Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 800,000 hernia repair surgeries happen every year in the United States. Most of these are covered by insurance. It’s important for people facing this surgery to know if their insurance will cover it. Our amazing guide to hernia surgery insurance coverage. We reveal the critical steps to get your medically necessary procedure approved.
At our organization, we understand the need to figure out insurance coverage for hernia surgery. We aim to provide top-notch international healthcare. We also offer personalized VIP service and full medical support.
Most insurance plans do cover hernia surgery. But, how much they cover can change based on your policy and provider. We’ll look into the different parts of insurance coverage for hernia surgery. Our goal is to give you a clear guide through this complex issue.
Key Takeaways
- Most insurance plans cover hernia surgery, but coverage varies by policy and provider.
- Understanding your insurance coverage is key to managing surgery costs.
- We offer full medical support and help with insurance coverage.
- Our goal is to provide outstanding international healthcare with VIP service.
- We help patients understand their insurance options and make informed choices about their care.
Understanding Hernia Surgery
It’s important for patients to know about hernia surgery before they look at insurance. A hernia happens when an organ or tissue pushes through a weak spot in the muscle or tissue that usually keeps it in place.
What is a Hernia?
A hernia is when there’s a weakness or tear in the muscle wall. This lets an organ or tissue bulge out. It can cause pain, discomfort, and serious problems if not treated.
Types of Hernias
There are many types of hernias, each with its own cause and symptoms:
- Inguinal Hernia: This is when tissue, like part of the intestine, pushes through a weak spot in the abdominal muscles in the groin area.
- Umbilical Hernia: It happens near the belly button when part of the intestine bulges through the abdominal wall.
- Hiatal Hernia: This is when the stomach bulges up into the chest through an opening in the diaphragm.
- Incisional Hernia: It develops through a scar or incision in the abdominal wall from previous surgery.
Reasons for Surgery
Surgery is often needed to fix a hernia, mainly if it’s causing a lot of pain or could lead to serious problems. The main reasons for hernia surgery are:
- Relief from Pain: Surgery can help get rid of the pain from hernias.
- Prevention of Complications: Fixing the hernia can stop serious issues like strangulation, where the blood supply to the herniated tissue is cut off.
- Improved Quality of Life: Repairing a hernia can greatly improve a patient’s life by getting rid of the discomfort and limitations it causes.
Knowing about hernias and surgery helps patients make better choices about their insurance and care.
Importance of Insurance Coverage for Surgery
Hernia surgery can be very expensive. But, insurance can help a lot. It covers costs like surgeon fees and post-operative care.
Financial Implications
Insurance is key in managing these costs. It reduces what patients have to pay out of pocket. This lets patients focus on getting better, not on money worries.
The cost of hernia surgery varies. It can be from $10,000 to $20,000 or more. Insurance helps make this cost more affordable, so patients can get the surgery they need.
“Having insurance coverage for hernia surgery can be a significant financial relief, allowing patients to prioritize their health and recovery.”
Peace of Mind
Insurance also brings peace of mind. It means patients don’t have to worry about the surgery’s cost. This reduces stress and anxiety.
Dealing with insurance can be hard. But, having good coverage makes a big difference. Patients should check their insurance before surgery to know what’s covered.
“Insurance coverage is not just about financial protection; it’s also about having the peace of mind that comes with knowing you’re covered.”
— Medical Insurance Expert
In summary, insurance is vital for hernia surgery. It helps with money worries and gives peace of mind. This lets patients focus on getting better.
Types of Insurance that May Cover Surgery
Many insurance types can cover hernia surgery, each with its own rules. It’s key to know these options to handle the cost of your care.
Private Insurance Plans
Private insurance plans vary a lot in hernia surgery coverage. Some offer full benefits, while others are more limited. It’s vital to check your policy to see what’s covered and what you’ll pay out of pocket.
When looking at private insurance, think about deductibles, copays, and coinsurance. Knowing these can help you guess your costs.
Medicare Coverage
Medicare, for people 65 and older, covers hernia surgery under certain rules. Medicare Part A and Part B might cover different parts of your care, like hospital stays and surgeries.
To make sure you’re covered, it’s important to know Medicare’s rules and any costs you might face.
Medicaid Eligibility
Medicaid, for low-income folks, also covers hernia surgery. But, eligibility and what’s covered can vary a lot by state.
