Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that about 50% of people over 60 in the United States have diverticulosis? This condition can lead to diverticulitis.
Diverticulitis happens when small pouches in the colon wall get inflamed. This can cause severe pain, changes in bowel habits, and other symptoms. It’s important to manage diverticulitis well to avoid serious problems and improve life quality.
We know that treating diverticulitis needs a full plan, including diet and lifestyle changes. By understanding the condition and its symptoms, we can find the best treatment.
Key Takeaways
- Diverticulitis is a common condition that affects a significant portion of the population over 60.
- Managing diverticulitis symptoms is key to avoid complications.
- A complete treatment plan includes diet changes and lifestyle adjustments.
- Understanding diverticulitis is the first step towards effective management.
- A healthy diet is very important in managing diverticulitis symptoms.
Understanding Diverticulitis: An Overview
Diverticulitis is a condition where the diverticula in the digestive tract get inflamed. Understanding diverticulitis is crucial for effective management. We’ll look into what diverticulitis is, its symptoms, and what causes it.
What is Diverticulitis?
Diverticulitis happens when the diverticula in the colon wall get inflamed or infected. It can be mild or severe. It’s often linked to diverticulosis, which is having diverticula without inflammation.
The exact reason for diverticulitis isn’t always known. But it’s thought to be due to diet, lifestyle, and genetics.
Symptoms of Diverticulitis
The symptoms of diverticulitis can vary. They usually include:
- Abdominal pain, often in the lower left side
- Fever and chills
- Nausea and vomiting
- Changes in bowel habits
- Bloating and gas
These symptoms can be like those of other conditions. So, getting a proper diagnosis is key. If symptoms don’t go away or get worse, see a doctor.
Causes and Risk Factors
Several things can lead to diverticulitis. Knowing these can help prevent and manage it:
Risk Factor | Description |
Age | Diverticulitis is more common in people over 40 years old. |
Diet | A low-fiber diet can increase the risk of developing diverticulitis. |
Lifestyle | Lack of physical activity and obesity are associated with an increased risk. |
Genetics | A family history of diverticulitis can increase an individual’s risk. |
Knowing these risk factors and symptoms helps manage the condition. It also helps find the right medical care when needed.
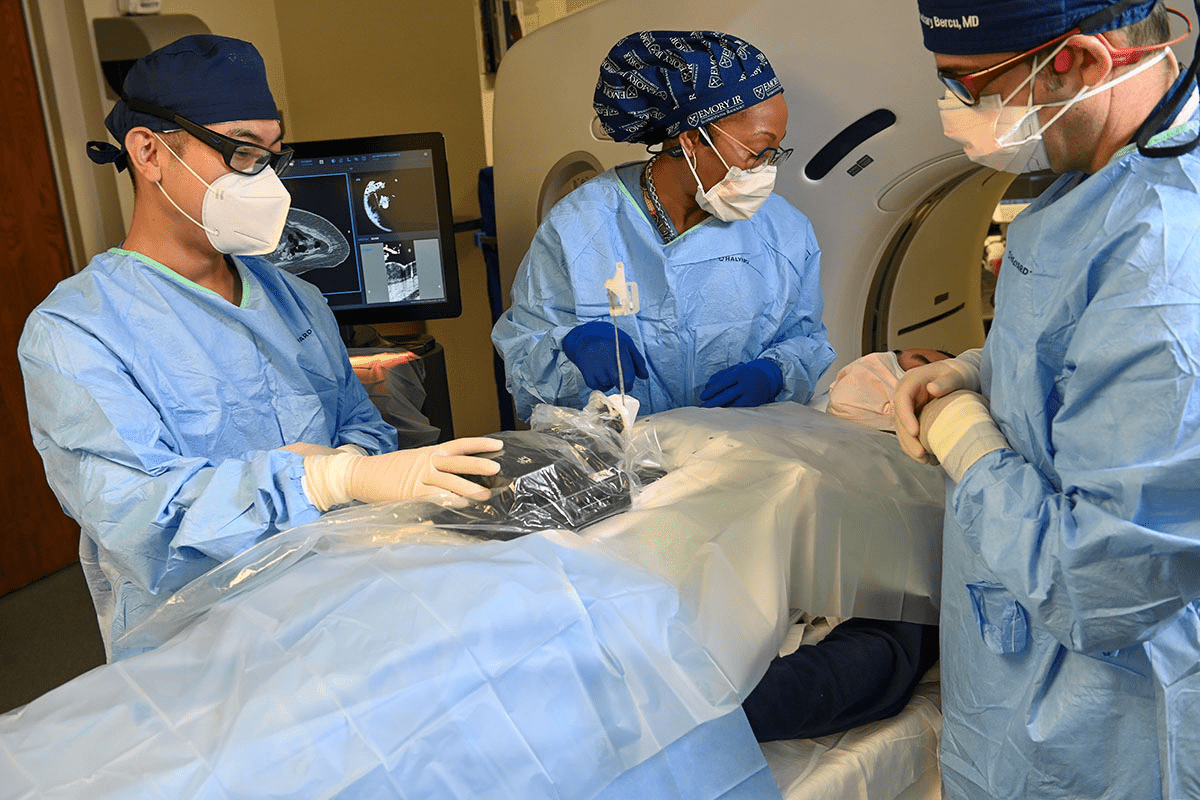
Diagnosing Diverticulitis
Doctors use a detailed medical history, physical exam, and specific tests to diagnose diverticulitis. We’ll look at how they do it and why catching it early is so important.
Common Diagnostic Tests
Several tests help find diverticulitis. These include imaging, blood tests, and colonoscopy.
- Imaging Tests: CT scans are top for spotting diverticulitis, showing inflamed areas clearly.
