Last Updated on December 2, 2025 by Bilal Hasdemir
This statistic highlights the effectiveness and reliability of non-mesh hernia repair methods. We specialize in providing premium care through advanced tissue repair techniques, such as the Shouldice Repair, which have been refined over decades to ensure optimal surgical outcomes and high patient satisfaction.
Our team is dedicated to delivering exceptional medical care with a focus on personalized service and comprehensive support.
The ultimate guide to the best non-mesh hernia repair. We explore the amazing benefits of the Shouldice, Bassini, and other techniques.
Key Takeaways
- Over 400,000 successful hernia repairs have been performed using these techniques.
- Tissue repair techniques, such as Shouldice Repair, offer optimal surgical outcomes.
- Our team is committed to delivering premium care with personalized service.
- We prioritize patient satisfaction through comprehensive medical support.
Understanding Hernias: Types and Causes
A hernia occurs when an organ or tissue protrudes through a weakened area in the muscle or fascia, leading to various health issues. This condition can manifest in different forms and is influenced by a range of factors, including genetics, lifestyle, and overall health.
What is a Hernia?
A hernia is essentially a breach in the integrity of the abdominal wall, allowing contents such as intestine or fatty tissue to bulge through. This can result in a visible lump or discomfort, particularly during physical activities or straining.
The abdominal wall is composed of layers of muscle and fascia, which provide containment and support for internal organs. When there is a weakness or defect in these layers, it can lead to the protrusion of organs or tissues, forming a hernia.
Common Types of Hernias
There are several types of hernias, each with distinct characteristics and implications:
- Inguinal Hernia: Occurs when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles in the groin area.
- Umbilical Hernia: Happens near the belly button, often due to a weakness in the abdominal wall near the navel.
- Incisional Hernia: Develops through a scar or incision in the abdominal wall, resulting from previous abdominal surgery.
Each type of hernia has its specific causes and risk factors, which are crucial to understand for effective management and treatment.
Causes and Risk Factors of Hernias
Hernias are caused by a combination of factors, including congenital conditions, lifestyle factors, and certain health considerations. Some of the key risk factors include:
- Genetic Predisposition: Individuals with a family history of hernias are more likely to develop one.
- Age: The risk of developing a hernia increases with age, as the muscles and tissues weaken over time.
- Physical Strain: Activities that involve heavy lifting, bending, or straining can increase the risk.
- Chronic Conditions: Certain conditions, such as chronic coughing or constipation, can also contribute to the development of hernias.
Understanding these causes and risk factors is essential for prevention and for making informed decisions about treatment options.
An Overview of Hernia Repair Options
Hernia repair options are diverse, encompassing both surgical and non-surgical approaches, each with its own set of benefits and considerations. When considering hernia repair, it’s essential to understand the various methods available to determine the most appropriate treatment plan.
Surgical vs. Non-Surgical Approaches
Surgical and non-surgical approaches are the two primary categories of hernia repair. Surgical approaches involve operative techniques to repair the hernia, either through open surgery or laparoscopic surgery. Non-surgical approaches, on the other hand, may include watchful waiting, lifestyle modifications, and the use of supportive devices.
We recommend discussing the risks and benefits of each approach with a healthcare professional to determine the best course of treatment. The choice between surgical and non-surgical methods depends on several factors, including the type and size of the hernia, the patient’s overall health, and their personal preferences.
Overview of Mesh vs. Non-Mesh Techniques
Within surgical hernia repair, there are two main techniques: mesh and non-mesh repairs. Mesh repair involves using a synthetic or biological mesh to reinforce the weakened area, promoting tissue ingrowth and reducing the likelihood of recurrence. Non-mesh repair techniques, such as suturing or tissue repair, rely on the patient’s own tissues to close the hernia defect.
| Technique | Description | Benefits |
| Mesh Repair | Uses synthetic or biological mesh to reinforce the weakened area. | Lower recurrence rates, stronger repair. |
| Non-Mesh Repair | Rely on the patient’s own tissues to close the hernia defect. | Avoids potential mesh complications, suitable for certain patient groups. |
Both mesh and non-mesh techniques have their place in hernia repair, and the choice between them depends on various factors, including the patient’s condition, the surgeon’s expertise, and the specific characteristics of the hernia.
