Last Updated on December 2, 2025 by Bilal Hasdemir
Many people have bowel surgery every year. Bowel resection is a common surgery. It removes a part of the intestine that is damaged or sick.Detailed guide on how bowel resection done is performed, covering both open and laparoscopic surgical techniques.
The bowel resection operation helps with many issues. These include bowel obstruction, cancer, and inflammatory bowel disease. Knowing the bowel resection procedure steps helps patients get ready for surgery and recovery.
Key Takeaways
- Bowel resection is a surgical procedure that involves removing a portion of the intestine.
- The surgery is performed to treat various conditions, including bowel obstruction and cancer.
- Understanding the bowel resection procedure steps can help patients prepare for the surgery.
- The bowel resection operation is a significant procedure that requires careful consideration.
- Patients should discuss their options with a healthcare professional to determine the best course of treatment.
Understanding Bowel Resection Surgery
Bowel resection surgery removes a damaged or diseased part of the intestine and is often a lifesaving procedure. It treats conditions in the small or large intestine.
Definition and Purpose
This surgery aims to remove the diseased or damaged part of the intestine, primarily to restore its normal function. It can be done on the small or large intestine, based on the disease’s location and type.
The colon surgery technique varies. Surgeons might use open surgery or laparoscopic or robotic-assisted methods. The choice depends on the patient’s health, disease extent, and surgeon’s skill.
Common Conditions Requiring Bowel Resection
Several conditions may need bowel resection surgery. These include:
- Colorectal Cancer: It’s a main treatment for colorectal cancer, aiming to remove the cancerous part.
- Inflammatory Bowel Disease (IBD): Bowel resection is needed if Crohn’s disease or ulcerative colitis can’t be controlled by medicine or if complications happen.
- Diverticulitis: If diverticulitis is complicated, with recurring inflammation or complications like abscesses or perforations, surgery might be needed.
- Intestinal Obstruction: Surgery may be done to relieve an obstruction caused by scar tissue, tumors, or other factors.
It’s important to know about the intestinal resection method and when bowel resection surgery is needed. Deciding to have this surgery is a big choice. It’s made after tests and talking to healthcare providers.
The bowel surgery steps include careful planning and precise surgery. Good post-operative care is also key for the best results.
Types of Bowel Resection Procedures

Bowel resection procedures differ based on where and how much of the gut is affected. The surgical method used greatly affects the patient’s outcome and recovery.
Small Intestine Resection
Small intestine resection, or small bowel resection, is for diseased or damaged parts of the small intestine. It can be done through open surgery or laparoscopic methods. The choice depends on the patient’s health and the surgeon’s expertise.
The main steps in small intestine resection are:
