, allows for early mobilization |
| Minimally Invasive Surgery | Less invasive surgical techniques to reduce tissue damage | Less blood loss, quicker recovery, reduced risk of complications |
Decompression Procedures for Spinal Cord Injury
Decompression procedures are vital for spinal cord injuries. They relieve pressure on the spinal cord. Spinal cord decompression uses surgery to remove the cause of compression and improve spinal cord function.
Minimally Invasive Approaches to Spinal Trauma
Minimally invasive surgery is becoming more popular in spinal trauma. It uses smaller incisions and causes less tissue damage. This leads to less pain and faster recovery.
Managing spinal trauma needs a team effort. It involves the latest surgical methods and technology to improve patient results.
Maxillofacial and Neck Trauma Surgery
Trauma to the maxillofacial region and neck is complex. It needs special surgical techniques. The goal is to fix both function and looks.
Facial Fracture Repair Techniques
Fixing facial fractures is key in maxillofacial surgery. Maxillofacial surgeons use many methods to fix facial bones. Miniplates and microplates help fix fractures better and more precisely.
The right method depends on the fracture’s location and how bad it is. For example, fixing the zygomatic complex often needs a mix of methods to align and fix it right.
Mandibular and Maxillary Reconstruction
Rebuilding the mandible and maxilla is vital when trauma causes big bone loss. Reconstruction plates and bone grafts help fix these bones. They make sure the bones work right again.
3D printing and virtual planning have made these surgeries better. Surgeons can plan and make custom implants before surgery. This makes the surgery more precise.
Vascular and Airway Management in Neck Trauma
Neck trauma is risky for blood vessels and the airway. Airway management is the top priority. It’s critical to keep the airway open to save lives. Sometimes, endotracheal intubation or cricothyrotomy is needed.
Fixing neck vascular injuries is urgent. Tourniquets and vascular clamps help stop bleeding until the injury is fixed.
Wound Management and Soft Tissue Procedures
In trauma surgery, managing wounds is complex. It involves debridement, wound closure, and advanced methods like tissue flaps and negative pressure therapy. Good wound care is key to avoid infections, speed up healing, and reduce long-term harm.
Debridement and Wound Closure Techniques
Debridement removes dead, damaged, or infected tissue to help healthy tissue heal. There are different ways to do this, like surgery, mechanical, enzymatic, or autolytic debridement. The right method depends on the wound and the patient’s health.
Wound closure methods vary based on the wound’s type. Clean wounds might get primary closure, while contaminated wounds might wait. Some wounds are left open to heal on their own.
Skin Grafting and Tissue Flaps
Skin grafting uses healthy skin to cover wounds. It’s great for big wounds. There are split-thickness and full-thickness grafts, each with its own use.
Tissue flaps move a piece of tissue with its blood supply to the wound. They’re for complex wounds needing coverage and to restore function and look.
Fasciotomy for Compartment Syndrome
Fasciotomy is a surgery to relieve muscle compartment pressure. It’s for trauma-caused compartment syndrome, which can harm blood flow and muscle function. The surgery cuts the fascia to release pressure.
Negative Pressure Wound Therapy
Negative pressure wound therapy (NPWT) uses a vacuum dressing to aid healing. It helps by removing fluids, cutting down bacteria, and boosting tissue growth.
| Wound Management Technique | Description | Indications |
| Debridement | Removal of dead or infected tissue | Necrotic or infected wounds |
| Skin Grafting | Transplanting healthy skin | Large surface area wounds |
| Tissue Flaps | Transferring tissue with blood supply | Complex wounds requiring coverage and function restoration |
| Fasciotomy | Relieving pressure in muscle compartments | Compartment syndrome |
| NPWT | Applying vacuum dressing | Chronic or complex wounds |
Emergency Trauma Surgical Techniques and Innovations
The need for prompt and appropriate emergency surgery is significant.
Damage Control Surgery Principles
Damage control surgery (DCS) is a vital method for treating severe injuries. It focuses on quick control of bleeding and contamination. Then, it moves to resuscitation and final repair.
DCS aims to save lives by reducing the initial surgery’s impact. This lowers the chance of complications.
The main parts of DCS are:
- Rapid control of hemorrhage
- Control of contamination
- Resuscitation in the intensive care unit
- Definitive repair in subsequent surgeries
Minimally Invasive Approaches in Trauma
Minimally invasive surgery (MIS) is becoming more common in trauma care. It offers benefits like less tissue damage, less pain, and faster recovery. Techniques like laparoscopy and thoracoscopy help diagnose and treat injuries.
MIS in trauma has many advantages:
- Less invasive, causing less trauma to the patient
- Smaller incisions, leading to less scarring and infection risk
- Quicker recovery, allowing patients to get back to normal activities sooner
Hybrid Operating Rooms and Advanced Imaging
Hybrid operating rooms are changing trauma surgery. They combine traditional ORs with advanced imaging like fluoroscopy and CT scanning.
