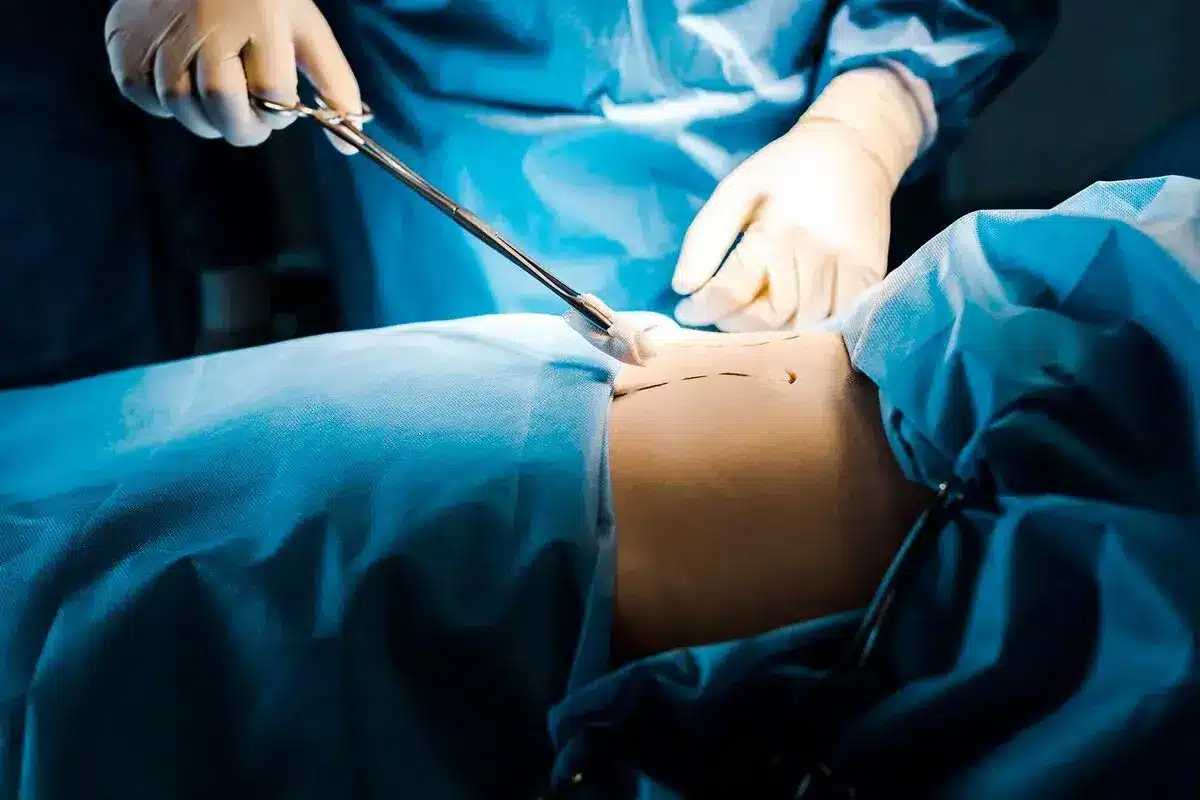
Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The initial consultation serves as the foundation for the entire reconstructive journey. It is a comprehensive medical evaluation where the surgeon assesses the patient’s specific defect, medical history, and functional goals. This phase is diagnostic, aiming to identify the root cause of the deformity and the biological constraints of the patient’s tissues.
During this meeting, the surgeon evaluates the blood supply, skin quality, and available donor sites. It is a collaborative session in which the patient’s desires are mapped against surgical options. The surgeon focuses on educating the patient about the diagnosis to ensure informed decision-making.

Modern reconstructive surgery utilizes advanced imaging technology to bridge the gap between medical terminology and patient understanding. 3D simulation tools enable surgeons to capture high-resolution images of the patient’s anatomy and digitally manipulate them to visualize potential outcomes.
For procedures like breast reconstruction or craniofacial repair, these simulations are invaluable. They allow patients to visualize volume changes, symmetry adjustments, and contour improvements. While not a guarantee, these digital maps provide a realistic visual goal and help align patient and surgeon expectations.

Assessing the biomechanical properties of the skin is critical for planning incisions and flaps. The surgeon evaluates skin elasticity, recoil, and thickness to determine how well the tissue will withstand movement or stretching. This is particularly important for local flaps and tissue expansion.
The “pinch test” and other manual assessments help the surgeon gauge laxity. Skin that is too tight may require a skin graft or distant flap, while skin with good elasticity may allow for primary closure. This assessment dictates the surgical technique used to close the wound without excessive tension.
In abdominal, chest, and limb reconstruction, the integrity of the underlying muscle is paramount. The surgeon palpates the muscles to assess for separation, atrophy, or denervation. Dynamic testing, where the patient contracts specific muscle groups, helps identify weakness or hernias.
For abdominal wall reconstruction, staging the width of the diastasis recti or the size of the hernia defect is essential. This determines whether a simple suture repair is sufficient or if component separation and mesh reinforcement will be required to achieve a durable closure.

