Accurate skin diagnosis prevents future complications. Learn about our diagnostic tools, from routine skin exams and biopsies to advanced digital mole mapping.
Send us all your questions or requests, and our expert team will assist you.
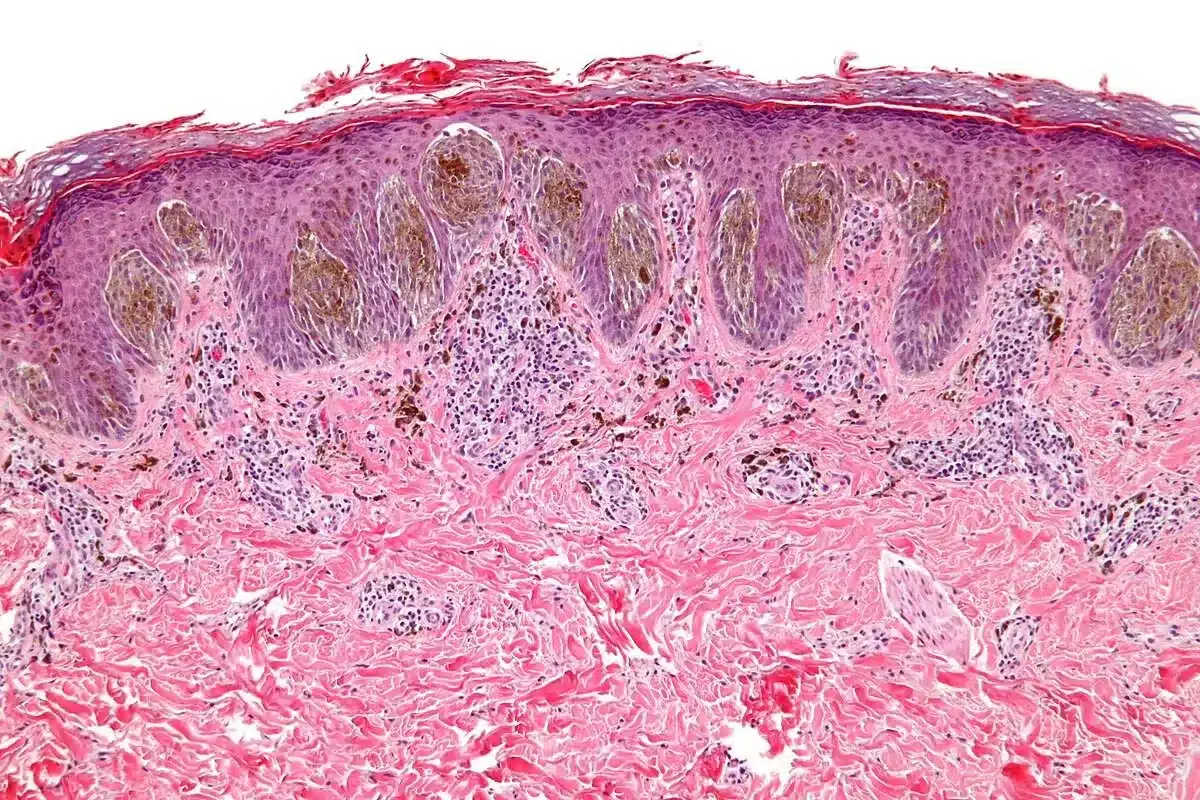
The foundation of dermatological diagnosis is the visual inspection of the skin. A thorough full-body skin exam involves checking every inch of the skin, from the scalp to the soles of the feet and between the toes.
Good lighting is essential for this process. Physicians often use a dermatoscope, a handheld device that provides magnification and polarized light, to see pigment structures and vessel patterns invisible to the naked eye.
This exam screens for skin cancer, changing moles, and other abnormalities. It also allows the doctor to assess the distribution and pattern of rashes, which provides critical diagnostic clues.

A detailed medical history provides the context for physical findings. The physician asks about the duration of the problem, associated symptoms like itching or pain, and potential triggers.
Family history is crucial for conditions like melanoma, psoriasis, and eczema. Medication history helps identify drug-induced skin reactions. Lifestyle factors, such as sun exposure and occupation, are also reviewed.