Hybrid ORs offer many benefits:
- Improved diagnostic accuracy
- Enhanced surgical precision
- Reduced need for reoperation
Technological Advancements in Trauma Surgery
Technology is greatly improving trauma care. Innovations like 3D printing, robotic surgery, and advanced hemostatic agents are leading to better outcomes.
Some key technological advancements are:
- 3D printing for preoperative planning and patient education
- Robotic-assisted surgery for precision and minimal invasiveness
- Advanced hemostatic agents for controlling bleeding
Post-Trauma Surgical Care and Rehabilitation
Recovering from trauma surgery takes a lot of work. It includes care in intensive units, more surgeries, and rehab. Good care is key to a smooth recovery and avoiding problems.
Intensive Care Management After Major Trauma
Intensive care is vital after trauma. It helps keep the patient stable and manages serious injuries. Close monitoring and quick action are key in the first days after surgery. A team of doctors, nurses, and specialists work together to meet the patient’s needs.
Patients might need help breathing and keeping their heart rate stable. Starting to move and rehab early in the ICU helps prevent problems like blood clots and muscle loss.
Secondary and Reconstructive Procedures
After getting stable, patients might need more surgeries. These fix ongoing injury issues. Reconstructive surgery aims to repair tissues, restore function, and improve looks. The timing and type of surgery depend on the patient’s health and injuries.
These surgeries can include skin grafts, tendon repairs, or fixing bones. Doctors plan these surgeries carefully, based on the patient’s needs and what will help the most.
Multidisciplinary Approach to Complex Trauma
Managing complex trauma needs a team effort. Specialists from different fields work together. They create a care plan that fits the patient’s needs.
This team looks at the patient’s physical, mental, and social health. A holistic approach helps the patient recover better and feel better overall.
Long-term Rehabilitation Strategies
Rehab is key for long-term recovery. It helps patients regain function, improve life quality, and get back to daily life. Rehab programs are made just for each patient, using physical and occupational therapy as needed.
Good rehab means keeping the treatment plan up to date. The goal is to help patients be independent and happy, and to fit back into their community.
Conclusion
Trauma surgery is key in emergency care, saving lives and preventing disabilities. New techniques, imaging, and rehab have made a big difference. This has improved how well trauma patients do.
The need for prompt and appropriate emergency surgery is significant.
Rehab is also vital for recovery. It helps patients get back to normal and join their communities again. Knowing trauma surgery well helps doctors give the best care to trauma patients.
FAQ
What is trauma surgery, and why is it important?
Trauma surgery treats injuries from accidents. It’s key in emergency care. Quick and right surgery can save lives and prevent lasting harm.
What are the different types of trauma surgeries?
Trauma surgeries include many types. These are orthopedic, abdominal, neurosurgical, thoracic, spinal, maxillofacial, and wound management.
What is the role of trauma centers in providing specialized care?
Trauma centers offer specialized care for injury patients. They are ranked from Level I to Level IV, with Level I being the top.
How are trauma patients evaluated and prepared for surgery?
First, patients are assessed and triaged. Then, imaging is used to see the injury’s extent. Next, they are prepared for surgery by stabilizing their vital signs.
What are some common techniques used in orthopedic trauma surgery?
Orthopedic surgery includes fixing fractures, reconstructing joints, and amputations. These help patients recover.
What is damage control surgery, and when is it used?
Damage control surgery is used in emergencies. It stops bleeding and contamination. The goal is to stabilize the patient before fixing the injury.
How are traumatic brain injuries managed surgically?
Brain injuries are treated with surgeries like craniotomy and intracranial pressure monitoring. They also repair skull fractures and hematomas.
What are some common surgical techniques used in thoracic trauma?
Thoracic surgery includes inserting chest tubes and emergency thoracotomy. It also fixes heart and great vessel injuries.
How are spinal injuries managed surgically?
Spinal injuries are treated with surgeries like cervical spine stabilization and thoracolumbar fracture management. Decompression procedures relieve spinal cord pressure.
What is the importance of post-trauma surgical care and rehabilitation?
Post-surgery care and rehabilitation are vital. They include intensive care, secondary procedures, and long-term rehabilitation. This helps patients recover fully.
What are some emerging trends and innovations in trauma surgery?
New trends include minimally invasive surgery and hybrid operating rooms. Advanced imaging technologies are also being used.
How does socioeconomic status impact trauma surgery outcomes?
Socioeconomic status affects outcomes. Disparities in care and resources can harm patient results.
What is the role of a multidisciplinary approach in complex trauma care?
A team approach is key in complex trauma care. It involves many specialties working together for patient care.
References
National Center for Biotechnology Information. Trauma surgery overview orthopedic focus. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7388795/