Last Updated on December 1, 2025 by Bilal Hasdemir
Getting a diagnosis of brain metastases can change your life. It brings a lot of uncertainty about what’s next. Recent numbers show more people with brain metastases than before.
Dealing with life expectancy and prognosis can feel overwhelming. But, new treatments like targeted therapies and immunotherapy are helping. They offer hope for better outcomes.
Key Takeaways
- Understanding the prognosis of brain metastases is key for patients and their families.
- New treatments have improved life expectancy.
- Targeted therapies and immunotherapy are showing great promise.
- Every patient’s case is different, needing tailored care.
- Keeping up with the latest treatments can greatly improve patient results.
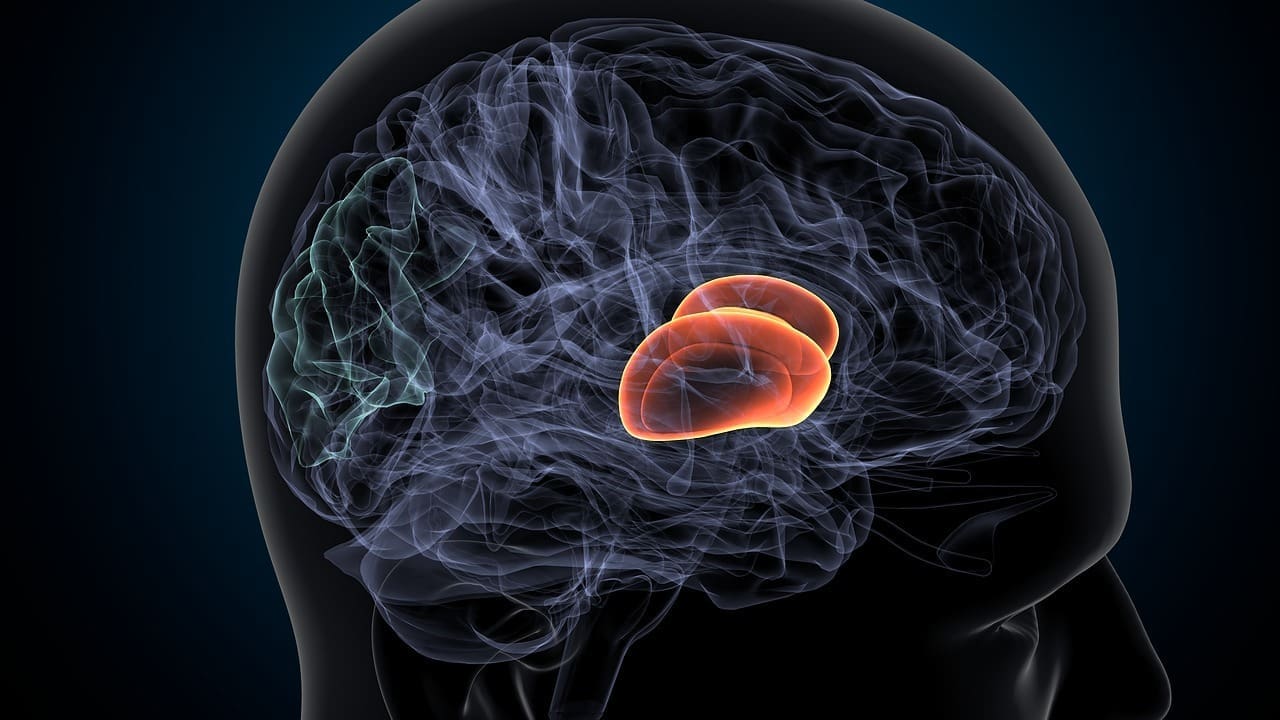
What Are Brain Metastases and How They Develop
Brain metastases happen when cancer cells break off from a main tumor. They travel through the blood or lymphatic system. Then, they form new tumors in the brain.
This process is complex. It involves several steps. These include invasion, circulation, and colonization of cancer cells in the brain tissue.
Definition and Mechanism of Brain Metastases
Brain metastases are secondary brain tumors. They come from cancer cells that have spread from a primary site elsewhere in the body. The mechanism involves cancer cells detaching from the primary tumor.
