Essential guide to Stem Cell Recovery and Follow-up, including strict infection control, lifestyle changes, and long-term screening to prevent complications and recurrence.
Send us all your questions or requests, and our expert team will assist you.

The journey of a Thalassemia patient does not end with stem cell infusion. The recovery phase is a profound physiological and psychological transition. For a child or adult who has known only chronic illness, monthly hospital visits, and nightly chelation routines, the transition to a “cured” status requires careful medical management and lifestyle adaptation.
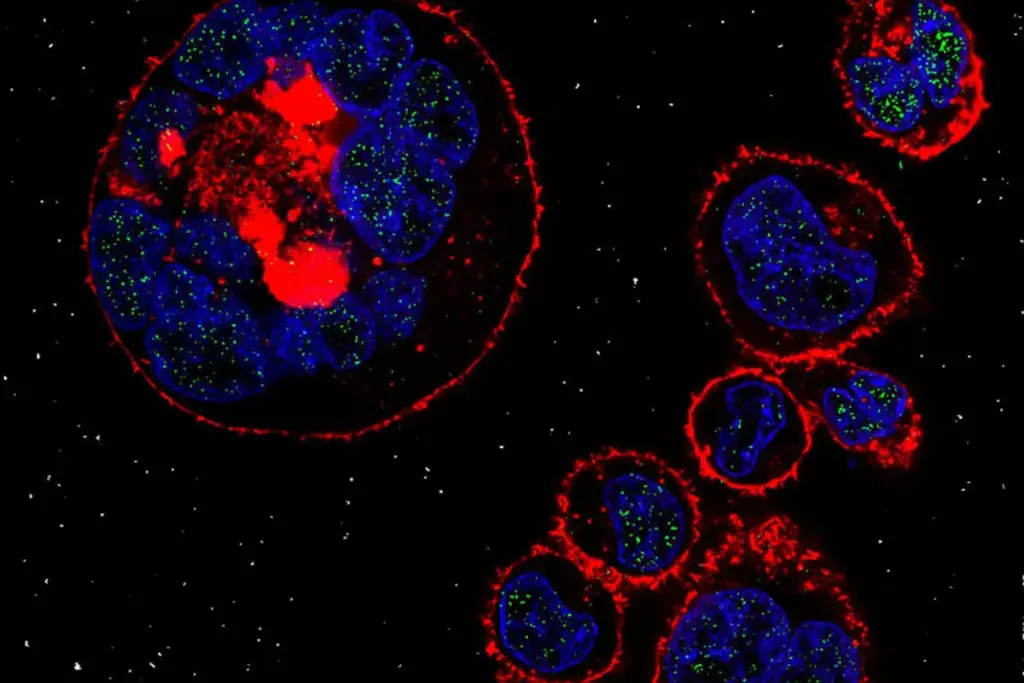
Chimerism Analysis: Regular DNA tests are performed to ensure the new marrow is 100% donor-derived (complete chimerism). A drop in donor cells might signal rejection, prompting immediate intervention with donor lymphocyte infusions.

Endocrine Restoration: Many Thalassemia patients have pre-existing damage to their endocrine glands from iron. After transplant, careful monitoring of thyroid function, bone density, and puberty hormones is essential. In some cases, reversing the iron overload can improve hormonal function; in others, lifelong hormone replacement may be needed.

The shift from “patient” to “survivor” is significant.
Freedom from Chelation: The cessation of nightly chelation therapy is often described as the most liberating aspect of the cure, drastically improving the quality of life for the entire family.

Lifetime: Even cured patients should have an annual check-up with a hematologist familiar with their history to monitor for late effects.
Send us all your questions or requests, and our expert team will assist you.
Thalassemia patients often have a bronze or greyish skin tone due to iron overload and melanin stimulation. After a successful transplant and the subsequent removal of excess iron (through phlebotomy), the skin typically returns to an everyday, healthy shade as iron stores are depleted.
Immunosuppressive drugs (anti-rejection medicine) are typically tapered off and stopped between 6 months and 1 year after the transplant, provided there is no active Graft-Versus-Host Disease. Once these are stopped, the patient is often medication-free, except perhaps for vitamins or hormone supplements if needed.
Fertility depends on the chemotherapy drugs used during conditioning and the patient’s pre-transplant iron damage. Many cured patients do go on to have natural pregnancies. Fertility preservation (sperm/egg banking) is discussed before transplant. Post-transplant fertility assessments are part of long-term follow-up.
Yes. Once the donor stem cells have fully engrafted and the immune system has adapted (tolerance), the cure is considered permanent. The patient’s bone marrow will produce healthy red blood cells for the rest of their life. Relapse (graft rejection) is rare after the first year.
Phlebotomy is the process of drawing blood, similar to donating blood. In patients with cured Thalassemia, it is used to remove excess iron. By removing blood, the body is forced to use the iron stored in the liver and heart to make new blood cells, effectively clearing the organs of excess iron.





Did you know that nearly 70% of patients who get a stem cell transplant notice unusual smells during recovery? This can be confusing and upsetting

