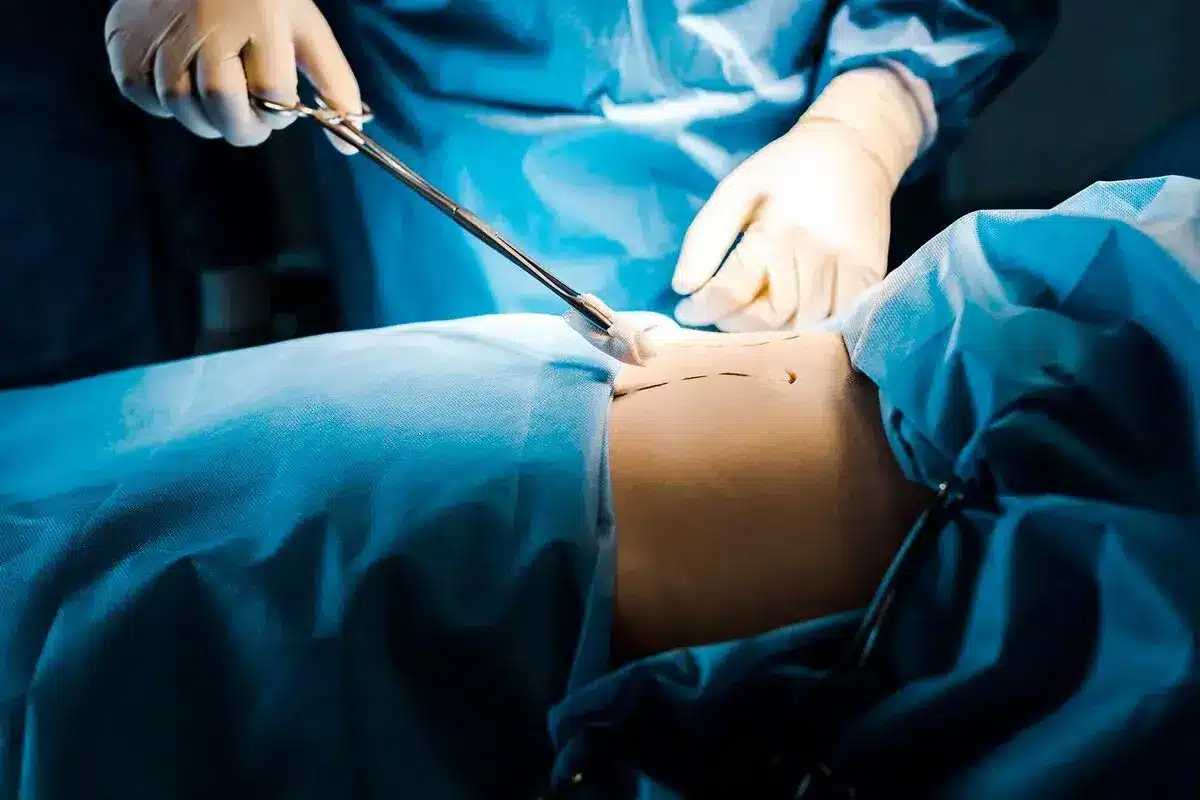
Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
Reconstructive surgery is a specialized field focused on restoring both the shape and function of the body. Unlike cosmetic surgery, which aims to improve normal features, reconstructive surgery fixes problems caused by birth defects, injuries, infections, tumors, or disease. Its main goal is to return the body to normal and improve the patient’s quality of life.
Surgeons see reconstructive surgery as a way to help patients move from having a physical problem to regaining normal body function. It’s more than just closing a wound; it’s about restoring how different tissues work together. When reconstruction is successful, patients can use their bodies more easily, like picking up objects, walking comfortably, or speaking clearly.

The best reconstructive surgeries combine careful surgical technique with a sense of artistry. While fixing function is the main goal, how the result looks is also very important. For example, a rebuilt nose needs to work well for breathing, but it should also look natural so the patient feels confident.
Modern surgical methods focus on the idea that how something works should guide how it looks. Surgeons use tissues that match the area in color, texture, and thickness, and follow the body’s natural lines. This approach helps the repair work well and blend in with the patient’s own body.

Microsurgery is a key part of modern reconstruction. It lets surgeons move tissue from one area of the body to another. In this technique, a piece of tissue with its blood supply is carefully removed and then reconnected to blood vessels at the new site using a microscope.
This method is important for fixing large wounds that can’t be closed with nearby tissue alone. It’s often used after injuries, cancer surgery, or severe burns. Restoring blood flow to the moved tissue helps it survive and work well in its new place.
Tissue expansion is a method that uses the body’s ability to grow new skin when stretched. A balloon-like expander is placed under healthy skin next to the area that needs repair. Over several weeks or months, the expander is slowly filled with salt water.
This process slowly stretches the skin, causing it to grow more cells and blood vessels. When there is enough new skin, a second surgery removes the expander and uses the new skin to cover the wound. This is helpful because the new skin matches the area around it in color and texture.

