Geriatrics addresses the health needs of older adults, focusing on frailty, dementia, falls, and chronic disease management.
Send us all your questions or requests, and our expert team will assist you.
Geriatrics is the branch of medicine dedicated to the health care of elderly people. It aims to promote health by preventing and treating diseases and disabilities in older adults. While there is no specific age that defines “old,” geriatrics typically focuses on adults aged 65 and older, particularly those over 80 or those navigating complex, overlapping health conditions. A physician who specializes in this field is called a Geriatrician.
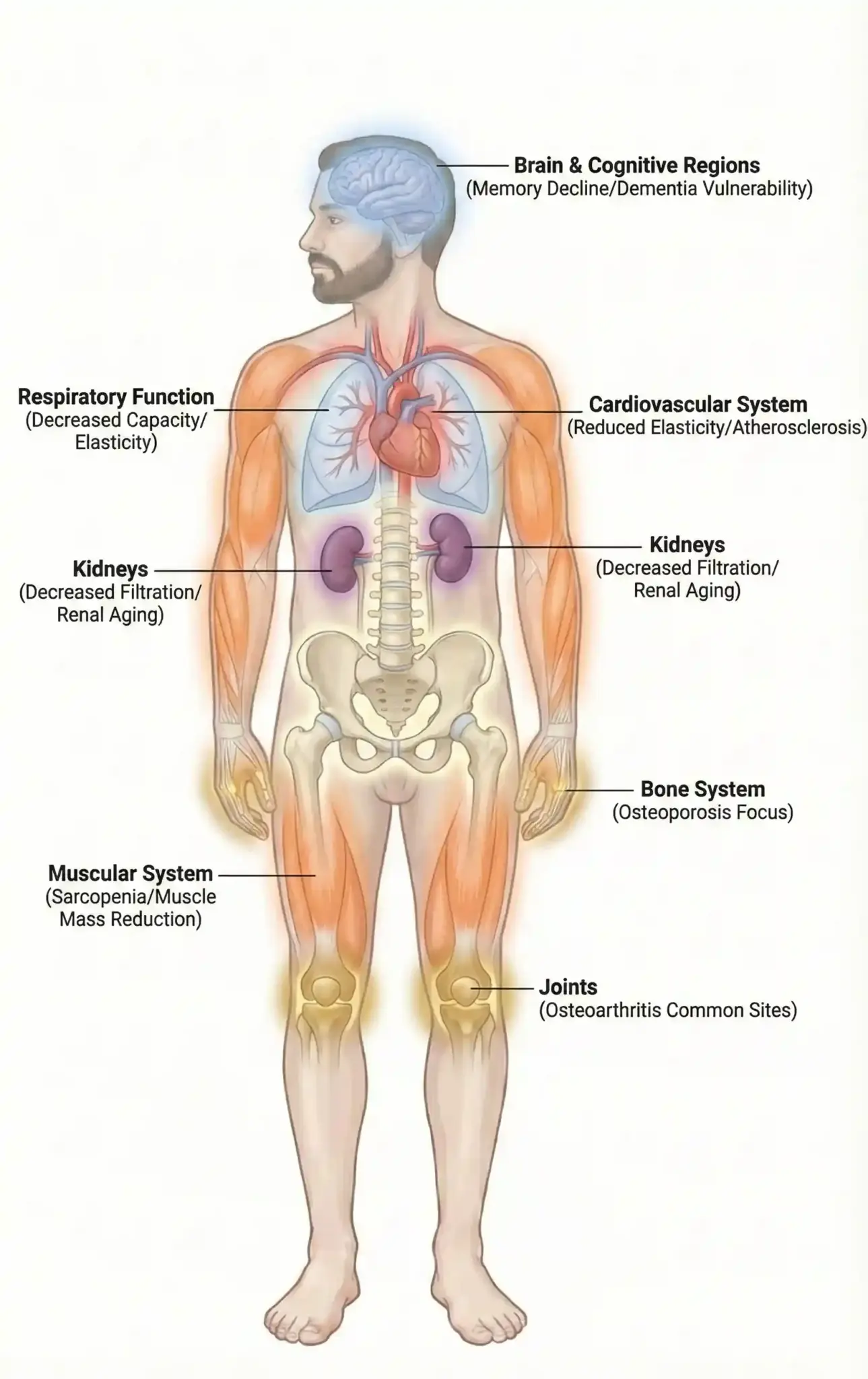
The human body undergoes a complex series of changes over time. This natural progression affects every cell, tissue, and organ system. Understanding these biological shifts is the foundation of specialized care for older adults.
Aging is not merely a decline in function but a remodeling of physiological processes. The reserve capacity of organs gradually diminishes, making the body more susceptible to stress and illness. This reduced ability to bounce back is a key concept in elder care.
Medical professionals in this field study the difference between normal aging and disease. While wrinkles and gray hair are visible signs, internal changes are far more significant. The elasticity of blood vessels decreases, metabolism slows, and the immune system becomes less robust.