Non-mesh hernia repair offers several key benefits that contribute to improved patient outcomes. By avoiding the use of mesh, patients can experience a reduced risk of certain complications associated with mesh implantation.
Reduced Risk of Complications
One of the significant advantages of non-mesh hernia repair is the reduced risk of complications. Mesh-related complications can include:
- Mesh rejection or migration
- Chronic pain
- Infection
- Bowel obstruction or adhesion
Biocompatible Materials Used
Although non-mesh hernia repair does not use mesh, it still utilizes materials that are highly biocompatible. These materials are designed to be compatible with the body’s tissues, reducing the likelihood of adverse reactions. For instance, sutures made from absorbable materials like Vicryl or Monocryl are often used, promoting natural healing without leaving foreign materials behind.
“The use of biocompatible materials in non-mesh hernia repair aligns with our commitment to delivering the highest quality care, ensuring that our patients receive the best possible outcomes.”
Shorter Recovery Times
Non-mesh hernia repair techniques are often associated with shorter recovery times. This is because the body’s natural tissue repair mechanisms are allowed to function without the presence of foreign materials. Patients typically experience less postoperative pain and can return to their normal activities sooner.
Key benefits of non-mesh hernia repair include:
- Reduced risk of mesh-related complications
- Use of biocompatible materials
- Potential for shorter recovery times
- Improved patient satisfaction due to fewer postoperative issues
At our institution, we prioritize patient care and outcomes. By choosing non-mesh hernia repair when appropriate, we aim to provide our patients with the best possible results, enhancing their overall quality of life.
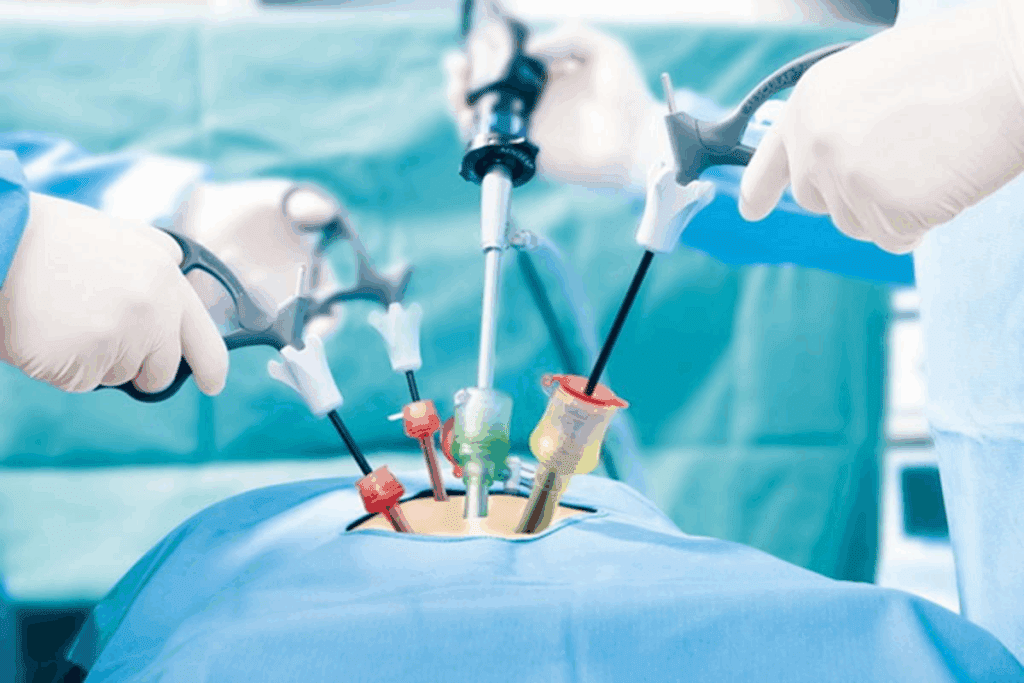
Open hernia repair is a traditional method where the surgeon makes a single incision in the groin to access the hernia. This technique allows for direct visualization and repair of the hernia. One of the well-known open repair techniques is the Shouldice repair, which involves a multi-layered closure of the posterior wall of the inguinal canal using the patient’s own tissues. This method is renowned for its low recurrence rates and is often considered the gold standard in non-mesh hernia repair.