They survive in the circulatory system. Then, they adhere to and invade the blood-brain barrier. This allows them to establish new growths in the brain.
The process of metastasis to the brain is not random. Certain primary cancers are more likely to metastasize to the brain. Understanding this mechanism is key for developing effective treatment strategies.
Common Primary Cancers that Metastasize to the Brain
Several primary cancers are known to frequently metastasize to the brain. These include:
- Lung cancer
- Breast cancer
- Melanoma
- Colorectal cancer
- Renal cell carcinoma
The frequency and pattern of brain metastasis vary among these primary cancers. For example, lung cancer and melanoma have a high tendency to spread to the brain.
Primary Cancer Type | Frequency of Brain Metastasis |
Lung Cancer | High |
Breast Cancer | Moderate to High |
Melanoma | High |
Colorectal Cancer | Low to Moderate |
Knowing the primary cancer type is key for managing brain metastases. It affects treatment decisions and prognosis.
Brain Metastases Survival: General Prognosis Overview
Knowing the prognosis for brain metastases patients is key for making treatment choices. The outlook varies based on several factors. These include the type of primary cancer, the number and location of brain metastases, and the patient’s health.
Median survival timeframes without treatment
Without treatment, the survival time for brain metastases patients is short. Studies show that without treatment, the median survival is about 1 to 3 months. This is due to the disease’s progression and neurological complications.
Overall survival ranges with modern treatments
Modern treatments have greatly improved survival chances for brain metastases patients. The overall survival range can be from 3 to 18 months or more. This depends on the treatments used, like surgery, radiation, and systemic therapy.
Recent studies show better survival rates thanks to new treatments. For example, patients getting stereotactic radiosurgery (SRS) or whole-brain radiation therapy (WBRT) live longer than those without these treatments.
Treatment Modality | Median Survival (months) | Overall Survival Range (months) |
No Treatment | 1-3 | N/A |
SRS | 9-12 | 6-18 |
WBRT | 3-6 | 2-12 |
Combined Modality | 12-18 | 6-25+ |
Historical trends in survival rates
Survival rates for brain metastases patients have improved over time. This is thanks to better diagnostic tools, surgery, radiation, and treatments. Historical data show a big shift from a few months to over a year or more in some cases.
As treatments keep getting better, knowing these trends is vital. It helps us understand the current prognosis and future improvements in survival rates.
Survival Rates Based on Primary Cancer Type
The type of cancer a person has greatly affects their chances of survival with brain metastases. Knowing these differences is key for planning treatment and understanding a patient’s outlook.
Lung Cancer Brain Metastases
Lung cancer is a top cause of brain metastases, with survival times ranging from 1 to 18 months. Non-small cell lung cancer (NSCLC) often has a better outlook than small cell lung cancer (SCLC). New treatments targeting specific genetic changes have helped some patients.
Breast Cancer Brain Metastases
Breast cancer brain metastases usually last from 2 to 25 months. Hormone receptor-positive breast cancer tends to do better than triple-negative breast cancer. New treatments, including targeted and immunotherapy, are showing promise for some patients.
Melanoma Brain Metastases
Melanoma brain metastases typically last from 3 to 13 months. The discovery of BRAF mutations has led to targeted therapies that help some patients. Immunotherapy is also showing great promise in treating melanoma brain metastases.
Colorectal Cancer Brain Metastases
Colorectal cancer brain metastases usually have a poor prognosis, lasting from 3 to 12 months. But, isolated brain metastases that can be treated locally may have a better chance. Researchers are working on new treatments to improve survival rates.
These survival ranges show why it’s important to consider the primary cancer type when predicting outcomes for brain metastasis patients. Ongoing research and new treatments are changing how we manage brain metastases.
Critical Factors That Determine Survival Length
Several key factors determine how long patients with brain metastases can live. These factors fall into two main categories: patient-related and disease-related. Both are important in predicting how long a patient might live.
Patient-related Factors
Factors related to the patient greatly affect survival time. These include:
- Performance Status: A patient’s health and ability to function, measured by scales like the Karnofsky Performance Status (KPS) or the Eastern Cooperative Oncology Group (ECOG) performance status, is a strong survival predictor.