- Identifying the diseased segment of the small intestine
- Removing the affected portion
- Reconnecting the remaining healthy sections
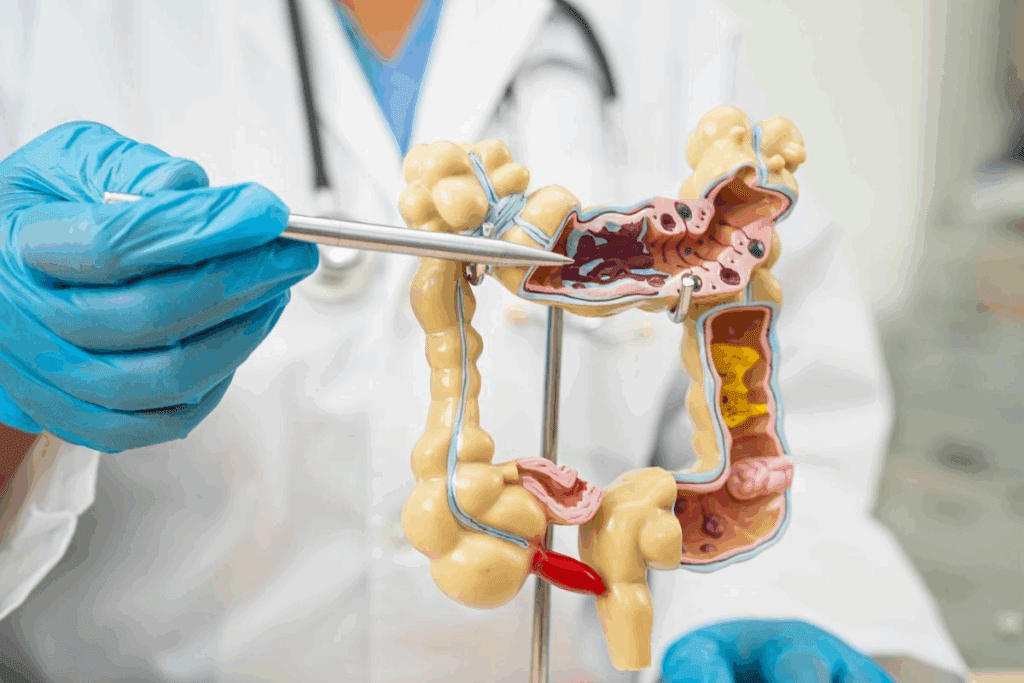
Large Intestine (Colon) Resection
Large intestine or colon resection, known as colectomy, involves removing a part or the whole colon. It’s often done for colorectal cancer, diverticulitis, and inflammatory bowel disease.
The colectomy surgical technique can be:
- Open colectomy
- Laparoscopic colectomy
- Robotic-assisted colectomy
Rectal Resection
Rectal resection removes part or all of the rectum. It’s mainly for rectal cancer or severe rectal disease. The surgery can be complex, using open bowel surgery or laparoscopic bowel resection.
Important aspects of rectal resection include:
- Preserving the anal sphincter function when possible
- Reconstructing the rectum or creating an ostomy if necessary
- Ensuring adequate removal of the diseased tissue
Medical Indications for Bowel Resection
Some gastrointestinal conditions need bowel resection to improve health and reduce symptoms. This surgery removes a part of the intestine that’s sick or damaged. Doctors usually try other treatments first before deciding on surgery.
Colorectal Cancer
Colorectal cancer often means a bowel resection is needed. If cancer is found in the colon or rectum, removing the affected area is key. This helps get rid of the cancer and keeps the intestine working right. Early detection makes bowel resection surgery for colorectal cancer more effective.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) can badly damage the intestines. If medicine doesn’t work or if problems happen, surgery might be needed. The goal is to take out the sick part of the intestine and make life better for the patient.
Diverticulitis
Diverticulitis happens when small pouches in the colon get inflamed. If it’s severe or keeps coming back, surgery might be the best choice. The surgery removes the bad part of the colon.
Other Conditions
Other reasons for bowel resection include intestinal blockage, not enough blood flow to the intestine, and certain hernias. The surgery’s type and how much is removed depends on the condition and the patient’s health.
| Condition | Description | Surgical Approach |
| Colorectal Cancer | Cancer in the colon or rectum | Removal of the cancerous segment |
| Inflammatory Bowel Disease | Chronic inflammation of the intestines | Removal of the diseased portion |
| Diverticulitis | Inflammation of diverticula in the colon | Removal of the affected colon segment |
In conclusion, bowel resection is a key surgery for many gut problems. Knowing why it’s needed and how it’s done is important for both patients and doctors.
Pre-Surgical Evaluation and Testing
The pre-surgical evaluation is key in getting patients ready for intestinal surgery procedures. It helps doctors spot risks and plan to avoid them. This ensures patients get the best care during bowel resection.
Physical Examination
A detailed physical examination is vital. Doctors check the patient’s health and look for signs of illness. They check nutrition, abdominal tenderness, and heart and lung health.