When patients ask what geriatrics is, they are inquiring about the branch of medicine dedicated to the health care of elderly people. It focuses on the unique needs of the aging population, distinguishing itself from adult internal medicine.
This specialty emphasizes the maintenance of function and quality of life. It acknowledges that older adults often have multiple chronic conditions. The goal is not just to treat individual diseases but to optimize the patient’s overall well-being.
Practitioners in this field are trained to navigate complex medical situations where standard treatment protocols may not apply. They prioritize patient preferences and consider the impact of treatments on daily living.

The geriatrics definition extends beyond clinical diagnosis to encompass a philosophy of holistic care. It recognizes that an older adult’s health is influenced by physical, mental, social, and environmental factors.
This approach moves away from a disease-centered model to a person-centered model. It considers how a condition affects the patient’s ability to live independently and interact with their community.
Care plans are tailored to align with the patient’s values and goals. Whether the objective is to walk without pain or to maintain cognitive clarity, the medical strategy is adjusted accordingly.
The world is experiencing a significant demographic shift with a rapidly aging population. This trend highlights the growing importance of geriatric medicine in the global healthcare landscape.
As life expectancy increases, the prevalence of age-related conditions rises. Healthcare systems must adapt to manage the complex needs of this expanding demographic.
This shift necessitates a greater number of healthcare providers skilled in elder care. It also drives innovation in how care is delivered, from home-based services to specialized hospital units.

A geriatrician, often called a geriatrics doctor, is a primary care physician or internist who has completed additional training in the care of older adults. They serve as the quarterback of the healthcare team.
These specialists are experts in managing multimorbidity, which is the presence of two or more chronic medical conditions. They are skilled in prioritizing treatments to avoid adverse drug interactions.
They also play a crucial role in coordinating care among various specialists. This prevents fragmented care and ensures that all treatments work together harmoniously.
Senescence is the biological process of aging. It involves molecular and cellular changes that accumulate over time. These changes lead to a gradual loss of physiological integrity.
One of the hallmarks of senescence is genomic instability. Over time, DNA damage accumulates, and the body’s repair mechanisms become less efficient. This contributes to the risk of cancer and other diseases.
Mitochondrial dysfunction is another key factor. As the power plants in cells become less efficient, energy production declines, and oxidative stress increases. This affects tissues with high energy demands, such as the heart and brain.
Frailty is a clinical state of increased vulnerability. It is characterized by a decline in reserve and function across multiple physiological systems. This leaves the individual less able to cope with everyday or acute stressors.
It is distinct from disability and comorbidity, although they often overlap. Frailty is a dynamic condition that can often be managed or even reversed with appropriate interventions.
Identifying frailty is essential for risk stratification. Frail older adults are at higher risk for falls, hospitalization, and adverse outcomes from surgery.
Send us all your questions or requests, and our expert team will assist you.