Understanding the patient’s skincare routine and product use can reveal causes of contact dermatitis or acne. This conversation builds a complete clinical picture.

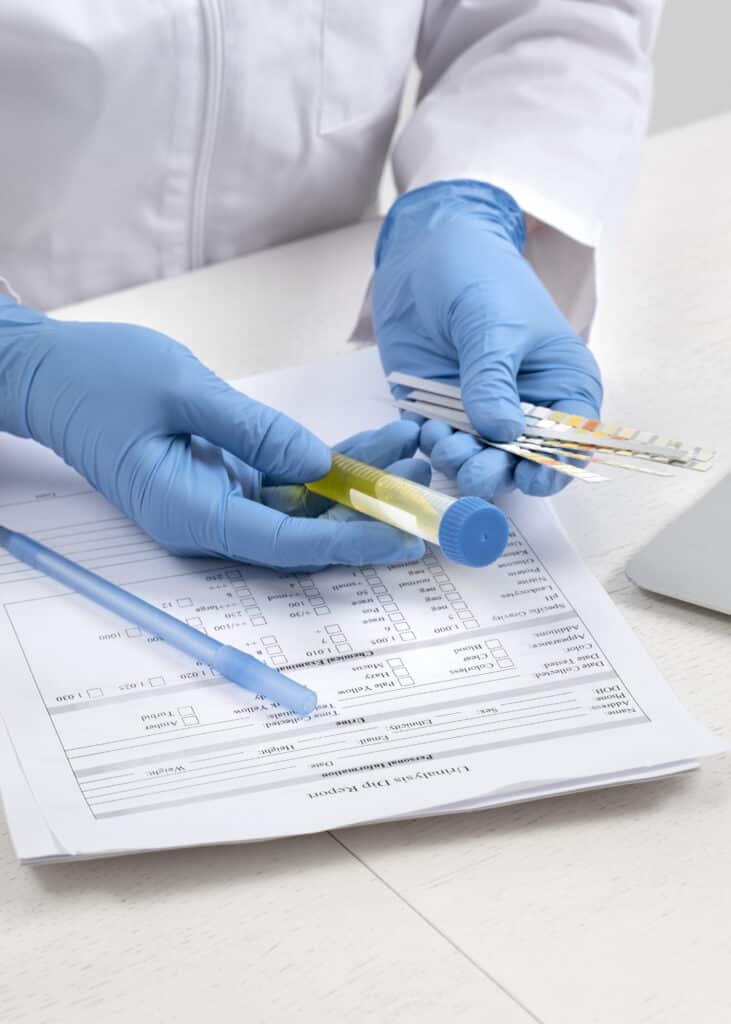
When a diagnosis cannot be made solely by observation, a skin biopsy is performed. This involves removing a small skin sample for microscopic examination by a pathologist.
A shave biopsy removes the top layers of skin and is used for superficial lesions. A punch biopsy uses a circular tool to remove a core of tissue, including deeper layers, which is helpful for rashes and inflammatory conditions.
An excisional biopsy removes the entire lesion and is the standard for suspected melanoma. The type of biopsy chosen depends on the suspected condition and the location.
Patch testing is the gold standard for diagnosing allergic contact dermatitis. Small amounts of potential allergens are applied to patches, which are then placed on the patient’s back.
The patches remain in place for 48 hours. The patient returns to have them removed, and the skin is evaluated for reactions. A second reading is often performed a few days later to detect delayed reactions.
This test helps identify triggers like nickel, fragrances, preservatives, and rubber accelerators found in everyday products. Avoiding identified allergens is curative.
To diagnose fungal infections, a KOH (potassium hydroxide) preparation is used. Skin scrapings, hair, or nail clippings are placed on a slide with KOH solution, which dissolves skin cells but leaves fungal elements intact.
Under a microscope, the physician looks for hyphae (branching filaments) or spores. This rapid, in-office test can confirm conditions like athlete’s foot, ringworm, or tinea versicolor.
It distinguishes fungal infections from other conditions, such as eczema or psoriasis, that may look similar but require different treatments.