We suggest contacting your state’s Medicaid office to find out what’s covered and any rules you need to follow.
Factors Influencing Coverage Decisions
It’s important for patients to understand what affects insurance coverage for hernia surgery. Insurance companies make decisions based on the policy and if the surgery is needed.
Policy Exclusions and Limitations
Insurance policies have exclusions and limits that can impact hernia surgery coverage. Policy exclusions are certain conditions or procedures not covered. For example, some policies might not cover all hernia types or only pay for surgeries that are really needed.
It’s a good idea to read your insurance policy well. Look for what’s not covered and what is. Important things to check include:
- Specific hernia types or conditions that are excluded
- Limitations on surgical procedures or treatments
- Exclusions related to pre-existing conditions
Medical Necessity Criteria
The need for a procedure is a big factor in insurance decisions. Insurance usually only covers what’s medically necessary. What counts as necessary can differ by insurance company but often includes:
- The severity of the hernia and its health impact
- Presence of symptoms like pain or discomfort
- Failure of other treatments
We suggest patients work with their doctors to meet insurance’s medical necessity standards. This might mean sharing medical records and other documents to show why surgery is needed.
How to Check Your Insurance Policy
To get ready for hernia surgery costs, it’s key to check your insurance policy. This step helps you know what’s covered and what you might have to pay out-of-pocket.
Verifying Benefits
Verifying your insurance benefits means looking at the details of your coverage. Here’s what to check:
- Coverage Details: Find out what your plan covers, including any limits on hernia surgery.
- Pre-Authorization Requirements: See if you need approval before your surgery. We can help with this.
- Out-of-Pocket Costs: Figure out any deductibles, copays, or coinsurance you’ll have to pay.
By checking these benefits, you can plan better for your surgery and avoid surprise costs. Healthcare experts say, “Knowing your insurance is vital for managing medical expenses.”
“Insurance coverage greatly affects your financial planning for medical procedures. It’s important to review your policy to know what’s included.”
— Medical Insurance Expert
Understanding Your Deductibles
Understanding your deductibles is key to managing healthcare costs. Here are important points to remember:
- Deductible Amount: Know how much you must pay before your insurance starts.
- Copays and Coinsurance: Understand any extra costs after you’ve met your deductible.
- Maximum Out-of-Pocket: Know the most you’ll pay each year, including deductibles, copays, and coinsurance.
By carefully looking at your insurance policy and understanding deductibles, you can make smart choices about your care and finances. We’re here to help you through these steps, ensuring you get the care you need without financial surprises.
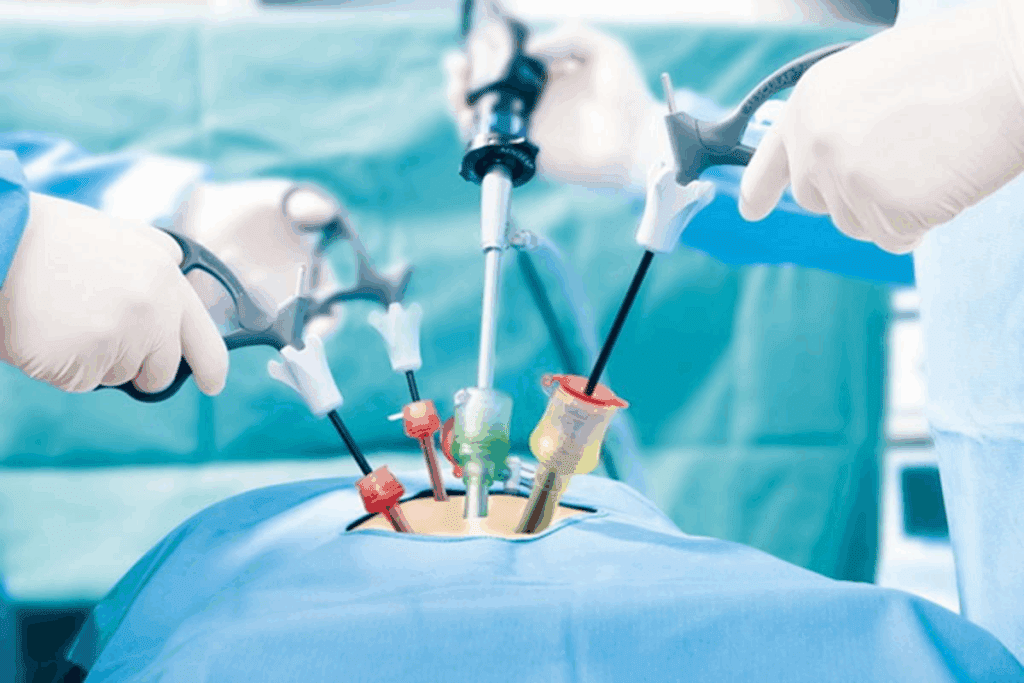
Pre-Authorization: What You Need to Know
Before you have hernia surgery, it’s key to know about pre-authorization. This is when insurance checks if a surgery is needed and if it’s covered. It’s a big step in getting your surgery approved.