Brain health is a central concern in geriatrics, meaning and practice. While some cognitive changes are a regular part of aging, significant memory loss is not. Distinguishing between benign forgetfulness and dementia is a critical skill.
The aging brain undergoes structural changes, including a slight decrease in volume and alterations in neurotransmitter levels. However, the brain retains plasticity, the ability to adapt and form new connections.
Preserving cognitive function involves managing cardiovascular risk factors, engaging in mental stimulation, and maintaining social connections.
Aging affects all the sensory systems, influencing how older adults interact with their environment. Vision changes often include presbyopia and a need for more light. Hearing loss, particularly high-frequency hearing loss, is common.
Decreased taste and smell can affect appetite and nutrition. Changes in touch and proprioception can impact balance and increase the risk of falls.
Addressing these sensory deficits is vital to maintaining independence and safety. Simple interventions such as hearing aids or improved lighting can make a profound difference.
Immunosenescence describes the gradual deterioration of the immune system. This makes older adults more susceptible to infections and less responsive to vaccinations.
The body produces fewer new immune cells, and existing cells become less effective at recognizing new threats. This contributes to the severity of illnesses like influenza and pneumonia in this population.
Chronic low-grade inflammation, often termed “inflammaging,” is also characteristic of aging. This persistent inflammation contributes to the development of chronic diseases such as atherosclerosis and diabetes.
The way the body processes drugs changes with age. Pharmacokinetics, which includes absorption, distribution, metabolism, and excretion, is altered. This makes older adults more sensitive to medications.
Kidney and liver function naturally decline, slowing the clearance of drugs from the body. This increases the risk of toxicity and side effects.
Medication management is a cornerstone of the specialty. Physicians must carefully weigh the benefits and risks of every drug prescribed.

Health in older age is deeply intertwined with social and environmental factors. Social isolation and loneliness are significant health risks, comparable to smoking or obesity.
The living environment plays a crucial role in safety and independence. Factors such as stairs, lighting, and access to transportation can determine whether an older adult can age in place.
Understanding the patient’s support system and living situation is essential for creating a realistic and practical care plan.
Ethical considerations are frequently at the forefront of elder care. Issues such as decision-making capacity, advance directives, and end-of-life care require sensitivity and legal knowledge.
Respecting patient autonomy while ensuring safety is a delicate balance. Physicians often facilitate conversations about goals of care to ensure treatments align with the patient’s wishes.
These discussions often involve family members and surrogates. Navigating these complex dynamics is a key skill for the specialist.
The gold standard of care is the Comprehensive Geriatric Assessment (CGA). This is a multidimensional diagnostic process used to determine the medical, psychosocial, and functional capabilities of a frail older person.
It involves a team of health professionals and goes far beyond a standard medical exam. The goal is to develop a coordinated and integrated plan for treatment and long-term follow-up.
The CGA has been proven to improve survival and function in older adults. It is the practical application of the field’s holistic philosophy.
Research in the biology of aging is advancing rapidly. Scientists are exploring ways to target the fundamental processes of aging to extend the healthspan, the period of life spent in good health.
Defining geriatrics in the future will likely include the use of geroprotectors, drugs that delay the aging process. Technology will also play a larger role, from wearable monitors to smart homes that support independence.
The field is evolving from managing decline to actively promoting vitality and resilience in later life.

Geriatrics works closely with palliative care principles.

Aging is a journey that deserves dignity, respect, and expert guidance. At Liv Hospital, our Geriatrics Department provides a “Medical Home” for older adults. We understand that our patients have lived full lives and have unique stories. Our medical approach is designed to honor that history by providing care that adds life to years, not just years to life.
In geriatrics, the family is often the patient’s voice.
At Liv Hospital, we believe that aging is not a disease to be cured, but a stage of life to be optimized. We are dedicated to helping our seniors live their golden years with strength, clarity, and independence.
There is no specific age that automatically places someone in this category. Still, patientsare typically age 65 and older, with a focus on those over 75 or those with multiple complex health conditions.
Many insurance plans require a referral from a primary care physician to see a specialist, but it is best to check with your specific insurance provider and the specialist’s office.
A geriatrician has specialized training in the unique health needs of older adults, focusing on maintaining independence, managing multiple medications, and treating conditions common to aging,l ike dementia and falls.
Yes, a geriatrician often works alongside your other specialists, such as cardiologists or neurologists, to coordinate your care and ensure all treatments work well together.
While these specialists manage complex illnesses, they also focus on preventative care and healthy aging for active older adults who want to maintain their current level of health and function.


In medical emergencies, O-negative blood is very important. It can be given to anyone because it matches all blood types. This rare blood type is

Many think urologists mainly help men. But, the truth is more complex. Urology is a branch of medicine that deals with disorders and diseases of


Understanding your options for dental fillings is key to good dental health. It helps you make smart choices about your teeth.types of fillings dentist25 Types

Over 1.7 million PET scans are done every year in the United States. They help doctors find and treat many health issues, including pet scan

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)