Surgical readiness involves optimizing the patient’s physiology to withstand the stress of surgery and healing. This includes ensuring that chronic conditions like diabetes and hypertension are under strict control. High blood sugar levels, for instance, can severely impair wound healing and increase the risk of infection.
Nutritional status is also evaluated. Patients must have adequate protein stores to build new tissue. The surgeon checks for anemia and clotting disorders to prevent intraoperative complications. This holistic review ensures the patient is physically capable of a safe recovery.
For body contouring and abdominal reconstruction, weight stability is a non-negotiable prerequisite. Patients are generally required to be at a stable weight for at least six to twelve months before surgery. Fluctuations in weight can alter the surgical plan and compromise the long-term results.
Operating on a patient who is actively losing weight can result in recurrent skin laxity. Conversely, gaining weight after surgery can stress the repair and lead to recurrence of hernias or diastasis. Stability ensures that the tissue envelope is in a steady state for reconstruction.
Nicotine is a potent vasoconstrictor that significantly impairs microcirculation. In reconstructive surgery, which relies on the survival of moved tissue (flaps) and the healing of incision lines, adequate blood flow is critical. Nicotine use drastically increases the risk of tissue necrosis, wound infection, and flap failure.
Surgeons enforce a strict nicotine cessation protocol, typically requiring patients to stop all nicotine products (including vapes and patches) for at least 4 to 6 weeks before and after surgery. Compliance is often verified through urine cotinine tests to ensure patient safety.
Nicotine is a potent vasoconstrictor that significantly impairs microcirculation. In reconstructive surgery, which relies on the survival of moved tissue (flaps) and the healing of incision lines, adequate blood flow is critical. Nicotine use drastically increases the risk of tissue necrosis, wound infection, and flap failure.
Surgeons enforce a strict nicotine cessation protocol, typically requiring patients to stop all nicotine products (including vapes and patches) for at least 4 to 6 weeks before and after surgery. Compliance is often verified through urine cotinine tests to ensure patient safety.
Beyond standard photographs, complex reconstructions often require advanced radiological imaging. CT scans or MRIs are used to map perforator blood vessels for free flaps, assess bone stock for craniofacial repair, or define the anatomy of a complex hernia.
This “roadmap” allows the surgeon to plan the operation with high precision, identifying the best blood vessels to use and avoiding critical structures. It minimizes operative time and exploratory dissection, resulting in safer, more predictable surgeries.
A thorough review of the patient’s medication list is conducted to prevent drug interactions and bleeding risks. Blood-thinning medications, anti-inflammatories, and certain herbal supplements must be paused before surgery to minimize the risk of hematoma.
Conversely, some medications may need to be adjusted or bridged. The surgical team coordinates with the patient’s prescribing physicians to manage these changes safely, ensuring that underlying health conditions remain stable throughout the perioperative period.
If the reconstruction involves a graft or flap, the donor site must be carefully selected and planned. The surgeon evaluates potential sites based on tissue quality, color match, and the ability to hide the resulting scar. The functional impact of taking tissue from the donor area is also considered.
The consultation includes a discussion about the donor site scar and any potential temporary weakness or sensory changes in that area. This ensures the patient understands that reconstruction often involves creating a second surgical site to repair the first.

Send us all your questions or requests, and our expert team will assist you.
You must stop smoking and using all nicotine products for at least 4 to 6 weeks before surgery and continue for the same period afterward. Nicotine shrinks blood vessels, which can cause the reconstructed tissue to die and wounds to fall open.
For most reconstructive surgeries, autologous blood donation is not necessary. However, for extensive procedures involving significant blood loss, your surgeon might discuss this option or ensure that blood is available if needed. We optimize your blood counts beforehand to minimize this risk.
If you develop a cold, flu, or any infection in the week leading up to surgery, you must notify your surgeon immediately. Elective surgeries are often rescheduled to ensure your body is not fighting a disease, which could compromise anesthesia safety and healing.
It is helpful to be close to your goal weight, but you don’t need to be perfect for the consultation. The consultation is the time to discuss your goals and create a timeline. However, achieving a healthy BMI before the scheduled surgery significantly reduces the risk of complications.
Even if the surgery involves soft tissue, a CT angiogram allows the surgeon to “see” the blood vessels under your skin. This map helps them identify the best arteries to supply blood to the reconstructed tissue, making the surgery safer and faster.







Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)