Laparoscopic hernia repair, on the other hand, is a minimally invasive technique that involves making several small incisions through which a laparoscope and surgical instruments are inserted. This approach allows for a faster recovery and less postoperative pain compared to open repair. The laparoscopic technique is particularly beneficial for patients with bilateral hernias or those who have had previous hernia repairs. However, it requires specialized training and equipment.
Other Innovative Techniques
Beyond open and laparoscopic repairs, there are other innovative non-mesh techniques being explored and utilized. These include:
- Endoscopic-assisted hernia repair: A technique that combines the benefits of laparoscopic surgery with the security of open repair.
- Robotic hernia repair: Utilizes robotic systems to enhance the precision and dexterity of the surgeon during the procedure.
- Tissue repair techniques: Various methods that focus on reinforcing the hernia site using the patient’s own tissues, often through suturing or other tissue approximation methods.
These innovative techniques are continually evolving, with ongoing research aimed at improving outcomes and reducing recovery times. As we move forward, it’s likely that we will see even more advanced and effective non-mesh hernia repair methods.
What to Expect During Non-Mesh Hernia Surgery
As you prepare for non-mesh hernia surgery, it’s essential to know what to expect from the preoperative assessment through the surgical procedure and into postoperative care. Understanding these steps can help alleviate anxiety and ensure a smoother recovery process.
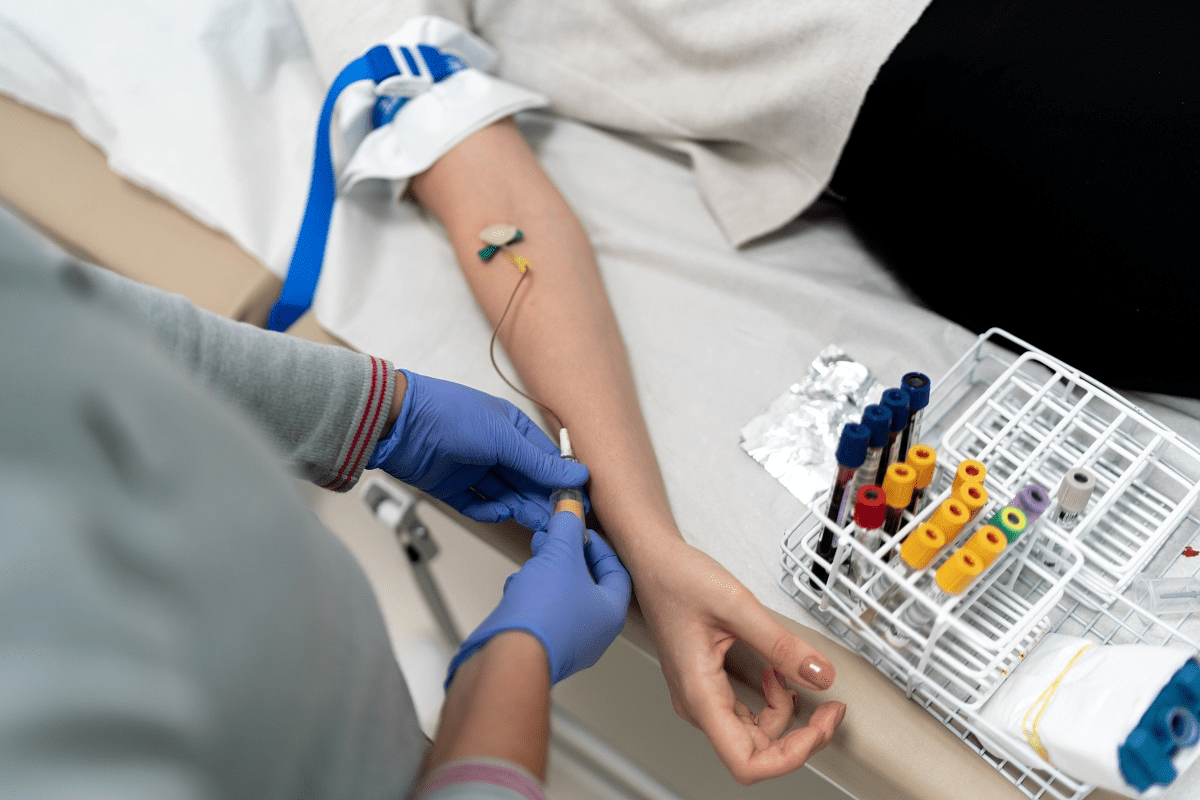
Preoperative Assessment
Before undergoing non-mesh hernia surgery, you will undergo a thorough preoperative assessment. This evaluation is crucial for identifying any potential risks and ensuring that you are adequately prepared for the surgery.
The assessment typically includes a review of your medical history, current medications, and any allergies you may have. Our team will also conduct necessary physical examinations and may order diagnostic tests such as blood work or imaging studies.
- Review of medical history
- Assessment of current medications and allergies
- Physical examination
- Diagnostic tests (blood work, imaging studies)
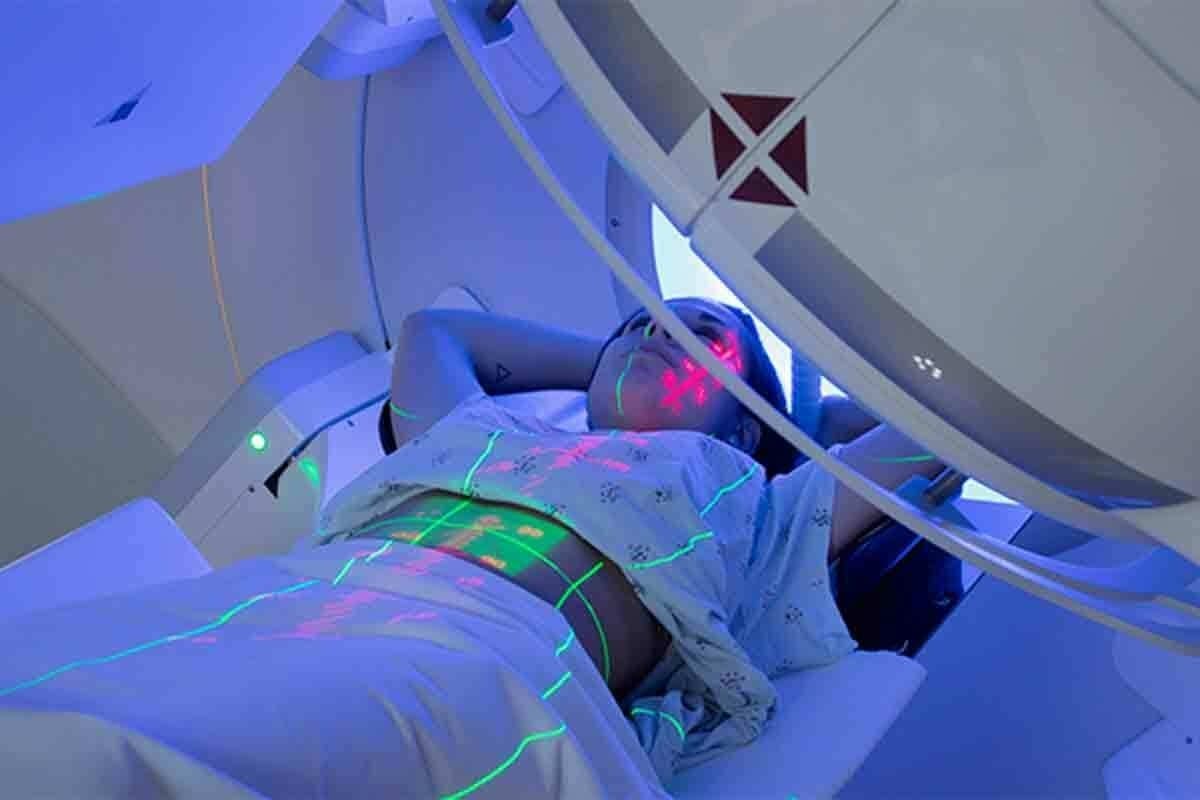
The Surgical Procedure
Non-mesh hernia repair surgery involves several techniques, including open and laparoscopic methods. The choice of technique depends on the type and severity of the hernia, as well as your overall health.
