Recognize key heart symptoms like chest pain and shortness of breath. Understand major modifiable and non-modifiable Cardiology risk factors for adults.
Send us all your questions or requests, and our expert team will assist you.

Heart disease often develops quietly over many years, but there are usually warning signs before a major event occurs. Invasive cardiology is often brought into the picture when these symptoms start to interfere with daily life or when they suggest a dangerous blockage. Understanding these symptoms is crucial because the sooner you seek help, the more options doctors have to treat you. Ignoring symptoms allows the damage to accumulate, potentially weakening the heart muscle permanently.
Risk factors are the conditions or habits that make it more likely for you to develop heart disease. Some of these you can see, like a growing waistline, while others are hidden in your blood, like high cholesterol. An invasive cardiologist considers all these factors when deciding if a catheterization is necessary. They look at the whole picture—your history, your lifestyle, and your current complaints—to determine the probability of a blockage.

The most classic symptom that leads a patient to an invasive cardiologist is chest pain, medically known as angina. However, “pain” is not always the word patients use. Many describe it as a pressure, a squeezing sensation, a heaviness, or a tightness. It might feel like an elephant is sitting on your chest or like a tight band is wrapped around your ribs.
Stable angina is a type of chest discomfort that follows a predictable pattern. It usually happens when you make your heart work harder, such as when walking up a hill, carrying heavy groceries, or dealing with emotional stress. The narrowed arteries cannot supply enough blood to meet the increased demand.
Unstable angina is much more serious and is often a sign of an impending heart attack. This type of pain can happen while you are resting, sleeping, or watching TV. It means that blood flow is critically reduced, often by a blood clot that is forming and dissolving in the artery.