- Age: Younger patients usually have better survival rates than older ones.
- Comorbidities: Having other serious health conditions can make it harder for a patient to handle treatments and can affect survival.
Disease-related Factors
Factors related to the disease also greatly impact survival time. These include:
- Intracranial Burden: The number, size, and location of brain metastases can greatly affect survival. Patients with fewer and smaller metastases tend to do better.
- Extracranial Disease Status: The presence and extent of cancer outside the brain (extracranial disease) can also affect survival. Patients with controlled extracranial disease tend to have better outcomes.
- Primary Cancer Type: The type of primary cancer that has spread to the brain impacts survival. Different cancers have different prognoses and treatment responses.
Understanding these factors helps doctors give more accurate survival predictions. It also helps tailor treatments to meet each patient’s unique needs.
Factor | Description | Impact on Survival |
Performance Status | Overall health and functional status | Higher performance status is associated with better survival |
Age | Patient’s age | Younger age is generally associated with better survival |
Intracranial Burden | Number, size, and location of brain metastases | Lower intracranial burden is associated with better survival |
Extracranial Disease Status | Presence and extent of cancer outside the brain | Controlled extracranial disease is associated with better survival |
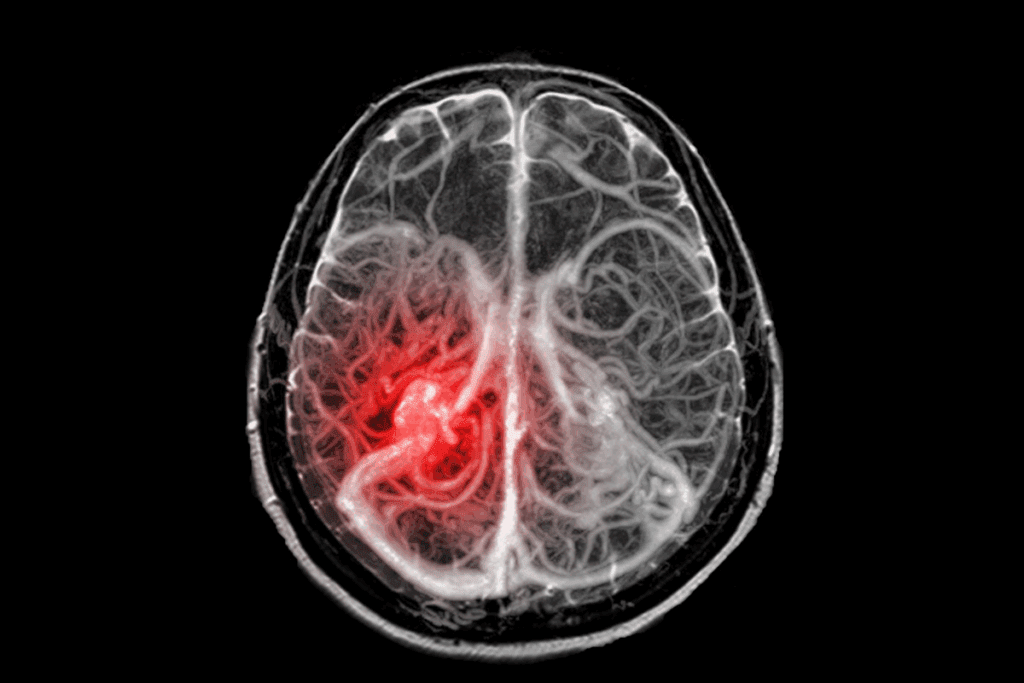
How Extracranial Disease Status Affects Survival Timeline
The spread of cancer outside the brain, known as extracranial disease, greatly affects survival. It’s key to manage this spread to improve chances of living longer.
Controlled vs. Uncontrolled Systemic Disease
Those with controlled systemic disease have a better outlook than those without. Controlled systemic disease means the cancer outside the brain is being kept in check by treatment.
Research shows that those with controlled extracranial disease live longer than those without.
Impact of Limited Extracranial Metastases
Having a few spots of cancer outside the brain can affect survival. Patients with a small number of these spots might have a better chance of survival.