Laboratory Tests
Laboratory tests give more detailed health info. Tests include:
- Blood work to check overall health and find hidden conditions
- Urine tests for infections or other problems
- Coagulation studies to see bleeding risk during surgery
These tests help doctors understand the patient’s health and plan their care.
Imaging Studies
Imaging studies are also key. They give detailed images of the bowel and tissues. Common ones are:
- Computed Tomography (CT) scans to see the bowel and find abnormalities
- Magnetic Resonance Imaging (MRI) to see disease extent and plan surgery
- X-rays to check the bowel for obstructions or issues
These studies help surgeons choose the best colon resection technique and prepare for surgery challenges.
Doctors use physical exams, lab tests, and imaging to understand the patient’s condition. They create a personalized plan for bowel surgery steps. This careful evaluation is critical for the best outcomes in bowel resection.
Preparing for Bowel Resection Surgery
Bowel resection surgery needs careful preparation. This includes changing your diet, cleaning your bowel, and managing your medications. Getting ready right is key for a good surgery and recovery.
Dietary Restrictions
Before surgery, you might need to eat a certain way. You might have to eat a low-fiber diet or a liquid diet. This helps keep your bowel clean. The exact diet depends on your surgeon and your health.
Sticking to the diet helps avoid surgery problems. You should also not eat or drink anything for a while before surgery, as your doctor tells you.
Bowel Preparation
Cleaning your bowel is a big part of getting ready for surgery. It removes waste to lower infection risks during and after surgery.
You might use laxatives or enemas for this. Always follow your surgeon’s or doctor’s exact instructions on how to prepare your bowel.
Medications Management
Managing your medications is important before surgery. Some medicines, like blood thinners, might need to be stopped to avoid bleeding.
Tell your doctor about all your medicines, including prescription and over-the-counter ones, and supplements. They will tell you which ones to keep taking or stop before surgery.
By following the pre-surgery advice on diet, bowel prep, and meds, you help make your surgery and recovery better.
Anesthesia for Bowel Resection
Anesthesia is key in bowel resection surgery. It makes sure patients are comfortable during open bowel surgery, laparoscopic bowel resection, or robotic bowel resection. This helps in achieving better surgical results.
Types of Anesthesia Used
General anesthesia is the main choice for bowel resection surgery. It makes the patient sleep and feel no pain during the surgery. Sometimes, regional anesthesia is added to help with pain after the surgery.
- General Anesthesia: This is the most common type of anesthesia used for bowel resection surgery, ensuring the patient is completely asleep and pain-free during the operation.
- Regional Anesthesia: Techniques such as epidural anesthesia may be used to numb a specific region of the body, reducing pain after surgery.
Anesthesia Risks and Considerations
Anesthesia is usually safe, but there are risks. These include allergic reactions, breathing problems, and nausea and vomiting after surgery.
- Allergic Reactions: Though rare, allergic reactions to anesthesia can occur. Patients should inform their anesthesiologist about any known allergies.
- Respiratory Complications: Anesthesia can affect breathing, and in some cases, may lead to respiratory complications, even in patients with no breathing issues.
- Post-Operative Nausea and Vomiting: This is a common side effect of anesthesia. Medications can be given to help manage these symptoms.
It’s vital for patients to talk about their health and any worries with their anesthesiologist before surgery. This way, the anesthesia plan fits their needs, reducing risks and improving results.