During the surgery, we will make incisions to access the hernia, carefully repair the weakened area, and then close the incisions. The use of biocompatible materials ensures a safe and effective repair.
| Surgical Technique | Description | Benefits |
| Involves a single incision to access the hernia | Effective for complex hernias, allows for direct visualization | |
| Minimally invasive, using several small incisions and a camera | Less postoperative pain, quicker recovery time |
Postoperative Care and Monitoring
After the surgery, our team will closely monitor your recovery to manage any pain or discomfort and watch for any signs of complications.
Postoperative care includes pain management through medication, monitoring for infection, and follow-up appointments to ensure the hernia is healing properly.
Key aspects of postoperative care include:
- Pain management
- Monitoring for complications
- Follow-up appointments
By understanding what to expect during non-mesh hernia surgery, you can better prepare yourself for the process and recovery. Our team is committed to providing you with the highest quality care throughout your journey.
Recovering from non-mesh hernia repair requires patience, and knowing what to expect can make a significant difference. We understand that the recovery process can be just as important as the surgery itself, and we’re here to guide you through it.
Initial Recovery Phase
The initial recovery phase typically lasts a few weeks. During this time, patients are advised to avoid heavy lifting, bending, or strenuous activities. We recommend taking it easy and allowing your body to heal. Most patients can resume normal activities within 2-4 weeks, but this can vary depending on individual factors, such as overall health and the complexity of the surgery.
Key aspects to focus on during the initial recovery phase include:
- Managing pain effectively through medication and rest
- Monitoring the surgical site for any signs of infection or complications
- Gradually increasing physical activity as advised by your healthcare provider
Long-Term Recovery Expectations
While the initial recovery phase is crucial, long-term recovery expectations are equally important. Full recovery from non-mesh hernia repair can take several months. During this period, patients may experience occasional discomfort or soreness, which should gradually diminish over time.
To ensure a smooth long-term recovery, we advise patients to:
- Follow a balanced diet to support healing and overall health
- Engage in regular, moderate exercise to maintain strength and flexibility
- Attend follow-up appointments with your surgeon to monitor the healing process
By understanding the recovery timeline and following our guidance, patients can optimize their healing process and return to their normal activities with confidence.
Success Rates and Effectiveness
The efficacy of non-mesh hernia repair is supported by evidence-based data highlighting its success rates and long-term outcomes. We will examine the factors that influence the effectiveness of this surgical approach and compare its outcomes with those of mesh repair techniques.
Influencing Factors
Several factors contribute to the success rates of non-mesh hernia repair. These include:
- Surgeon Expertise: The skill and experience of the surgeon play a crucial role in determining the success of the procedure.
- Patient Selection: Careful selection of patients based on their overall health and the type of hernia is vital.