Studies suggest that treating these spots aggressively, along with brain metastases, can improve survival rates.
Survival with Extensive Systemic Disease
Widespread cancer outside the brain, or extensive systemic disease, usually means a worse prognosis.
Patients with this condition often need a more detailed treatment plan. This plan aims to control both brain metastases and the cancer spread.
Extracranial Disease Status | Median Survival Time |
Controlled Systemic Disease | 12-18 months |
Limited Extracranial Metastases | 9-15 months |
Extensive Systemic Disease | 3-6 months |
Prognostic Assessment Tools for Survival Estimation
Estimating survival time for brain metastases patients needs advanced tools. These tools help doctors predict outcomes. This guides treatment and improves care.
Prognostic tools are key in neuro-oncology. They help estimate survival and tailor treatments. We use various indices to understand the factors affecting survival.
Diagnosis-Specific Graded Prognostic Assessment (DS-GPA)
The Diagnosis-Specific Graded Prognostic Assessment (DS-GPA) is a key tool. It has evolved to include specific diagnosis factors. It looks at age, performance status, and more to estimate survival.
The DS-GPA has been updated for different cancers. This makes predictions more accurate for each cancer type.
Recursive Partitioning Analysis (RPA)
Recursive Partitioning Analysis (RPA) is another tool for survival estimation. It sorts patients into groups based on age, performance status, and more.
RPA is used in radiation oncology. It helps tailor treatments based on patient needs and expected outcomes.
Other Prognostic Indices and Calculators
There are other tools like the Graded Prognostic Assessment (GPA) and the Basic Score for Brain Metastases (BS-BM). Nomograms also use clinical and molecular factors.
These tools keep getting better with new data. They help us give more personalized care to brain metastases patients.
Untreated Brain Metastases: Natural History and Timeframes
It’s important for patients and their families to understand how untreated brain metastases progress. When these metastases are not treated, the main goal is to manage symptoms and improve life quality.
Expected Survival Without Intervention
Patients with untreated brain metastases usually live from 1 to 3 months. This time can vary based on the type of primary cancer, the number of metastases, and the patient’s health. It’s vital to discuss treatment options quickly to find the best path forward.
Palliative Care Approaches and Outcomes
Palliative care is key in managing symptoms and improving life quality for those with untreated brain metastases. It aims to ease symptoms and stress, aiming to enhance the patient’s and family’s life. Palliative care teams work closely with patients to meet their unique needs, like pain management and emotional support.
Quality of Life During Untreated Progression
The quality of life for patients with untreated brain metastases can differ greatly. Some may decline quickly, while others may stay stable for a while. Managing symptoms well is essential to maintain a good quality of life. This includes controlling headaches, seizures, and cognitive changes, as well as emotional and psychological support.
We understand the tough journey patients face with brain metastases, whether treated or not. Our goal is to provide care that meets their physical, emotional, and social needs. We aim to support them fully as they navigate this complex situation.
Surgical Resection: Impact on Survival Timeline
Surgical resection has become a key part of treating brain metastases. It offers hope for better survival rates. This treatment involves removing tumors from the brain.
Survival Benefits After Complete Resection
Removing all brain metastases can greatly improve survival. Research shows that complete removal leads to better outcomes. This is because it reduces tumor size and relieves symptoms.
Key survival benefits include:
- Increased overall survival time
- Improved quality of life
- Reduced risk of neurological deterioration
Ideal Candidates for Surgical Intervention
Not every patient with brain metastases is a good candidate for surgery. The decision to have surgery depends on several factors. These include the number, size, and location of tumors, and the patient’s health.
Ideal candidates typically have:
- A single or limited number of brain metastases
- Accessible tumor location
- Controlled or controllable systemic disease
- Good performance status
Post-Surgical Survival Statistics by Cancer Type
Survival rates after surgery differ based on the cancer type. Here’s a look at the statistics:
Cancer Type | Median Survival (months) |
Lung Cancer | 10-14 |
Breast Cancer | 12-18 |
Melanoma | 8-12 |
Recurrence Patterns and Management
Even with successful surgery, tumors can come back. It’s important to understand how and when this happens.