A Wood’s lamp emits ultraviolet light (black light). When illuminated in a dark room, certain bacteria, fungi, and pigment changes fluoresce in specific colors.
This tool helps diagnose scalp fungal infections (tinea capitis) and bacterial infections such as erythrasma. It also highlights pigment disorders like vitiligo and melasma, showing the extent of pigment loss or deposition.
It is a non-invasive and painless diagnostic aid that provides immediate information about the nature of skin lesions.

Send us all your questions or requests, and our expert team will assist you.
A Tzanck smear is used to diagnose viral infections like herpes simplex and varicella zoster (shingles). A vesicle is unroofed, and the fluid and base are scraped onto a slide.
After staining, the sample is examined for multinucleated giant cells, which are characteristic of herpes virus infections. While less common now due to PCR testing, it remains a quick, low-cost diagnostic tool.
It provides immediate confirmation of a viral cause of blistering eruptions, enabling prompt antiviral therapy.
Dermoscopy involves using a specialized magnifier with lighting to examine skin lesions. It allows visualization of subsurface structures that are not visible to the naked eye.
It significantly increases the accuracy of diagnosing melanoma and other skin cancers. Specific patterns of pigment network, dots, and globules help distinguish benign moles from malignant ones.
Dermoscopy is also used to evaluate hair disorders and nail pigmentation. It reduces the need for unnecessary biopsies of benign lesions.
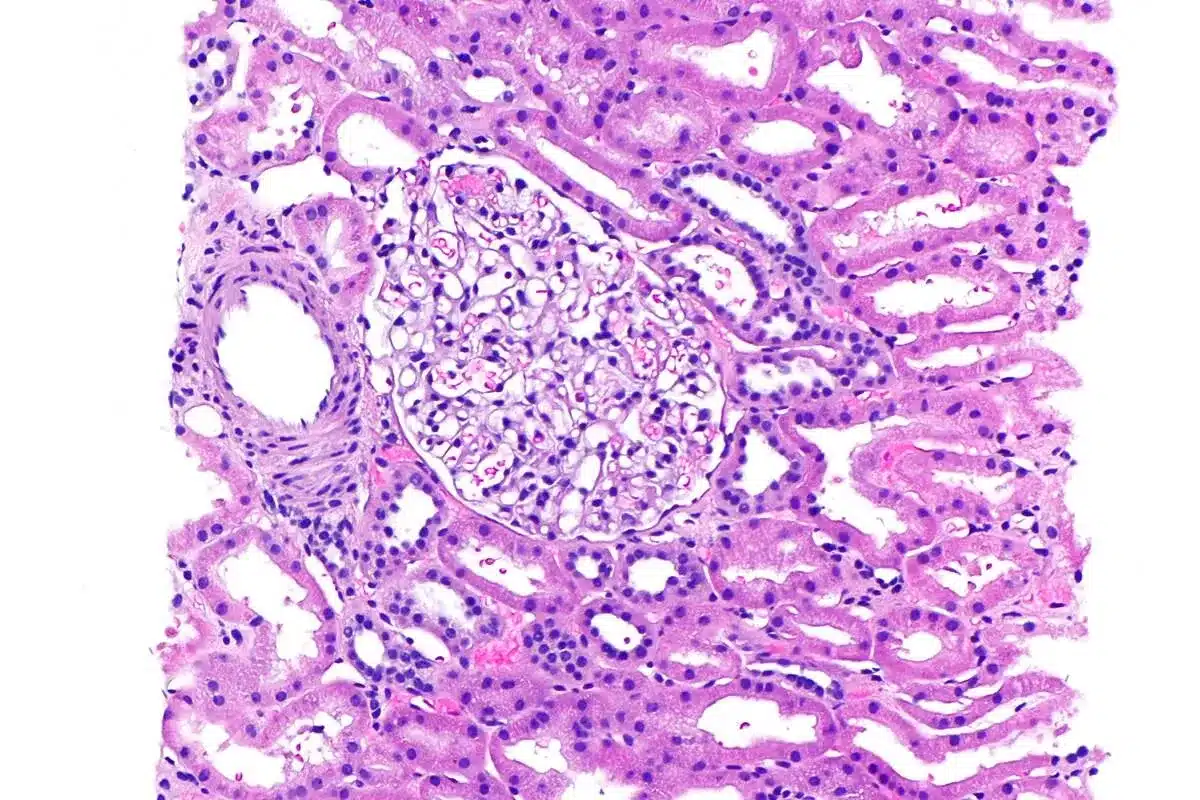
While dermatology focuses on the skin, blood tests are often necessary to evaluate underlying systemic causes. Autoimmune panels (ANA) screen for lupus and dermatomyositis.