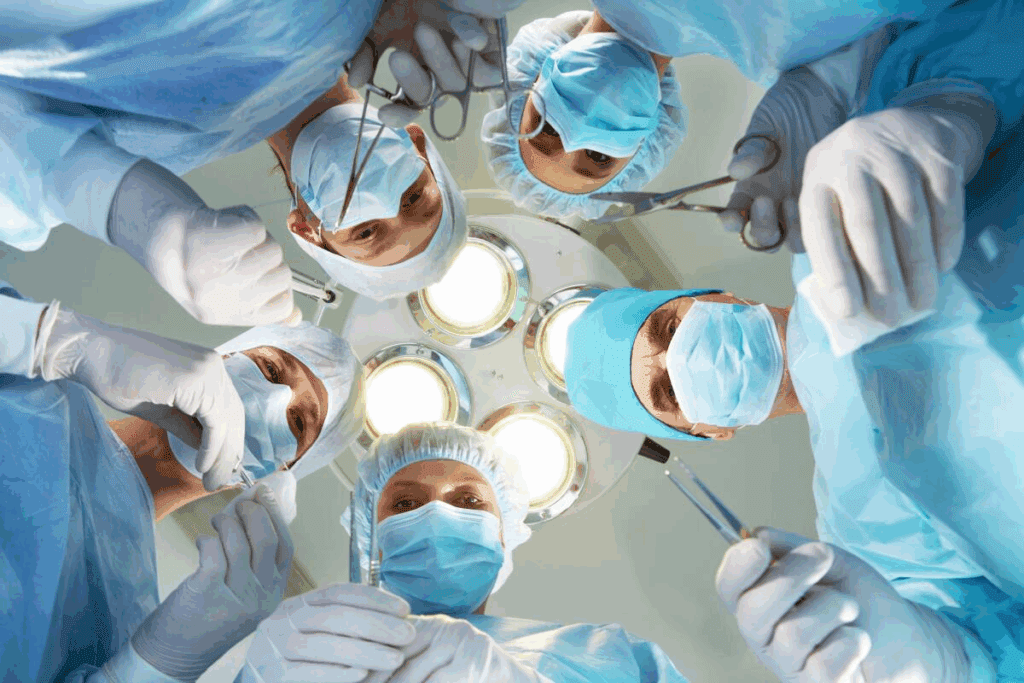
How Bowel Resection is Done: Surgical Approaches
Bowel resection can be done in different ways, like open, laparoscopic, and robotic-assisted surgery. The choice depends on the patient’s health, the condition being treated, and the surgeon’s skills.
Open Bowel Surgery Technique
Open bowel surgery uses a big incision in the abdomen. It’s a traditional method that lets surgeons see and work on the bowel directly. It’s often used for complex cases or when the disease is widespread. The size of the incision depends on the surgery and the patient’s body.
Laparoscopic Bowel Resection Method
Laparoscopic bowel resection is a minimally invasive technique. It uses small incisions in the abdomen. A laparoscope and instruments are inserted through these small openings. This method leads to faster recovery and less pain compared to open surgery. Laparoscopic surgery is good for many patients and results in fewer complications and a shorter hospital stay.
Robotic-Assisted Bowel Surgery
Robotic-assisted bowel surgery uses a robotic system to help surgeons. It offers high-definition 3D visualization and precise tools. Robotic-assisted surgery can improve precision and flexibility, leading to better results for some patients. It’s great for complex procedures and those needing precise work.
The choice between open, laparoscopic, and robotic-assisted surgery depends on many factors. These include the patient’s condition, the surgeon’s experience, and the surgery’s needs. Each method has its benefits and is chosen based on what’s best for the patient’s recovery and outcome.
Step-by-Step Process of How Bowel Resection is Done
It’s important for patients and doctors to know how bowel resection works. This surgery has many steps, from the first cut to joining the healthy parts back together.
Initial Incision and Access
The first thing done is making a cut to get into the belly. The size of the cut varies based on the surgery type. Open surgery needs a big cut, while laparoscopic and robotic surgeries use smaller ones.
Identification and Isolation of Diseased Segment
After getting inside, the surgeon finds the bad part of the bowel. They might use special images to help. Then, they separate it from the rest to keep it clean and ready for removal.
Removal of the Affected Bowel Section
The surgeon then carefully cuts out the bad part. How much they take out depends on the problem, like cancer or inflammation. They aim to get rid of the bad part and keep as much good bowel as they can.
Anastomosis Techniques
Next, the surgeon joins the good parts of the bowel back together. They can use stitches or staples, depending on where it is and the patient’s situation.