Common recurrence patterns include:
- Local recurrence at the resection site
- Distant brain metastases
- Systemic disease progression
When tumors come back, treatment options vary. They can include more surgery, radiation, or systemic treatments.
Radiation Therapy Outcomes and Survival Benefits
Radiation therapy is key in treating brain metastases. It offers various options based on each patient’s needs. We’ll look at the different radiation therapy methods and how they affect survival rates.
Whole-Brain Radiotherapy Survival Rates
Whole-brain radiotherapy (WBRT) is a common treatment for brain metastases, mainly for those with many lesions. Research shows WBRT can increase survival time, with a median of 3 to 6 months. This treatment is often combined with other therapies to improve patient results.
Stereotactic Radiosurgery Results
Stereotactic radiosurgery (SRS) is a precise radiation therapy that targets specific areas. For patients with a few brain metastases, SRS has shown good results, with a median survival of 6 to 16 months. This method works well for those with oligometastatic disease.
Combined Radiation Approaches
Using different radiation therapy methods together can lead to better patient outcomes. For example, combining SRS with WBRT can improve local control and possibly survival. These combined methods are customized for each patient’s condition and disease extent.
Radiation Necrosis and Management
Radiation necrosis is a complication of radiation therapy, where brain tissue reacts to the radiation. Managing it involves medical treatments and sometimes surgery. Early detection and proper management are key to reducing its impact on quality of life.
Systemic Therapy Impact on Brain Metastases Survival
Systemic therapy is key in fighting brain metastases. It offers new ways to help patients. The fight against brain metastases is complex. It involves many treatments like chemotherapy, targeted therapies, and immunotherapy.
Chemotherapy Effectiveness and Limitations
Chemotherapy is a mainstay in cancer treatment, including brain metastases. But, it faces a big challenge: the blood-brain barrier. This barrier blocks some chemotherapy from reaching the brain.
Despite this, some chemotherapy works well against brain metastases. This is true for cancers like small cell lung cancer and germ cell tumors. The trick is to pick the right chemotherapy for the cancer type and to use it with other treatments.
Key considerations for chemotherapy in brain metastases include:
- Choosing agents with known blood-brain barrier penetration
- Combining chemotherapy with other modalities like radiation therapy
- Monitoring for neurotoxicity and adjusting doses
Targeted Therapies and Survival Extension
Targeted therapies have changed cancer treatment by focusing on specific cancer growth factors. For brain metastases, they offer big benefits, mainly when the cancer has specific molecular drivers.
In non-small cell lung cancer with EGFR mutations or ALK rearrangements, targeted therapies work well against brain metastases. Also, in HER2-positive breast cancer, treatments targeting HER2 can control brain metastases effectively.
Benefits of targeted therapies include:
- Improved efficacy against specific molecular subtypes
- Potential for better blood-brain barrier penetration
- Generally more favorable side effect profile compared to traditional chemotherapy
Immunotherapy Advances and Outcomes
Immunotherapy uses the body’s immune system to fight cancer. It’s a promising treatment for brain metastases. Checkpoint inhibitors, a type of immunotherapy, have shown activity against brain metastases in various cancers, including melanoma and non-small cell lung cancer.
The effectiveness of immunotherapy in brain metastases is being studied. Researchers are looking into combining different treatments and new immunotherapeutic agents. Immunotherapy could lead to long-lasting responses and better survival for patients with brain metastases.
Key aspects of immunotherapy for brain metastases:
- Potential for durable responses and improved survival
- Ongoing research into combination regimens and novel agents
- Importance of patient selection based on tumor characteristics and immune profile
Single vs. Multiple Brain Metastases: Survival Differences
It’s important to know how single versus multiple brain metastases affect survival. The number of metastases plays a big role in treatment choices and how long a patient might live.
Prognosis with Solitary Brain Metastasis
Patients with just one brain metastasis usually have a better chance of survival. Research shows that these patients can live from 11 to 25 months after treatment.
Treatment approaches for one metastasis often include surgery and radiation. This combo can greatly improve survival chances.