- Surgical Technique: The choice of non-mesh technique, such as the Shouldice repair, can significantly impact outcomes.
By understanding and optimizing these factors, we can enhance the effectiveness of non-mesh hernia repair. For more detailed information on non-mesh hernia repair, you can visit .
Comparative Outcomes
When comparing non-mesh hernia repair to mesh repair, several studies have shown that non-mesh techniques can offer comparable, if not superior, success rates. The table below summarizes key findings from recent studies.
| Repair Technique | Recurrence Rate | Complication Rate |
| Non-Mesh Repair | 2-5% | 5-10% |
| Mesh Repair | 1-3% | 10-15% |
As shown in the table, while mesh repair may have a slightly lower recurrence rate, non-mesh repair tends to have a lower complication rate, making it a favorable option for many patients.
We believe that the success of non-mesh hernia repair is multifaceted, relying on a combination of skilled surgeons, appropriate patient selection, and the chosen surgical technique. By focusing on these elements, we can achieve high success rates and positive outcomes for our patients.
Potential Risks and Complications
Understanding the potential complications of non-mesh hernia repair is essential for making informed decisions about your care. While we strive to provide the best possible outcomes, it’s crucial to acknowledge that, like any surgical procedure, non-mesh hernia repair carries certain risks.
Common Complications of Non-Mesh Repair
Non-mesh hernia repair can be associated with several complications, including:
- Infection: As with any surgical procedure, there’s a risk of infection with non-mesh hernia repair.
- Recurrence: There’s a possibility that the hernia could recur, requiring further treatment.
- Nerve Damage: Nerve damage is a potential complication, which can result in numbness or pain.
- Bleeding or Hematoma: Bleeding or the formation of a hematoma (a collection of blood outside a blood vessel) can occur.
It’s essential to note that while these complications can occur, their incidence can be significantly reduced with proper surgical technique and postoperative care.
How to Minimize Risks
Minimizing the risks associated with non-mesh hernia repair involves a combination of careful patient selection, meticulous surgical technique, and comprehensive postoperative care. Here are some strategies we employ:
- Preoperative Assessment: A thorough preoperative assessment helps identify potential risks and allows us to take necessary precautions.
- Surgical Expertise: Our surgeons are highly experienced in performing non-mesh hernia repairs, which is critical in minimizing complications.
- Postoperative Monitoring: Close monitoring after surgery enables us to quickly identify and address any complications that may arise.
| Complication | Risk Minimization Strategy |
| Infection | Prophylactic antibiotics, sterile surgical technique |
| Recurrence | Proper surgical technique, postoperative support |
| Nerve Damage | Careful dissection, nerve-sparing techniques |
| Bleeding or Hematoma | Meticulous hemostasis, postoperative monitoring |
By understanding the potential risks and taking proactive steps to minimize them, we can ensure the best possible outcomes for our patients undergoing non-mesh hernia repair.
Choosing the Right Surgeon for Non-Mesh Repair
Selecting the right surgeon for non-mesh hernia repair is a crucial decision that significantly impacts the outcome of your surgery. We understand the importance of this choice and are committed to guiding you through the process.
When searching for a surgeon, it’s essential to consider several key factors that contribute to a successful non-mesh hernia repair. We will walk you through the critical qualifications and characteristics to look for in a surgeon.
What Qualifications to Look For
A qualified surgeon for non-mesh hernia repair should possess specific training and expertise. We recommend looking for surgeons who are:
- Board-certified in general surgery or a related specialty
- Fellowship-trained in hernia repair or minimally invasive surgery
These qualifications ensure that your surgeon has the necessary knowledge and skills to perform your surgery effectively.