The Importance of Pre-Authorization
Pre-authorization is a big deal for hernia surgery. It makes sure your surgery is needed and covered by your insurance. This way, you won’t face unexpected bills.
Key benefits of pre-authorization include:
- Confirmation of medical necessity
- Reduced risk of denied claims
- Clear understanding of coverage and out-of-pocket costs
- Streamlined billing process
How to Obtain Pre-Authorization
To get pre-authorization, follow these steps. First, your doctor will send a request to your insurance. They’ll include all the details about your surgery. Then, the insurance will decide if it’s covered.
To make the process easier:
- Make sure your doctor has all the needed documents.
- Check if your insurance got the request.
- Ask your insurance about your pre-authorization status.
Knowing about pre-authorization and how to get it helps a lot. It makes your hernia surgery process smoother.
In-Network vs. Out-of-Network Providers
It’s important to know the difference between in-network and out-of-network providers for hernia surgery costs. Your insurance coverage greatly affects how much you’ll pay out of pocket.
Benefits of Choosing In-Network Providers
In-network providers have deals with your insurance company. This means they charge lower rates for their services. Choosing an in-network provider for hernia surgery can help you save money because:
- Lower out-of-pocket costs due to pre-negotiated rates
- Reduced risk of unexpected medical bills
- Simplified billing processes
These advantages can make hernia surgery costs more affordable for patients.
Potential Costs of Out-of-Network Providers
Out-of-network providers don’t have deals with your insurance. This can lead to:
- Higher out-of-pocket costs due to the lack of negotiated rates
- Increased risk of receiving surprise medical bills
- More complex billing and reimbursement processes
While sometimes choosing an out-of-network provider is necessary, it’s key to know the financial risks involved.
We suggest checking if your insurance covers in-network providers. Also, talk to your healthcare provider about any concerns. This way, you can make a well-informed choice about your care.
Common Questions About Coverage
Many patients wonder about their insurance coverage for hernia repair surgery. It’s important to know the details of your coverage, even for procedures that might not be urgent.
What If Surgery Is Considered Elective?
Insurance for hernia surgery can change if it’s seen as elective. Elective surgery coverage depends on your insurance and policy. Always check your policy to see what’s covered.
Insurance might not cover surgery if the hernia isn’t causing big problems. But, many plans do cover it if it’s needed for health reasons.
Are All Procedures Covered?
Insurance doesn’t cover all parts of hernia surgery. The covered hernia repair procedure might include the surgery itself. But, things like insurance covers hernia mesh surgery might have special rules.
Procedure | Typical Coverage | Conditions/Requirements |
Hernia Repair Surgery | Generally covered if medically necessary | Pre-authorization may be required |
Hernia Mesh Surgery | Covered in most cases | Specific mesh types may be preferred or required |
Elective Hernia Surgery | Coverage varies by policy | May require additional documentation or justification |
Make sure to check with your insurance about what’s covered. This will help you understand what’s included and what’s not.
Financial Assistance Options
Hernia surgery can be expensive, but there are ways to make it more affordable. We know it’s hard to handle medical costs. So, we help our patients find financial aid programs.
Payment Plans and Financing
Payment plans and financing are key to managing hernia surgery costs. Many providers offer flexible plans to spread out payments. Financing options might have low or no interest for some patients.
Patients should talk to their healthcare provider’s billing team about these options. They can find the best plan or financing for their situation. It’s important to ask about any fees and the total amount that can be financed.
Nonprofit Organizations Providing Aid
Some nonprofit organizations also offer financial help for hernia surgery. They might give grants or other aid to reduce costs for patients.
Patients can look for nonprofits that help with medical costs. These groups have rules for who can get help. We can guide you to reputable nonprofits that have helped our patients.