Survival with Oligometastatic Disease
Oligometastatic disease means having 2-4 brain metastases. It’s a middle ground between having one or more. Survival times for these patients vary, but usually range from 8 to 15 months.
Aggressive local therapies, like stereotactic radiosurgery (SRS), are used. They aim to extend life and improve quality of life for these patients.
Outcomes with Multiple Lesions
Those with more than four brain metastases face a tougher prognosis. Survival times are generally shorter, from 3 to 6 months. This depends on the cancer type, how well the patient is doing, and if there’s cancer outside the brain.
Whole-brain radiation therapy (WBRT) is often used for multiple metastases. It tries to manage symptoms and improve life quality.
Number of Brain Metastases | Median Survival Time | Common Treatment Approaches |
Solitary | 11-25 months | Surgical resection, SRS |
Oligometastatic (2-4) | 8-15 months | SRS, WBRT |
Multiple (>4) | 3-6 months | WBRT, systemic therapy |
The table above shows survival differences based on metastasis number. It highlights median survival times and common treatments.
Long-term Survivors: Characteristics and Treatment Patterns
Learning about long-term survivors with brain metastases helps us find better ways to treat them. We’ll look at what makes these patients special, the treatments that help them live longer, and how to keep them healthy over time.
Profiles of Patients Surviving Beyond 2 Years
People who live more than two years with brain metastases often share certain traits. They might be younger, have a better health status, less cancer outside the brain, and certain genetic markers.
A study in the Journal of Neuro-Oncology found that these survivors often got aggressive treatments like surgery and radiosurgery. They also noted that some cancers, like breast cancer, tend to do better.
Characteristic | Long-term Survivors (>2 years) | Short-term Survivors ( |
Median Age | 55 years | 62 years |
Primary Tumor Type | Breast Cancer (40%), NSCLC (30%) | NSCLC (50%), Melanoma (20%) |
Treatment Approaches | Surgery + SRS (60%), SRS alone (20%) | WBRT (70%), Palliative Care (20%) |
Treatment Approaches Associated with Extended Survival
Several treatments can help patients with brain metastases live longer. These include surgery and radiosurgery, as well as targeted and immunotherapies for some patients.
A study in the International Journal of Radiation Oncology, Biology, Physics showed that radiosurgery can extend life by 7 months. This is compared to whole-brain radiation therapy.
Maintenance Strategies for Long-term Survivors
For those who live a long time, it’s important to keep them healthy. This includes regular check-ups, ongoing treatments, and help for any brain or cognitive problems.
A study in the Journal of Clinical Oncology stressed the need for a team approach to care. This team should include neuro-oncologists, radiation oncologists, and specialists in rehabilitation.
By understanding what makes long-term survivors tick, we can improve how we treat brain metastases. This can lead to better outcomes for patients.
Quality of Life During Survival Period
Living with brain metastases affects how well someone feels every day. It shapes what treatments they choose and how happy they are. Keeping quality of life high is key when dealing with brain metastases.
Neurocognitive Outcomes with Different Treatments
How treatments for brain metastases affect the brain varies. Surgery and radiation therapy are common, each with its own brain side effects. For example, whole-brain radiation can make some patients forgetful, while stereotactic radiosurgery (SRS) might have fewer side effects.
When picking treatments, we must think about how they affect the brain. New research and techniques aim to lessen these effects, helping patients live better.
Symptom Management Strategies
Managing symptoms is key to a good life with brain metastases. Symptoms like headaches, seizures, and brain fog are common. Medications, like corticosteroids, help reduce swelling and headaches.
- Seizure management through antiepileptic drugs
- Cognitive rehabilitation to address memory and concentration issues
- Pain management strategies, including medication and alternative therapies
By tackling symptoms early, we can greatly improve a patient’s life quality.
Supportive Care Approaches
Supportive care is vital for brain metastases management. It includes palliative care, which helps ease symptoms and stress of serious illnesses.
Supportive Care Approach | Description | Benefits |
Palliative Care | Relief from symptoms and stress | Improved quality of life, symptom management |
Cognitive Rehabilitation | Addressing cognitive difficulties | Enhanced cognitive function, independence |
Psychological Support | Counseling and emotional support | Reduced anxiety and depression, improved coping |
Balancing Survival Extension with Quality of Life
Choosing treatments for brain metastases is a tough decision. It’s about extending life versus keeping quality of life high. Decisions must weigh life extension against daily living impact.