- Blood Tests: They check for infection or inflammation signs.
- Colonoscopy: This looks inside the colon, done after the acute phase ends.
Diagnostic Test | Purpose |
CT Scan | Accurately visualizes inflamed diverticula |
Blood Tests | Checks for signs of infection or inflammation |
Colonoscopy | Examines the inside of the colon |
Importance of Early Detection
Finding diverticulitis early is key to avoiding serious problems. Quick diagnosis means quicker treatment, lowering risks of abscesses, perforations, or peritonitis.
Timely diagnosis is key to effective management. Knowing about the diagnostic process helps patients make better choices.
Home Remedies for Managing Symptoms
Managing diverticulitis symptoms at home involves making dietary changes, using over-the-counter medications, and staying hydrated. These home remedies can help ease symptoms and improve your life quality.
Dietary Adjustments
Changing your diet is key in managing diverticulitis symptoms. Eating foods high in fiber helps soften stool and reduces pressure on the diverticula.
- Fiber-rich foods include fruits, vegetables, and whole grains.
- Avoiding low-fiber foods like processed meats and dairy is also helpful.
Here’s a sample dietary plan:
Meal | Foods to Include | Foods to Avoid |
Breakfast | Oatmeal with fruits | Processed cereals |
Lunch | Vegetable salad with whole grain bread | Processed meats |
Dinner | Grilled vegetables with brown rice | Dairy products |
Over-the-Counter Relief
Over-the-counter medications can help with diverticulitis symptoms. Antispasmodic medications reduce bowel spasms, and pain relievers like acetaminophen ease pain.
Always follow the recommended dosage and talk to a healthcare provider before taking any medication.
Staying Hydrated
Drinking enough water is vital in managing diverticulitis symptoms. It helps soften stool and prevents constipation.
- Water intake should increase, even more, when eating high-fiber foods.
- Also, avoid caffeine and alcohol as they can dehydrate you.
The Role of Antibiotics in Treatment
Antibiotics are key in treating diverticulitis, mainly in severe cases. This condition, an inflammation of the digestive tract, can cause bacterial infections. We’ll look at when antibiotics are needed and the types used.
When are Antibiotics Necessary?
Antibiotics are given for diverticulitis when a bacterial infection is suspected or confirmed. The choice depends on the severity of symptoms and the patient’s health. For mild cases, diet changes and monitoring might be enough. But for severe symptoms or signs of infection, antibiotics are vital.
Key indicators for antibiotic use include:
- Presence of fever
- Significant abdominal pain or tenderness
- Evidence of abscesses or perforation
- Failure to improve with conservative management
Types of Antibiotics Commonly Prescribed
The type of antibiotic depends on the infection’s severity, patient allergies, and other medications. Common antibiotics for diverticulitis are:
- Ciprofloxacin and Metronidazole: Effective against many bacteria.