Here’s a quick guide to bowel resection surgery:
| Step | Description | Considerations |
| Initial Incision | Access to the abdominal cavity | Type of incision depends on surgical approach |
| Diseased Segment Identification | Locating the affected bowel section | Use of intraoperative imaging |
| Bowel Section Removal | Dissection and removal of diseased bowel | Extent of resection based on underlying condition |
| Anastomosis | Reconnection of healthy bowel sections | Technique choice (hand-sewn vs. stapled) |
Bowel resection surgery is very detailed and complex. It needs careful planning and skill. By following these steps, surgeons can help patients recover well.
Minimally Invasive Bowel Surgery Techniques
Minimally invasive bowel surgery has changed the way we treat colon problems. It offers patients a gentler option than old-school surgery. This new method uses tiny cuts, leading to less pain, smaller scars, and a quicker recovery.
Advantages of Minimally Invasive Approaches
These new surgery methods, like laparoscopic and robotic-assisted, bring many benefits. They are better than traditional surgery in many ways. Here are some of the key advantages:
- Less post-operative pain
- Shorter hospital stays
- Reduced risk of infection
- Smaller scars
- Quicker return to normal activities
Single-Incision Laparoscopic Surgery
Single-incision laparoscopic surgery (SILS) is a method that uses just one cut, usually in the belly button. This approach makes scars smaller and can speed up healing.
Benefits of SILS include:
- Improved cosmetic outcomes due to reduced visible scarring
- Potential for less post-operative pain
- Faster recovery
Natural Orifice Transluminal Endoscopic Surgery
Natural Orifice Transluminal Endoscopic Surgery (NOTES) is a cutting-edge method. It does the surgery through natural openings like the mouth or vagina, without any outside cuts. It’s a new area of research with promising benefits.
The possible advantages of NOTES are:
- No external scarring
- Reduced risk of infection
- Potential for less post-operative pain
Let’s compare these techniques to see their differences:
| Surgical Technique | Number of Incisions | Scarring | Recovery Time |
| Traditional Open Surgery | 1 large incision | Significant scarring | Longer recovery |
| Laparoscopic Surgery | Multiple small incisions | Minimal scarring | Moderate recovery |
| Single-Incision Laparoscopic Surgery | 1 small incision | Minimal scarring | Faster recovery |
| Natural Orifice Transluminal Endoscopic Surgery | No external incisions | No external scarring | Potential for rapid recovery |
Temporary and Permanent Ostomies
In some cases, bowel resection surgery involves creating an ostomy. An ostomy is a surgical opening created in the abdomen for waste elimination, serving as a crucial treatment component for many patients.
When an Ostomy is Necessary
An ostomy might be needed if the surgeon wants to divert waste. This allows the bowel to heal after surgery or when part of the intestine is removed. The decision to create an ostomy is made when other options are not possible.
Types of Ostomies
There are different types of ostomies for bowel resection surgery. These include:
- Colostomy: brings a part of the colon to the abdomen’s surface.
- Ileostomy: brings a part of the ileum (the small intestine’s end) to the surface.
Each type has its own use and care.
Living with an Ostomy
Living with an ostomy requires some changes, but it’s possible to live fully. Proper care, diet adjustments, and managing complications are key. Patients get help on caring for their ostomy and managing their condition.
Immediate Post-Operative Care
The time right after a bowel resection surgery is key for a good recovery. Patients are watched closely to avoid problems and help them heal.
Recovery Room Monitoring
In the recovery room, doctors and nurses keep a close eye on patients. They check vital signs like heart rate and blood pressure. They also look for any signs of trouble, like bleeding or breathing issues.
Pain Management
Managing pain is very important after surgery. Patients get pain medicine, which can be given in different ways, like through an IV or epidural. The goal is to control pain without harming the patient.
Doctors adjust pain treatment based on each patient’s needs and surgery type. They keep checking how much pain the patient feels and change the plan if needed.