By carefully choosing treatments and adding supportive care, we aim for the best balance. This ensures patients get care that meets their unique needs.
Recent Advances Improving Brain Metastases Survival Rates
The field of treating brain metastases is changing fast. New treatments are showing great promise. Researchers are finding new ways to fight metastatic disease, leading to better patient results.
Novel Therapeutic Approaches
In recent years, new treatments have been developed. These novel therapeutic approaches target specific parts of brain metastases. They include:
- Targeted therapies that attack specific genetic mutations in tumor cells
- Immunotherapies that use the immune system to fight cancer
- Combination regimens that mix different treatments for better results
These new methods are not just making patients live longer. They’re also making their lives better while they’re fighting cancer.
Blood-Brain Barrier Penetrating Agents
One big challenge in treating brain metastases is the blood-brain barrier (BBB). It blocks many treatments from reaching the brain. Now, scientists are working on blood-brain barrier penetrating agents to get around this problem.
These agents aim to:
- Get past the BBB more easily
- Bring more of the treatment to the tumor
- Help patients get better results from treatment
Personalized Medicine Strategies
The age of personalized medicine is changing how we treat brain metastases. Doctors can now tailor treatments based on each tumor’s genetic makeup.
This method leads to:
- More accurate targeting of tumor cells
- Fewer side effects for patients
- Better treatment results
Promising Clinical Trials and Emerging Data
Clinical trials are giving us new insights into treating brain metastases. The data from these studies are helping shape treatment plans and guide doctors.
Some exciting areas of research include:
- Combination therapies that mix different treatments
- New radiation methods that protect the brain
- Advanced surgery techniques for better tumor removal
As these advancements keep coming, we expect to see even better survival rates and outcomes for patients with brain metastases.
Discussing Prognosis: Understanding Your Specific Timeline
Understanding your prognosis is key when dealing with brain metastases. Your healthcare team can guide you through your situation. They help you make informed decisions about your care.
Interpreting Survival Statistics for Individual Cases
Survival statistics give a general idea of prognosis. But, individual outcomes can vary a lot. Consider your cancer type, brain metastases number and location, and overall health when looking at these statistics.
For example, survival times can range from a few months to several years. This depends on the cancer type and treatment. It’s important to talk to your healthcare provider about how these statistics apply to you.
Key Questions to Ask Your Healthcare Team
To understand your prognosis better, ask the right questions. Here are some:
- What is my overall prognosis based on my current condition?
- How does the type and stage of my primary cancer affect my brain metastases prognosis?
- What treatment options are available, and how might they impact my survival and quality of life?
- Are there any clinical trials or new treatments that might be suitable for me?
Making Informed Treatment Decisions
Understanding your prognosis and treatment options is key. Your healthcare team can guide you. They consider your condition and health to suggest the best treatments.
Think about the benefits and risks of each treatment. Also, consider how it will affect your quality of life. It’s important to talk about your personal preferences and values with your healthcare team. This ensures your treatment plan meets your goals.
Planning for Various Outcomes
Planning for different outcomes is important when managing brain metastases. Discuss advance care planning with your loved ones and healthcare team. This includes living wills and durable power of attorney for healthcare.
It’s also vital to talk about symptom management and supportive care. Your healthcare team can help with managing symptoms and accessing supportive care services. This ensures the best quality of life.
Prognostic Factor | Description | Impact on Survival |
Primary Cancer Type | Type of original cancer | Varies significantly by cancer type |
Number of Brain Metastases | Number of metastases in the brain | More metastases generally indicate poorer prognosis |
Performance Status | Patient’s overall health and functionality | Better performance status is associated with longer survival |
Conclusion
Knowing about brain metastases survival rates is key for patients and their families. We’ve looked at how survival changes based on several factors. These include the type of primary cancer, if there’s disease outside the brain, and the treatments available.