- Amoxicillin-clavulanate: Covers a wide range of bacteria.
- Piperacillin-tazobactam: Used in severe cases or when complications are a risk.
It’s important to finish all antibiotics, even if symptoms get better before finishing. This ensures the infection is fully treated and prevents antibiotic resistance.
Dietary Modifications for Long-Term Management
Managing diverticulitis long-term requires a few steps, with diet being key. What we eat affects symptoms and flare-ups. Making smart food choices can lower risks and improve life quality.
Foods to Include in Your Diet
Adding the right foods to your diet helps with diverticulitis. High-fiber foods are great because they soften and move food. This reduces pressure on the diverticula.
- Fruits such as apples, bananas, and berries
- Vegetables like broccoli, carrots, and leafy greens
- Whole grains including brown rice, quinoa, and whole-wheat bread
- Legumes such as beans, lentils, and peas
These foods are not just high in fiber. They also have important nutrients. A study found that a fiber-rich diet helps prevent diverticulitis. It keeps bowel movements regular and prevents constipation.
American Journal of Gastroenterology
Foods to Avoid During Flare-Ups
When you’re having a flare-up, change your diet to feel better. Some foods can make symptoms worse. It’s best to avoid them until you’re feeling better.
Foods to Avoid | Reason |
Nuts and seeds | Can be difficult to digest and may irritate the diverticula |
High-fat foods | Can slow digestion and worsen symptoms |
Processed meats | Low in fiber and high in unhealthy fats and preservatives |
The Benefits of Fiber
Fiber is key for managing diverticulitis. It softens stool, reduces pressure, and promotes regular bowel movements. A high-fiber diet can also prevent future flare-ups.
Increasing fiber intake should be done slowly. Sudden increases can cause discomfort like gas and bloating. Drinking more water helps fiber move through your system.
Understanding diet’s role in managing diverticulitis is important. Making the right dietary changes can help manage symptoms and improve overall health.
When to Seek Medical Attention
It’s vital to know when to get medical help for diverticulitis. This condition can get worse if not treated right away. So, it’s key to know when to act fast.
Severe Symptoms to Watch For
Some symptoms mean you need to see a doctor right away. These include:
- Severe abdominal pain that doesn’t get better or gets worse.
- Fever over 101°F (38.3°C).
- Vomiting or trouble keeping fluids down.
- Blood in the stool or black, tarry stools.
- Abdominal tenderness or muscle tension.
If you notice any of these signs, you should get medical help fast.
Potential Complications of Untreated Diverticulitis
Not treating diverticulitis can cause serious problems. These include:
Complication | Description |
Abscess Formation | A pocket of pus in the colon wall. |
Perforation | A hole in the colon wall that can cause peritonitis. |
Peritonitis | Inflammation of the abdominal lining, often from a perforation. |
Fistula | An abnormal connection between the colon and another organ or skin. |
Stricture | Narrowing of the colon that can block the bowel. |
Knowing these risks shows why it’s so important to get help if symptoms are severe.
Non-Surgical Treatments for Diverticulitis
Non-surgical treatments are key in managing diverticulitis. They help ease symptoms, prevent complications, and improve life quality for patients.
Lifestyle Changes and Their Impact
Making lifestyle changes is vital in treating diverticulitis. Dietary adjustments are a big part of this, focusing on more fiber to soften stool and ease pressure. Regular exercise is also important, as it helps with bowel movements and digestive health.
Staying hydrated is another key point. Drinking enough water helps prevent constipation by making stool softer and easier to pass. This can greatly lower the chance of diverticulitis flare-ups.
Probiotics and Gut Health
Probiotics are getting attention for their benefits in managing diverticulitis. These live bacteria and yeasts help keep the gut healthy by balancing gut flora. Studies show they may reduce inflammation and improve symptoms in diverticulitis patients.
You can add probiotics to your diet with foods like yogurt, kefir, and fermented veggies, or with supplements. But, always talk to a healthcare provider before starting any new supplements to make sure they’re safe for you.
By using these non-surgical treatments, patients with diverticulitis can manage their condition better and lower the risk of complications. This approach combines lifestyle changes with medical advice to improve health outcomes.