Not everyone gets chest pain. Many people, especially those with diabetes or heart failure, experience shortness of breath as their primary symptom. This is known as dyspnea. You might find that you get winded doing simple tasks that used to be easy, like making the bed or walking to the mailbox. This type of condition happens because the heart cannot pump enough blood to the body, or pressure builds up in the lungs.
Unexplained fatigue is another major red flag. This is not just being worn out after a long day; it is a profound exhaustion that feels like your battery has been drained. Patients often describe feeling like their limbs are heavy or that they need to nap frequently. This symptom is often overlooked or blamed on aging, but it can be a sign that the heart is struggling to deliver oxygen to the muscles.
Heart symptoms can be tricky because they can radiate to other parts of the body. The brain can confuse the source of pain because the heart’s nerves also serve other areas. Pain or discomfort in the neck, jaw, throat, upper abdomen, or back can actually be heart pain.
Women, in particular, often experience these “atypical” symptoms. Instead of the crushing chest pain, a woman might feel severe nausea, indigestion, or pain between the shoulder blades. Cold sweats are another common sign. Breaking out in a cold, clammy sweat without a fever or physical exertion is a classic sign that the body is in distress due to cardiac issues.
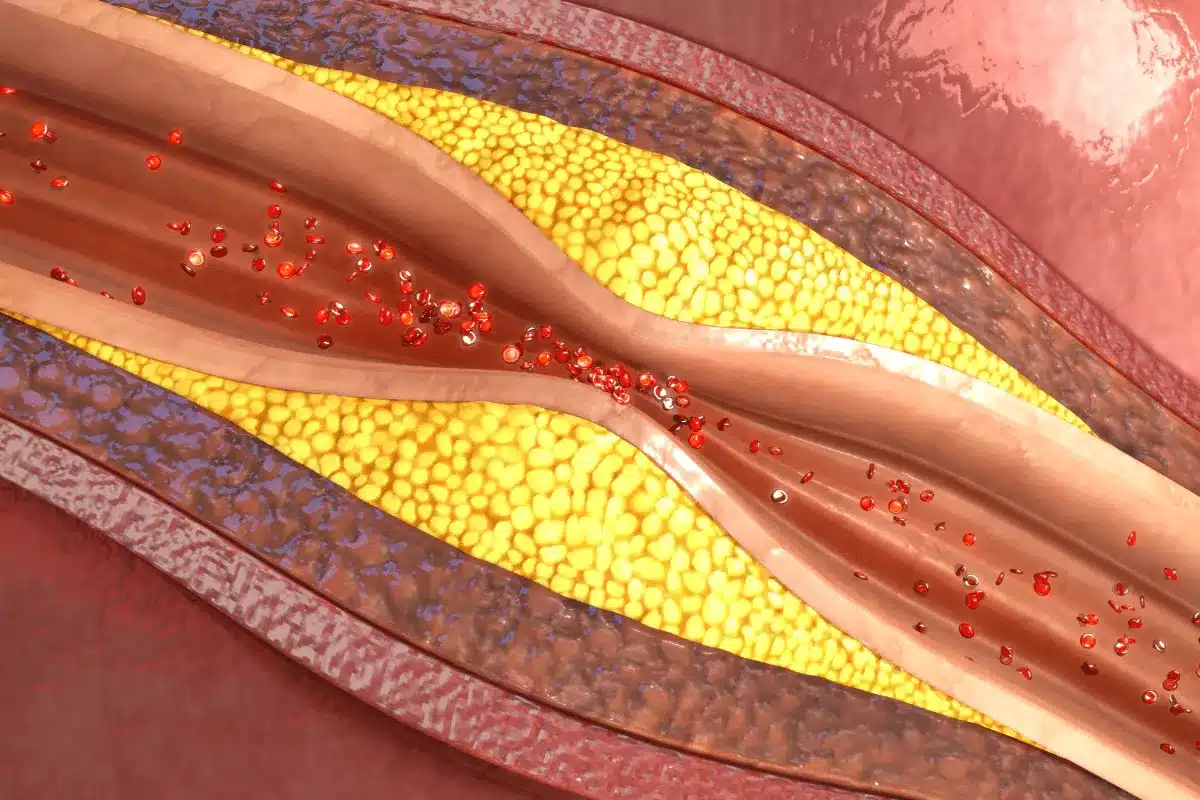
To understand why these symptoms happen, you need to understand atherosclerosis. This is the medical term for the hardening and narrowing of the arteries. It is a slow, complex disease that starts early in life and progresses over decades. It is the primary reason patients end up needing invasive cardiology procedures.
It begins when the inner lining of an artery is damaged by factors like smoking or high blood pressure. The body tries to repair this damage but ends up trapping cholesterol, fat, calcium, and other substances at the site. This mixture forms a bump called plaque. As the plaque grows, it takes up space inside the artery tube.
As plaque accumulates, the artery walls lose their elasticity. Healthy arteries are like rubber bands—they stretch and flex with each heartbeat. Diseased arteries become stiff like pipes. This stiffness forces the heart to pump harder to push blood through, raising blood pressure further and creating a vicious cycle of damage.

The good news is that many risk factors for heart disease are controllable. These are choices and environments that we can change. Smoking is perhaps the most significant risk factor for needing invasive procedures. The chemicals in tobacco smoke directly damage blood vessels and make blood more likely to clot.
Diet plays a massive role as well. A diet high in saturated fats, trans fats, sugar, and sodium accelerates plaque growth. Being overweight or obese puts extra strain on the heart and is often linked to other risks like diabetes and high blood pressure. A sedentary lifestyle, where one gets little to no exercise, weakens the heart muscle over time.

Some risks are written into our biology. Age is a major factor; simply getting older increases the risk of damaged arteries. Men are generally at higher risk at a younger age than women, though a woman’s risk increases sharply after menopause when natural protective hormones decline.
Family history is also a powerful predictor. If your parents or siblings had heart disease, especially at a young age, your genetic risk is higher. This doesn’t mean you’ll get heart disease, but you must be more careful than most. Genetics can influence how your body handles cholesterol and inflammation.
Send us all your questions or requests, and our expert team will assist you.
Angina is typically described as a pressure, squeezing, heaviness, or tightness in the center of the chest, rather than a sharp or stabbing pain.
High blood sugar levels over time damage the blood vessels and the nerves that control the heart, increasing the likelihood of developing atherosclerosis and silent heart disease.
Yes, genetic factors can increase your risk, especially if close male relatives developed heart disease before age 55 or female relatives before age 65.
Severe emotional stress can trigger a heart attack or a condition called broken heart syndrome by causing a surge of stress hormones that overwhelm the heart muscle.
Prolonged sedentary behavior slows down blood flow, reduces the body’s ability to process fats and sugars, and weakens the heart muscle over time.