Survival times can vary a lot, from a few months to years with the right treatment. Effective treatments like surgery, radiation, and systemic therapy can help. They can also improve how well a person lives with the disease.
Tools for predicting survival help patients and doctors make better plans. New treatments and personalized care are being developed. This gives hope to those facing brain metastases.
Understanding brain metastases and treatment options helps patients make informed choices. It’s vital to talk about prognosis and treatment goals with doctors. This way, patients can get the best care and quality of life.
FAQ
What are brain metastases and how do they develop?
Brain metastases are tumors that start in the brain from cancer cells that spread from other parts of the body. These cells break away, travel through the bloodstream or lymphatic system, and settle in the brain. There, they grow and form new tumors.
Which primary cancers are most likely to metastasize to the brain?
Lung cancer, breast cancer, melanoma, and colorectal cancer are most likely to spread to the brain. Their aggressiveness and specific molecular markers play a role in this.
What is the general prognosis for patients with brain metastases?
The prognosis for patients with brain metastases varies. It depends on the type of cancer, the number and location of brain tumors, and if the cancer has spread elsewhere. Survival times can range from a few months to several years, with some patients living longer.
How does the primary cancer type affect survival rates in brain metastases patients?
The type of cancer affects survival rates. For example, lung cancer brain metastases have a median survival of 1-18 months. Breast cancer brain metastases have a range of 2-25 months. Melanoma and colorectal cancer brain metastases have median survival ranges of 3-13 months and 3-12 months, respectively.
What are the critical factors that determine survival length in brain metastases patients?
Survival length is determined by patient and disease factors. These include the patient’s performance status and age, and the number, location, and presence of brain tumors, as well as the primary cancer type.
How does extracranial disease status affect the survival timeline of brain metastases patients?
The status of extracranial disease greatly affects survival. Patients with controlled systemic disease tend to live longer than those with uncontrolled or extensive disease.
What are the prognostic assessment tools used to estimate survival in brain metastases patients?
Tools like the Diagnosis-Specific Graded Prognostic Assessment (DS-GPA) and Recursive Partitioning Analysis (RPA) are used. They help estimate survival based on patient and disease characteristics.
What is the natural history of untreated brain metastases?
Untreated brain metastases progress quickly and have short survival times, usually 1-3 months. Palliative care can help manage symptoms and improve quality of life.
How does surgical resection impact the survival timeline of brain metastases patients?
Surgical resection can significantly improve survival for selected patients, like those with single or oligometastatic disease. Survival benefits vary based on the primary cancer type and other factors.
What are the outcomes and survival benefits of different radiation therapy approaches for brain metastases?
Radiation therapy, including whole-brain radiotherapy and stereotactic radiosurgery, can improve survival. Benefits vary based on the number and location of brain metastases and the primary cancer type.
How do systemic therapies, such as chemotherapy and targeted therapies, impact the survival of brain metastases patients?
Systemic therapies, like chemotherapy, targeted therapies, and immunotherapy, can improve survival. They are most effective in patients with specific molecular markers or tumor characteristics.
What is the difference in survival between patients with single, oligometastatic, and multiple brain metastases?
Patients with single brain metastases generally have better survival outcomes than those with multiple metastases. Oligometastatic disease falls in between in terms of survival prognosis.
What are the characteristics and treatment patterns of long-term survivors with brain metastases?
Long-term survivors often have controlled systemic disease, limited intracranial burden, and favorable primary cancer type. Treatment approaches include surgical resection, radiation therapy, and systemic therapies.
How can patients with brain metastases maintain quality of life during the survival period?
Patients can maintain quality of life by managing symptoms, preserving neurocognitive function, and receiving supportive care. Balancing survival extension with quality of life is key.
What are the recent advances improving brain metastases survival rates?
Advances include novel therapeutic approaches, such as blood-brain barrier penetrating agents, personalized medicine strategies, and emerging clinical trial data.
How can patients understand and discuss their prognosis with their healthcare team?
Patients can understand and discuss their prognosis by interpreting survival statistics, asking questions, and making informed treatment decisions. Planning for various outcomes is also essential.
National Center for Biotechnology Information. Brain Metastases Prognosis and Treatment Advancements. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5737512/