Surgical Options for Severe Cases
We suggest surgery for those with severe diverticulitis who haven’t gotten better with other treatments. It’s a last resort but sometimes it’s needed to avoid more problems.
Indications for Surgery
If you have severe symptoms like intense pain, a lot of bleeding, or signs of peritonitis, surgery might be needed. Also, if you keep getting diverticulitis or have complications like abscesses or fistulas, surgery is a good option.
Choosing surgery depends on your health, how bad your condition is, and how you’ve reacted to other treatments.
Indication | Description |
Severe Symptoms | Intense abdominal pain, significant bleeding, or signs of peritonitis |
Recurrent Diverticulitis | Frequent episodes of diverticulitis |
Complications | Abscesses, fistulas, or other complications |
Types of Surgical Procedures
There are several ways to treat diverticulitis with surgery:
- Primary Resection and Anastomosis: This involves removing the affected part of the colon and joining the healthy parts back together.
- Hartmann’s Procedure: A two-step process where the bad part of the colon is taken out. Then, the colon is either brought to the surface (colostomy) or fixed in a second surgery.
- Laparoscopic Surgery: A less invasive method using small cuts and a camera. It can help you recover faster.
The type of surgery you get depends on how bad your diverticulitis is, if you have complications, and your overall health.
Lifestyle Changes for Prevention
Making smart lifestyle choices can help prevent diverticulitis and boost gut health. By adding certain habits to your daily routine, you can lower your risk of getting this condition.
Regular Exercise
Keeping your digestive system healthy is key. Exercise helps move your bowels, improves gut movement, and boosts gut health.
- Types of Exercise: Aerobic exercises, like walking, cycling, and swimming, are great.
- Frequency: Try to do at least 30 minutes of moderate exercise every day.
Research shows that regular exercise can cut down diverticulitis risk. It does this by making gut movement better and lowering digestive tract pressure.
Exercise Type | Benefits for Diverticulitis Prevention |
Aerobic Exercise | Improves gut motility, reduces pressure on the digestive tract |
Strength Training | Enhances overall physical health, improves gut health |
Managing Stress
Long-term stress can harm your gut health and up your risk of diverticulitis. It’s vital to manage stress well to prevent this condition.
- Meditation and Mindfulness: These practices can lower stress levels.
- Yoga: It’s a mix of physical activity and stress-reducing techniques, making it great for health.
By managing stress well, you can keep your gut healthy and lower your risk of diverticulitis.
The Connection Between Diverticulitis and Aging
Aging plays a big role in getting diverticulitis. It affects how often and how severe it is. Knowing how aging changes our digestive system helps us prevent and manage this condition.
Changes in Digestive Health with Age
As we get older, our digestive system changes. It can move food slower, have less blood flow, and have different bacteria. These changes can lead to diverticula, which can get inflamed or infected, causing diverticulitis.
Key Changes in the Digestive System with Age:
- Decreased muscle tone and motility in the intestines
- Reduced blood flow to the digestive tract
- Alterations in gut microbiota
- Increased pressure on the walls of the colon
A study in the Journal of Clinical Gastroenterology found that diverticulitis gets more common with age. Most cases happen after 50. This shows how important age is in getting diverticulitis.
“The aging population is more susceptible to diverticular disease due to age-related changes in the colon, including increased intral colonic pressure and decreased colonic motility.”
– Journal of Clinical Gastroenterology
Prevention Strategies for Older Adults
Even though age is a risk factor, there are ways to lower the risk of diverticulitis. Older adults can make dietary changes, adopt a healthy lifestyle, and get regular check-ups.
Prevention Strategy | Description | Benefits |
Increased Fiber Intake | Consuming a diet rich in fiber | Reduces the risk of diverticulitis by promoting regular bowel movements |
Regular Exercise | Engaging in physical activity regularly | Improves bowel habits and reduces pressure on the colon |
Adequate Hydration | Drinking plenty of water | Softens stool and promotes regular bowel movements |
By following these prevention strategies, older adults can lower their risk of diverticulitis. This helps them manage their digestive health better.
Living with Diverticulitis: Patient Stories
Patient stories show how people deal with diverticulitis in different ways. They share tips on managing symptoms. Living with diverticulitis is a journey of trying new things to find what works best.