Hormonal panels check for androgen excess in acne or hair loss. Thyroid function tests evaluate dry skin or hair changes. Complete blood counts and metabolic panels monitor the safety of systemic medications.
Serologic testing can diagnose syphilis or Lyme disease presenting with skin rashes. Integrating lab data with skin findings leads to a comprehensive diagnosis.
If a bacterial infection is suspected, a swab of the pus or fluid is taken for culture. This identifies the specific bacteria causing the disease, such as Staphylococcus aureus.
Sensitivity testing determines which antibiotics are effective against the identified bacteria. This is crucial for treating methicillin-resistant Staphylococcus aureus (MRSA) and ensuring the correct antibiotic is prescribed.
It guides treatment for conditions such as impetigo, folliculitis, and infected eczema, helping prevent treatment failure and resistance.
Patients often start their journey by searching for dermatology near them or dermatology providers in their insurance network. Finding a board-certified provider is essential for an accurate diagnosis.
Clinics labeled as advanced dermatology often have access to specialized equipment, such as phototherapy units or Mohs surgery labs. Complete dermatology centers may offer both medical and cosmetic services under one roof.
Researching a provider’s credentials and patient reviews helps ensure the chosen specialist has the expertise relevant to the patient’s specific condition.
For rare or hereditary skin disorders, genetic testing may be indicated. This can confirm diagnoses of conditions like ichthyosis, epidermolysis bullosa, or neurofibromatosis.
Genetic testing is also becoming more relevant in melanoma management. Gene expression profiling can help predict metastatic risk in diagnosed melanomas.
This information aids in counseling families about recurrence risks and informs the intensity of surveillance and treatment required.
To evaluate hair loss, a hair pull test is performed. The physician gently pulls on a bundle of hair to see how many are actively shedding. This helps distinguish shedding disorders from breakage.
Trichoscopy uses a dermatoscope to examine the scalp and hair shafts. It reveals signs like hair diameter variability, empty follicles, or specific inflammatory patterns.
These non-invasive tools help differentiate between androgenetic alopecia, alopecia areata, and scarring alopecias, guiding appropriate therapy.
For patients with many moles or a high risk of melanoma, digital mole mapping is used. High-resolution full-body photography documents the patient’s skin surface.
Software can track changes in moles over time or identify new lesions. This surveillance method enables early detection of subtle changes that might be missed during a standard exam.
It reduces patients’ anxiety with atypical mole syndrome by providing an objective record of their skin.
Complex cases may require referral to sub-specialists. Dermatology consultants often focus on niche areas like contact dermatitis, cutaneous lymphoma, or pediatric dermatology.
Associates in dermatology practices often use a team approach, in which multiple colleagues review complex cases. This collaborative environment ensures that patients benefit from collective expertise.
Seeking a specialist ensures access to the most advanced diagnostic tools and the latest treatment protocols for challenging conditions.


No, a biopsy is a diagnostic tool used to determine what a skin lesion is; while it is used to rule out cancer, it is also used to diagnose rashes, infections, and benign growths.
Most dermatologists recommend an annual full-body skin exam for adults, but those with a history of skin cancer or numerous moles may need to be seen more frequently, such as every 6 months.
Coverage varies; while the medical exam is typically covered, the specific digital photography or automated mapping service may be considered an out-of-pocket expense depending on the plan.
The procedure involves a quick injection of local anesthetic, which causes a brief sting, but the actual removal of the skin sample is painless.