Exploring these options can make hernia surgery more affordable. We’re here to support our patients, including with financial help.
Next Steps After Surgery Authorization
After getting insurance approval, it’s time to prepare for surgery and learn about insurance claims after. Patients can take steps to make their surgery go smoothly.
Preparing for Your Surgery
Getting ready for hernia surgery is important. Patients should listen to their doctor’s advice on diet, medications, and aftercare. Here’s what to do:
- Follow your doctor’s diet advice before surgery.
- Tell your doctor about all medicines you’re taking.
- Make arrangements for someone to drive you home and help with care.
These steps can help avoid problems and speed up recovery.
Post-Surgery Insurance Claims
Knowing how to file insurance claims after surgery is key. Keep all records of your surgery and costs. Here’s how:
- Get a detailed bill from your doctor or hospital.
- Save receipts for any costs you paid yourself.
- Follow your insurance company’s claim process, which might be online or by mail.
Being organized can make things easier and help you get the benefits you deserve.
Our team is here to help with care and support before, during, and after surgery. We guide you through insurance claims and make sure you get the care you need.
Reviewing Your Insurance Plan Annually
It’s important to check your insurance plan every year. This makes sure it covers your healthcare needs, like hernia surgery. Changes in healthcare and insurance plans happen, so yearly checks help spot any missing coverage or policy updates.
Key Aspects to Review
When you look at your insurance, check the coverage details. Look for any changes to deductibles, copays, or coinsurance. This ensures you have enough coverage for hernia surgery and other medical needs.
Adjusting Coverage for Future Needs
Adjusting your coverage based on your health and future medical costs is wise. It gives you peace of mind and financial security. Regularly reviewing and updating your insurance helps prepare you for any medical needs, including hernia surgery.
Being proactive with your insurance coverage is key. It helps avoid unexpected medical bills and ensures you get quality care.
FAQ
Will my insurance cover hernia surgery?
Insurance coverage for hernia surgery depends on your policy and if the surgery is needed. Check your policy and talk to your insurance to see what’s covered.
What factors influence insurance coverage decisions for hernia surgery?
Insurance decisions are based on policy rules and if the surgery is necessary. Knowing these can help you understand your coverage for hernia surgery.
How do I check my insurance policy for hernia surgery coverage?
To check your policy, look at your benefits and deductibles. Also, check for any exclusions or limitations. This will show you what’s covered and what’s not.
What is pre-authorization, and why is it important for hernia surgery?
Pre-authorization means getting approval from your insurance before surgery. It makes sure the surgery is needed and covered by your plan.
How does choosing between in-network and out-of-network providers affect my costs?
Choosing in-network providers can save you money. They have deals with your insurance. Out-of-network providers might cost more or not be covered.
Will my insurance cover hernia surgery if it’s considered elective?
Insurance usually covers necessary surgeries, not elective ones. If your hernia surgery is needed, it’s more likely to be covered.
Are all aspects of the hernia repair procedure covered, including the use of hernia mesh?
Coverage for hernia surgery, including mesh use, depends on your policy. Check your policy and talk to your insurance to know what’s covered.
What financial assistance options are available for hernia surgery?
There are ways to help with surgery costs, like payment plans and nonprofit help. These options can make surgery more affordable.
How do I prepare for hernia surgery after insurance authorization?
Get ready for surgery by following your doctor’s advice. This might include diet changes, stopping meds, and arranging for care after surgery.
What are the next steps after insurance authorization for hernia surgery?
After getting approval, prepare for surgery and understand how to file claims. Keep records of your surgery and costs.
Why is it essential to review my insurance plan annually?
Reviewing your insurance plan yearly ensures it covers your healthcare needs. This helps spot any coverage gaps or policy changes.
Does Medicare cover hernia surgery?
Medicare might cover hernia surgery under certain conditions. Check Medicare’s coverage and talk to a healthcare expert to see what’s covered.
Does Medicaid cover hernia repair surgery?
Medicaid’s coverage for hernia surgery varies by state. Check Medicaid in your state to see what’s covered.
What is the impact of insurance deductible on hernia surgery costs?
Knowing your deductible and out-of-pocket costs for hernia surgery is important. Review your policy to understand these costs.
How does pre-authorization for hernia surgery affect my insurance claim?
Pre-authorization helps your insurance claim process smoothly. It reduces the chance of delays or denials.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7787284/