Heart disease is the top killer worldwide. Thanks to new tech, cardiac catheterization is key in finding and fixing heart problems. This method lets us

Is cardiac catheterization needed if you have 50 percent blockage? Get vital answers. Learn when treatment is best to avoid dangerous risks. Artery blockage is
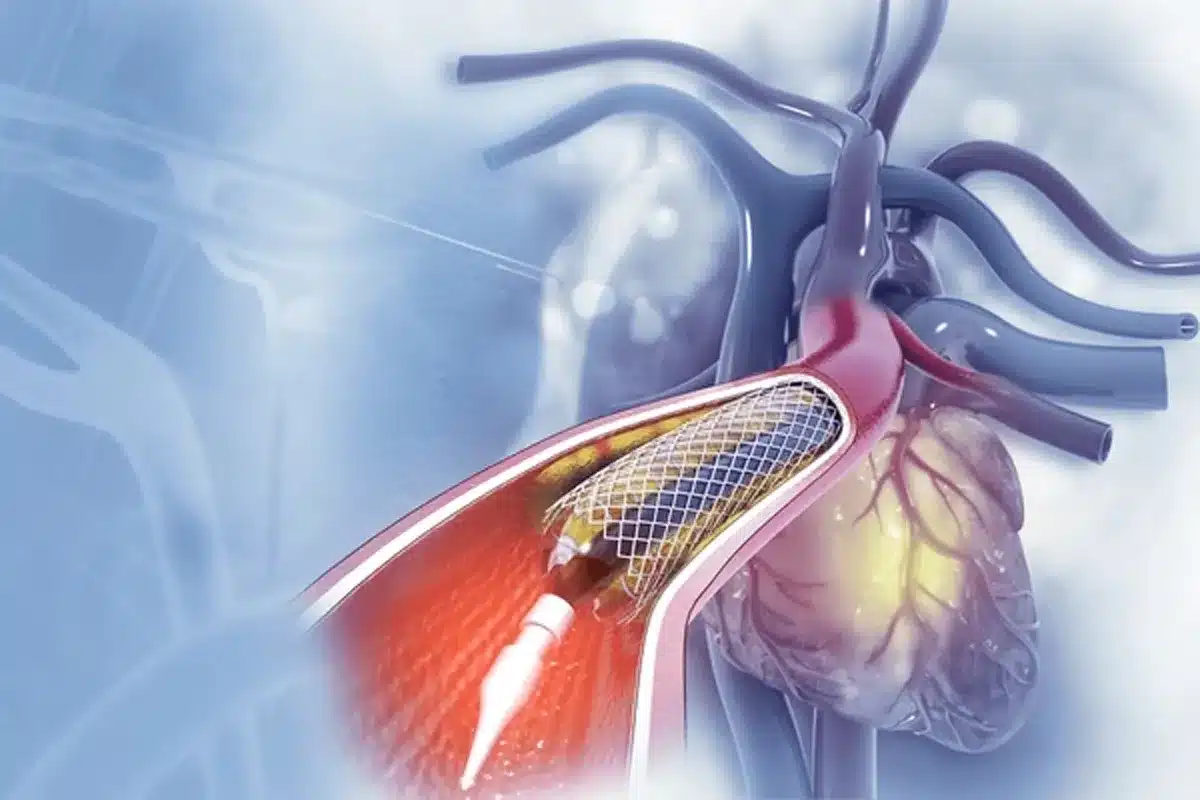
Steps of cardiac catheterization? Get best info here. From prep to recovery, understand this vital procedure to reduce anxiety and bad fear. Every year, over

Sleep for cardiac catheterization? Usually, twilight sedation is best. Avoid dangerous deep anesthesia risks while staying comfortable and calm. Having a cardiac cath can be

Recover from cardiac catheterization fast. Get best recovery tips. Most resume normal life in days! Learn how to ensure an amazing healing process. Having a

Is cardiac catheterization serious? It addresses vital health needs. While low risk, knowing the serious benefits is amazing for your peace of mind. Over a

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)