Early Mobilization
Early mobilization helps prevent blood clots and speeds up recovery. Patients are helped to move around soon after surgery. This helps prevent blood clots and improves strength and blood flow.
Moving early has many benefits for recovery. Doctors help patients come up with a safe and effective plan for getting up and moving.
Hospital Recovery After Bowel Resection
Recovery in the hospital after bowel resection surgery is a detailed process. It includes adjusting the diet, caring for the wound, and watching for any complications. This time is key to making sure the patient heals well.
Typical Hospital Stay Duration
The time spent in the hospital after surgery can change based on several things. These include how complex the surgery was, the patient’s health, and if any complications arise. Usually, patients stay for 5 to 7 days.
Dietary Progression
Managing the diet is a big part of recovery. At first, patients are on a clear liquid diet to ease the digestive system’s workload. As the bowel heals, the diet moves to full liquids and then soft foods. The pace is set based on how well the patient is doing.
| Diet Stage | Foods Included | Purpose |
| Clear Liquids | Broth, water, clear juices | Minimize digestive stress |
| Full Liquids | Clear liquids plus milk, juice without pulp | Gradually increase nutritional intake |
| Soft Foods | Soft, easily digestible foods like mashed potatoes, yogurt | Continue to increase nutrition while being gentle on the bowel |
Wound Care
Good wound care is vital to avoid infection and help the wound heal. The surgical area is watched for any signs of infection. Patients also learn how to take care of their wounds at home.
- Keep the wound clean and dry
- Monitor for signs of infection
- Follow the healthcare provider’s instructions for dressing changes
Monitoring for Complications
While in the hospital, patients are watched for any complications. These can include infection, bleeding, or problems with the anastomosis. Catching and treating these early is key to avoiding serious problems.
Potential Complications and Risks
Understanding the risks associated with bowel resection surgery is essential for both patients and healthcare providers. The surgery is usually safe, but there are risks to consider. This helps ensure the best care and management.
Immediate Surgical Complications
Complications can happen during or right after surgery. These include bleeding, damage to nearby organs, and bad reactions to anesthesia. “Surgeons do everything they can to avoid these problems,” says a top surgeon.
Infection Risks
Infections are a big risk after bowel resection surgery. Patients might get surgical site infections. These can be treated with antibiotics and good wound care. It’s key for patients to follow their post-op instructions well to lower this risk.
Anastomotic Leak
An anastomotic leak is a serious issue. It happens when the bowel connection doesn’t heal right, causing leaks. This needs quick medical help and might need more surgery.
Long-Term Complications
Long-term problems can include adhesions, bowel obstruction, and changes in bowel habits. Patients might need to change their diet and sometimes have more surgery to fix these issues.
A study in a well-known medical journal found, “Long-term complications after bowel resection show the need for ongoing care and monitoring.”
Knowing about these complications is key to getting the best results. By understanding the risks, patients can prepare better for surgery and recovery.
Recovery at Home Following Bowel Surgery
Recovering at home after bowel surgery means paying attention to a few key areas. These include physical activity, nutrition, and wound care. It’s important to follow the advice given by healthcare professionals to ensure a smooth recovery.
Activity Restrictions
After bowel surgery, it’s important to rest but also start moving again slowly. Avoid heavy lifting (more than 10 pounds) and strenuous activities for at least 4-6 weeks. Short walks are recommended to keep blood flowing and prevent blood clots.
- Resume normal activities gradually as advised by your healthcare provider.
- Avoid bending or straining, which can put pressure on the surgical site.
- Consider having someone assist with household chores during the initial recovery period.
Dietary Recommendations
Eating well is key to healing and recovery. You might start with a liquid or soft food diet and then move to solid foods as you can. Drinking plenty of fluids is also important.
- Start with small, frequent meals to ease digestion.
- Incorporate nutrient-rich foods, including fruits, vegetables, lean proteins, and whole grains.