Local and regional flaps are ways to move healthy tissue, still connected to its blood supply, to cover a nearby wound. A local flap uses tissue right next to the wound, moving it into place. A regional flap takes tissue from a nearby area and sometimes moves it under the skin to reach the wound.
These methods are commonly used in reconstructive surgery. Since the tissue keeps its own blood supply, it is stronger than a skin graft and can cover important areas like exposed bone or tendon. Planning these flaps takes a strong knowledge of blood vessels and how tissues work.
Skin grafting is a basic method used when a wound is too big to close directly or with nearby tissue, but the area underneath is healthy. It involves taking a thin layer of skin from another part of the body, like the thigh, and placing it over the wound.
There are two main types of skin grafts: split-thickness, which includes the top layer and part of the deeper layer of skin, and full-thickness, which includes all layers. Split-thickness grafts are often stretched to cover bigger areas. Full-thickness grafts are used for important areas like the face or hands, where appearance and less shrinking matter most.
Surgeons use a step-by-step approach called the reconstructive ladder to decide how to fix a wound. This method helps them choose the simplest and least invasive way that will work. The ladder starts with letting the wound heal on its own, then moves to direct closure, skin grafts, local flaps, and finally moving tissue from another part of the body.
Today, surgeons sometimes use what’s called the reconstructive elevator, meaning they can skip steps to get a better result for the patient. The main idea is to pick the best method for each person’s needs and long-term goals, not just the simplest option.
Regenerative medicine is now often used in reconstructive surgery. It uses natural materials and the patient’s own cells to help healing and grow new tissue. For example, fat grafting adds volume and brings in stem cells that can make the skin and scars look and feel better.
Acellular dermal matrices (ADMs) are another helpful tool. They act as a framework for the patient’s own cells to grow and form new blood vessels. These advances help surgeons strengthen repairs, cover soft tissue better, and avoid taking large amounts of tissue from other areas.
Reconstructive surgery for children treats birth defects that affect how they grow and function. Timing is very important, and surgeries are often planned around key growth stages or social milestones. The aim is to fix the problem while letting the child’s bones and tissues grow naturally.
Surgeons consider that children’s skin is very stretchy and heals quickly. Surgeries like cleft lip and palate repair, ear reconstruction, and hand surgery are designed to give the best early results and reduce the need for more surgeries later.
Reconstruction is an important part of cancer care. It helps patients recover from the effects of cancer surgery. Whether rebuilding a breast after mastectomy or fixing a jaw after cancer removal, reconstructive surgeons work closely with cancer doctors to make sure the treatment is safe and effective.
Often, reconstruction is done right away to save skin and help with emotional recovery. Sometimes, though, it needs to be delayed if the patient will have radiation or strong chemotherapy. The plan is always tailored to each patient’s cancer treatment and outlook.
Every reconstructive surgery starts with a careful check of the patient’s body. Surgeons look for healthy tissue that can be used, check the blood vessels, and examine the skin’s quality. They also identify “angiosomes,” which are areas of tissue supplied by one main artery.
This evaluation helps decide if a patient needs a complex tissue transfer or a simpler method. Things like past surgeries, damage from radiation, and smoking history all affect which procedures are possible.
Reconstructive surgery does more than fix the body. For people with visible differences or physical limits, it can help them regain confidence and independence. It lets them get back to daily life, work, and social activities without being held back by their condition.
This process often helps people move past a difficult time in their lives. Whether they are healing from an injury or illness, getting their body back can also help them heal emotionally. Surgeons focus on educating and supporting patients to set realistic expectations and encourage a positive attitude during recovery.

Send us all your questions or requests, and our expert team will assist you.
Reconstructive surgery is performed to correct abnormal structures of the body caused by congenital disabilities, developmental abnormalities, trauma, infection, tumors, or disease. Health insurance policies generally cover it. Cosmetic surgery is performed to reshape typical body structures to improve appearance and self-esteem, and is usually not covered by insurance.
Yes, reconstructive surgery is typically considered medically necessary because it aims to restore function or correct a physical abnormality. However, the definition of medical necessity can vary by insurance provider, and pre-authorization is often required to confirm coverage based on specific medical criteria.
A flap is a unit of tissue that is transferred from one part of the body to another while maintaining its own blood supply. This is different from a graft, which is completely detached. Flaps can carry skin, fat, muscle, and even bone to repair complex defects.
The duration varies wildly depending on the complexity. A simple skin graft might take one hour, while a complex microsurgical free flap reconstruction for head and neck cancer can take 8 to 12 hours. Your surgeon will provide a specific time estimate based on your surgical plan.
Yes, all surgeries involving incisions leave scars. However, reconstructive surgeons are experts in scar management. They place incisions in natural skin lines whenever possible and use advanced closure techniques to ensure the resulting scars are as delicate and inconspicuous as possible.







Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)