It is best to arrive with a clean face or remove makeup upon arrival, as makeup can mask skin color, texture, and subtle lesions, making an accurate diagnosis difficult.


how long does it take for a scab to heal Nearly 5 million people in the United States get surgical excisions every year. After such

ultraviolet radiation lamp Phototherapy, or light therapy, uses specific light wavelengths. It’s often used for jaundice in newborns and some skin issues. Studies show it’s

Over 1 in 5 Canadians will get cancer, says the Canadian Cancer Society. This shows how key accurate diagnosis is. But can a surgeon reliably
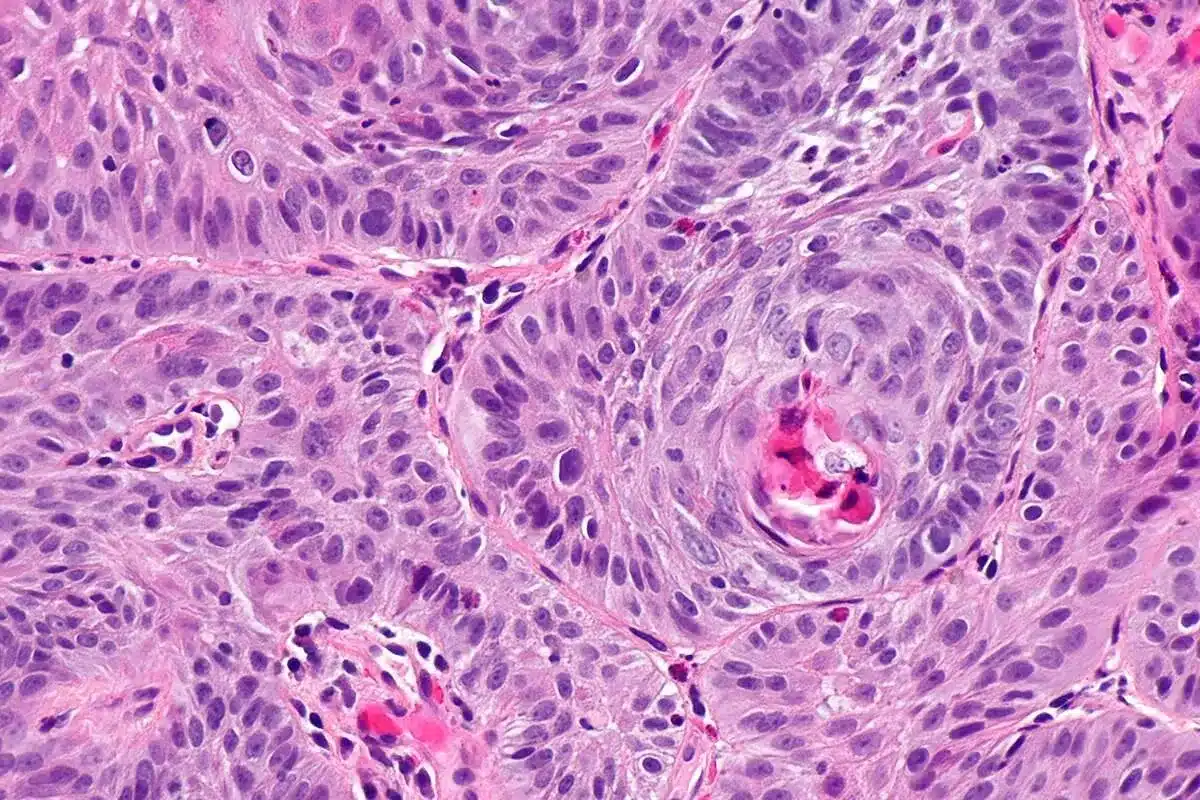
Squamous cell carcinoma is a common skin cancer found in thousands globally each year. It’s a big worry, as one in five Americans will get
Melanoma is a dangerous form of skin cancer. If caught early, it has a very good treatment outcome. The American Academy of Dermatology says the
Nearly 1.8 million new cancer cases are diagnosed every year in the United States. Biopsies are key in finding these cases. A biopsy means taking

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)