Many people are surprised when they find out they have diverticulitis. It often starts with severe pain or changes in bowel habits. Knowing about the condition is the first step to managing it well.
Personal Experiences with Treatment
Everyone’s experience with diverticulitis treatment is different. Some find relief with diet changes, while others need antibiotics or surgery. It shows how varied the condition can be.
“I was diagnosed with diverticulitis after years of experiencing intermittent abdominal pain. Through trial and error, I found that a high-fiber diet significantly reduced my symptoms.”age 42
Tips from Those Who Manage It
Managing diverticulitis well involves lifestyle changes, diet, and sometimes medical help. Here are tips from those who live with it:
- Stay hydrated: Drinking lots of water is key for digestive health. It helps prevent constipation, a common cause of flare-ups.
- Monitor your diet: Eating a high-fiber diet helps, but it’s also important to know which foods can trigger flare-ups.
- Exercise regularly: Being active improves digestion and lowers the risk of complications from diverticulitis.
- Manage stress: Stress can affect your digestion. Techniques like meditation or yoga can help manage stress.
By sharing their stories, people with diverticulitis help others facing similar challenges. Their experiences show the value of a complete approach to managing diverticulitis. This includes diet, lifestyle changes, and medical treatment when needed.
Frequently Asked Questions on Diverticulitis
We’ve talked a lot about diverticulitis. Now, let’s tackle some common questions and myths. Knowing the facts about diverticulitis can help you understand its chronic nature and how it impacts people.
Addressing Misconceptions
Many think a low-fiber diet causes diverticulitis. But, the truth is, we don’t know for sure what causes it. Another myth is that diverticulitis is rare. But, it’s actually quite common in older adults.
The Chronic Aspect
Diverticulitis can come back, and knowing this is key to managing it. Some people get flare-ups often, while others go long periods without symptoms. It’s important to recognize when a flare-up is happening and how to handle it.
Understanding diverticulitis helps people make better choices about their treatment. We hope this info has answered your questions and eased your worries about diverticulitis.
FAQ
What is diverticulitis, and how does it differ from diverticulosis?
Diverticulitis is when the diverticula in the colon wall get inflamed. Diverticulosis is when you have diverticula but no inflammation. Knowing the difference is key to managing it right.
What are the common symptoms of diverticulitis?
Symptoms include stomach pain, changes in bowel habits, fever, and nausea. Spotting these signs early is important for getting medical help fast.
How is diverticulitis diagnosed?
Doctors use a physical exam, CT scans, and sometimes endoscopy to diagnose it. These tests confirm if you have diverticulitis.
What dietary changes can help manage diverticulitis symptoms?
Eating more fiber, drinking plenty of water, and avoiding certain foods can help. A diet rich in fiber is great for managing diverticulitis over time.
When are antibiotics necessary for treating diverticulitis?
Antibiotics are needed for moderate to severe cases. They’re also used when there’s a high risk of complications or symptoms don’t go away.
Can lifestyle changes help prevent diverticulitis flare-ups?
Yes, regular exercise, managing stress, and a balanced diet can help prevent flare-ups. These changes can also help manage the condition well.
What are the signs that indicate the need for immediate medical attention?
Severe stomach pain, high fever, vomiting, and rectal bleeding are signs to see a doctor right away. They can prevent serious problems.
How does aging affect the risk of developing diverticulitis?
The risk of diverticulitis goes up with age, after 40. Older people should watch for symptoms and take steps to prevent it.
Are there any natural remedies that can help manage diverticulitis?
While medical treatment is key, natural remedies like probiotics and herbal supplements can help. A high-fiber diet also supports gut health and eases symptoms.
Can diverticulitis be cured, or is it a chronic condition?
Diverticulitis can be managed with treatment, but it often comes back. Understanding it’s a chronic condition helps in finding long-term ways to manage it.
What role do probiotics play in managing diverticulitis?
Probiotics help keep the gut healthy, reduce inflammation, and ease symptoms. They’re a good supplement for those with diverticulitis.
When is surgery considered for diverticulitis treatment?
Surgery is an option for severe cases, when treatments don’t work, or for those with many episodes. The decision depends on how severe and frequent the episodes are.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30537746/