Importance of Experience and Reviews
Experience is a critical factor when choosing a surgeon for non-mesh hernia repair. We suggest looking for surgeons with:
- A high volume of hernia repair surgeries performed annually
- A track record of successful outcomes and low complication rates
- Positive patient reviews and testimonials
| Qualification/Experience | Description | Importance Level |
| Board Certification | Certified by a recognized medical board | High |
| Fellowship Training | Specialized training in hernia repair or minimally invasive surgery | High |
| Experience in Non-Mesh Repair | Proven track record of performing non-mesh hernia repairs | High |
| Patient Reviews | Positive feedback from previous patients | Medium |
By considering these factors and qualifications, you can make an informed decision when choosing a surgeon for your non-mesh hernia repair. We are dedicated to supporting you throughout this process to ensure the best possible outcome.
Preparing for Your Surgery: Tips and Considerations
As you prepare for non-mesh hernia repair surgery, we want to ensure you feel supported and informed every step of the way. Proper preparation is key to a smooth and successful surgical experience.
Preoperative Preparations to Know
To prepare for your surgery, follow specific preoperative instructions, such as dietary changes or cessation of certain medications. We will provide you with detailed guidance on how to prepare, including any necessary tests or evaluations.
Key Questions for Your Surgeon
Before your non-mesh hernia repair, we recommend asking your surgeon questions about the procedure, recovery expectations, and postoperative care. This will help you understand what to expect and ensure a successful outcome.
By being prepared and informed, you can minimize risks and optimize your recovery. We are committed to delivering exceptional care and support throughout your surgical journey.
FAQ
What is non-mesh hernia repair?
Non-mesh hernia repair is a surgical technique used to repair hernias without the use of synthetic mesh. Instead, it often utilizes sutures or biocompatible materials to reinforce the weakened area.
What are the benefits of non-mesh hernia repair?
The benefits of non-mesh hernia repair include reduced risk of complications associated with mesh, such as chronic pain and mesh migration, as well as potentially shorter recovery times and the use of biocompatible materials.
What types of hernias can be treated with non-mesh repair?
Various types of hernias, including inguinal, umbilical, and incisional hernias, can be treated with non-mesh repair techniques, depending on the patient’s condition and the surgeon’s expertise.
How long does it take to recover from non-mesh hernia repair?
Recovery times can vary, but most patients can expect to return to normal activities within a few weeks. The initial recovery phase typically involves rest and limited activity, followed by a gradual return to full activity.
What are the potential complications of non-mesh hernia repair?
While generally safe, non-mesh hernia repair can be associated with complications such as infection, bleeding, and recurrence. However, our experienced surgeons take steps to minimize these risks.
How do I choose the right surgeon for non-mesh hernia repair?
When selecting a surgeon, look for board certification, experience in non-mesh hernia repair techniques, and positive patient reviews. It’s also essential to discuss your options and concerns with your surgeon.
What preoperative preparations are necessary for non-mesh hernia surgery?
Preoperative preparations may include medical evaluations, adjustments to medications, and lifestyle changes. Your surgeon will provide specific guidance on how to prepare for your surgery.
What questions should I ask my surgeon before non-mesh hernia repair?
Consider asking about your surgeon’s experience with non-mesh techniques, the specifics of the procedure, potential risks and complications, and what to expect during recovery.
How effective is non-mesh hernia repair compared to mesh repair?
Non-mesh hernia repair can be an effective alternative to mesh repair, with comparable success rates in many cases. The choice between techniques depends on individual patient factors and surgeon expertise.
What is the Shouldice Repair technique?
The Shouldice Repair is a type of non-mesh hernia repair that involves a multi-layered closure of the posterior wall of the inguinal canal using a specific suturing technique. It’s known for its low recurrence rates.
Are there any long-term results or studies on non-mesh hernia repair?
Yes, there are studies and long-term data available on non-mesh hernia repair techniques, showing promising results in terms of recurrence rates and patient satisfaction. We can provide you with the most current evidence-based information.
Can I expect less pain with non-mesh hernia repair?
Many patients experience less chronic pain with non-mesh hernia repair compared to mesh repair. However, pain management varies from person to person, and our team will work with you to develop an effective pain management plan.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11872052/