- Avoid foods that can cause discomfort or digestive issues.
Wound Care at Home
Proper wound care is essential to avoid infection and promote healing. Follow the specific instructions from your healthcare team about cleaning, dressing changes, and watching for infection signs.
- Keep the wound dry and clean as per the instructions.
- Watch for signs of infection, such as redness, swelling, increased pain, or discharge.
- Report any concerns or changes in the wound to your healthcare provider promptly.
When to Contact Your Doctor
Knowing when to call your doctor is important during recovery. Contact your healthcare provider if you have:
- Severe abdominal pain or cramping.
- Fever or chills.
- Vomiting or inability to keep fluids down.
- Signs of infection at the surgical site.
- Any other concerning symptoms or changes in your condition.
By following these guidelines and staying in touch with your healthcare team, you can manage your recovery well. This helps avoid complications and ensures a smooth process.
Conclusion
Bowel resection surgery is a big deal that needs careful thought and planning. It’s important to know about the reasons for the surgery, the different ways it can be done, and what to expect after. This helps patients make smart choices about their health.
Choosing to have bowel resection surgery usually comes after trying other treatments. The surgery can be done in several ways, like open, laparoscopic, or robotic-assisted. Each method has its own good points and things to watch out for.
After the surgery, patients need to rest in the hospital and then at home. They should be ready for possible problems like infections or leaks. Following their doctor’s advice is key to a smooth recovery.
Knowing what to expect during and after surgery helps patients deal with their recovery better. This knowledge lets them be more involved in their care. It can lead to better results and an easier return to daily life.
FAQ
What is bowel resection surgery?
Bowel resection surgery, also known as intestinal resection, removes a diseased part of the intestine. It then connects the healthy parts together.
Why is bowel resection surgery performed?
It’s done to treat many conditions. These include colorectal cancer, inflammatory bowel disease, and bowel obstruction.
What are the different types of bowel resection procedures?
There are several types. These include small intestine resection, large intestine (colon) resection, and rectal resection. Each has its own use and method.
How is bowel resection surgery typically performed?
It can be done in different ways. These include open surgery, laparoscopic surgery, and robotic-assisted surgery. The choice depends on the patient’s condition and the surgeon’s preference.
What is the difference between laparoscopic and open bowel resection?
Laparoscopic surgery uses small incisions. Open surgery uses a larger incision. Laparoscopic surgery usually means less pain and quicker recovery.
Will I need an ostomy after bowel resection surgery?
It depends on the disease and the surgeon’s decision. Some patients need a temporary or permanent ostomy. Others might not need one at all.
How long does it take to recover from bowel resection surgery?
Recovery time varies. It depends on the surgery type and any complications. Patients usually spend a few days in the hospital and weeks at home recovering.
What are the possible complications of bowel resection surgery?
Complications can include immediate surgical issues and infection risks. There’s also a chance of anastomotic leak and long-term problems like bowel obstruction. These risks are managed with proper care and technique.
How can I prepare for bowel resection surgery?
Preparation involves following dietary rules and bowel preparation. You’ll also need to manage your medications and undergo tests. This ensures the best outcome.
What kind of anesthesia is used for bowel resection surgery?
General anesthesia is commonly used. In some cases, regional anesthesia might be an option. The anesthesiologist will discuss the best choice with you.
What are the benefits of minimally invasive bowel surgery?
Techniques like laparoscopic and robotic-assisted surgery offer advantages. These include less pain, faster recovery, and smaller scars compared to open surgery.
How will I manage pain after bowel resection surgery?
Pain management starts in the hospital and continues at home. This includes using pain medications. You’ll also learn how to manage your pain effectively during recovery.
When can I resume normal activities after bowel resection surgery?
The time to resume normal activities varies. It depends on your recovery and the surgeon’s instructions. Generally, you should avoid heavy lifting and bending for several weeks.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29618601/